-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Q. Which organs have TSH receptors and hence are affected by TSH receptor antibodies in Graves’ disease?
- Thyroid
- Fibroblasts – including orbital fibroblasts
- Adipocytes – including orbital adipocytes
- Bone cells
-
Q. What is the histopathological feature in Graves’ disease?
- Patchy lymphocytic infiltration
- Follicular hyperplasia
- Reduction of follicular colloid
-
Q. What is the nature of the lymphocytes?
- They are mainly T cells
- Some B cells may be present
-
Q. Which antibody is associated with Graves’ disease?
- TRAb
- TSH receptor antibody – which is stimulating TSI (TSI- TRAb)
- TRAb
-
Q. What is the class of TRAb?
- It is an IgG1 antibody
- It is oligoclonal, unlike TPO and Anti Tg, which are polyclonal
-
Q. Does TRAb values help in the follow-up of a patient on ATD treatment?
- Yes it does
- At the time of discontinuation of ATD if TRAb is high- chances of recurrence are hight
-
Q. What happens to TRAb after radioactive iodine therapy?
- Transient increase of TRAb- that’s why orbitopathy worsens
- It normalizes in 3-5 months
- Then slowly declines over years
-
Q. What happens to TRAb after thyroid surgery?
- The rapid decline in levels are seen
- By 18 months- 80% of TRAb disappear after surgery
-
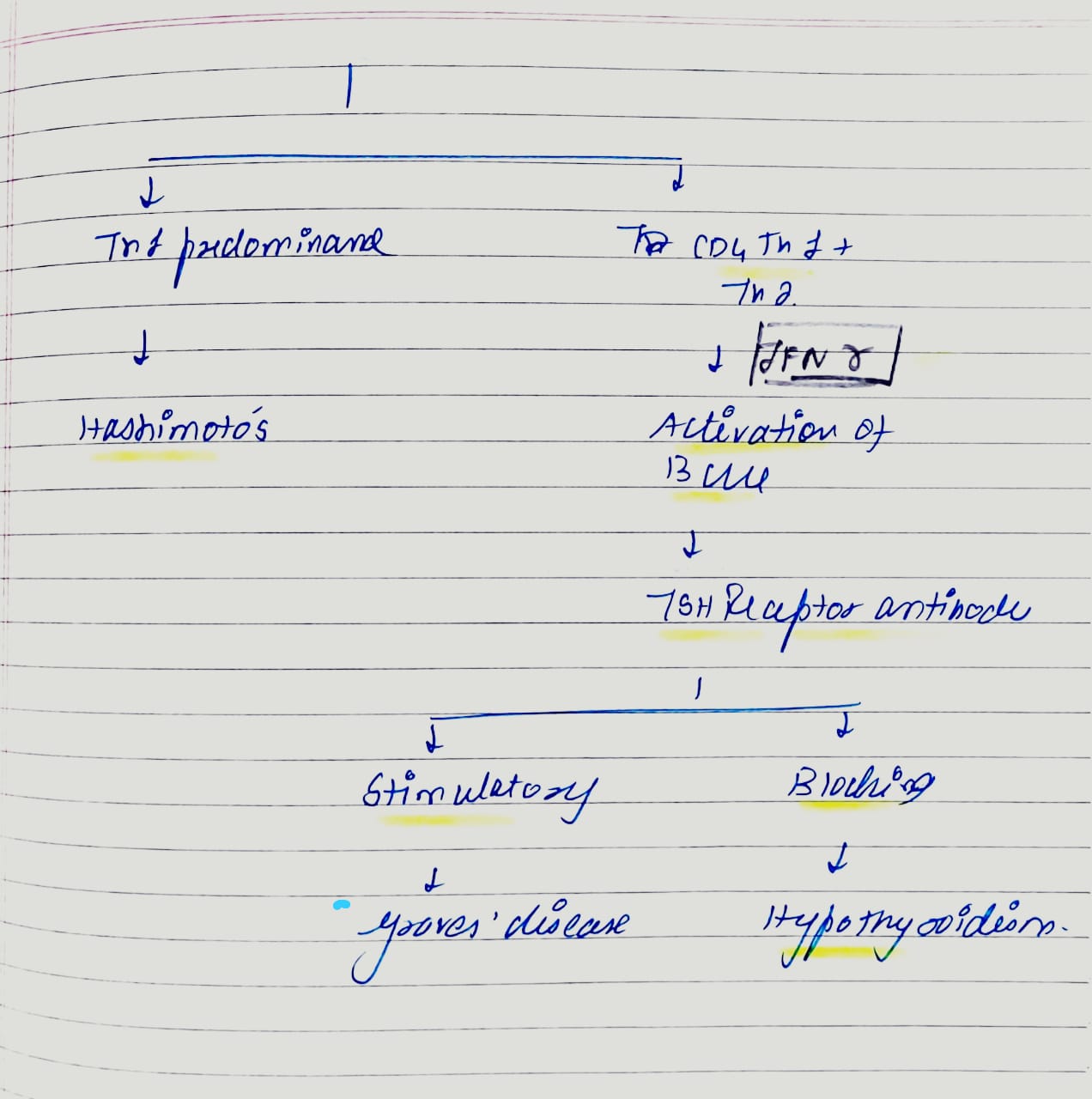
Q. What are the types of TRAb antibodies?
- Stimulating
- Blocking
- Neutral
-
Q. What subtype of TRAb is seen in Graves’ disease?
- A mixture of stimulating and blocking antibody- mainly stimulating antibody
-
Q. Which are the specific T cells which are pathogenic in Graves’?
- CD4+ Th1 cells – predominate
- They produce IL2, TNF alpha, and Interferon-gamma
- They activate CD8 T cell
- CD4 Th2 are also present
- Graves is a mixture of CD4 Th1 + Th2
- Hashimoto’s is a predominantly Th1 disease
-
Q. Which of these cytokines increases the production of TRAb antibodies?
- Interferon-gamma is the main culprit here
-
Q. Which are the costimulatory molecule for T Cell activation by APC in Graves, and which is it in type 1 diabetes?
- Type 1 diabetes- costimulatory molecules are CD28 interacting with CD80 and 86
- In Graves', it is CD40
-
Q. Why does Graves’ disease become milder in pregnancy?
- Because of the increase of Treg – regulatory T cells
-
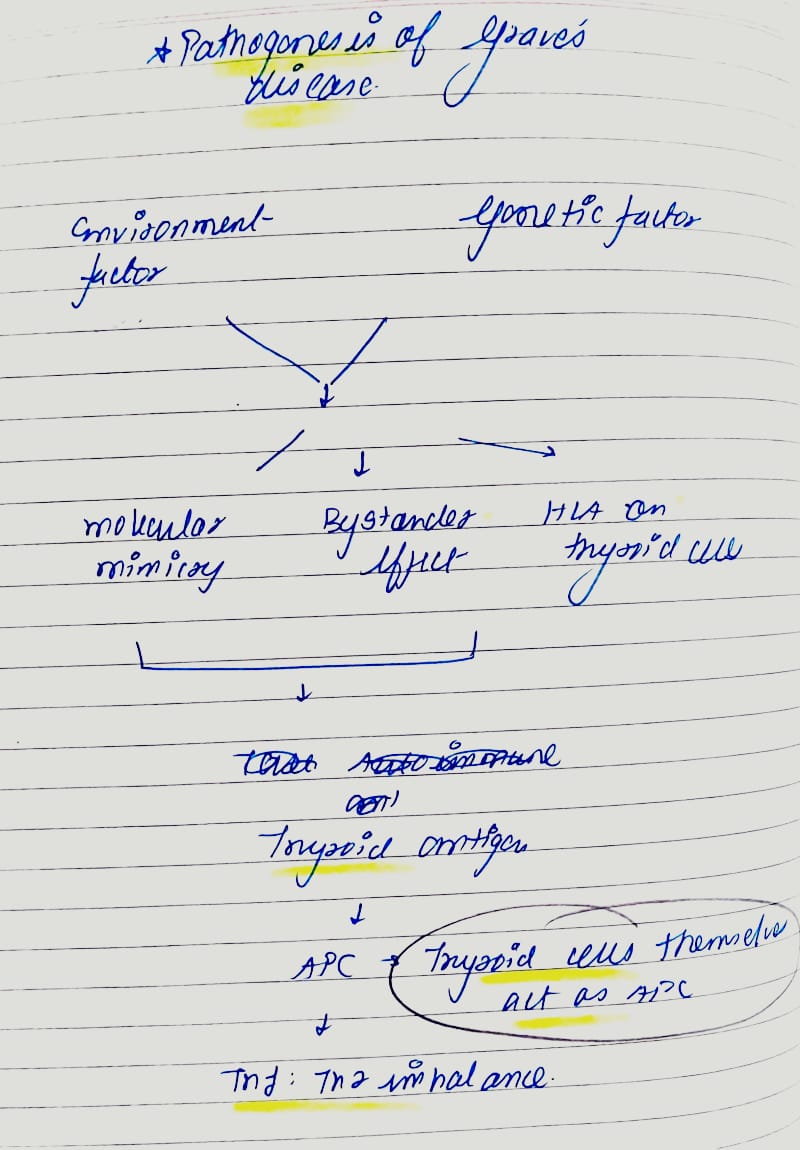
Q. Which are the possible immune mechanisms which activate the autoimmunity in Graves’?
- Three possible problems:
- Molecular mimicry – bacterial heat shock protein, Yersinia, Retroviral sequences
- Thyroid cell HLA expression
- Bystander activation
- Three possible problems:
-
**Precipitating factors **
-
Q. Which HLA subtypes are associated with Graves’ disease?
- HLA-DR8 is associated
- However, the association is weak, and hence typing is not useful
-
Q. Can infections predispose to thyroid autoimmune disease?
- Yes
- Some have been implicated, like retrovirus and hepatitis C
- However, none have been proven
-
Q. Can stress precipitate Graves’?
- Yes
- Stress increase cortisol → suppression of immunity → rebound hyperimmune response once cortisol is relived
-
Q. Why do females have more Graves’ disease?
- It is not exactly known
- However, the moderate amount of estrogen stimulate autoimmunity – neither high nor low amounts
-
Q. What is the relation of pregnancy with graves’?
- Graves’ becomes milder in pregnancy
- However, many new cases of Graves are precipitated in the postpartum period
- The presence of fetal cells in the mother may be responsible- this is called Fetal microchimerism
-
Q. Which drugs can precipitate Graves’ disease?
- Iodine
- Amiodarone
- Almetezumab used in Multiple sclerosis
- Interferon alpha- used in hepatitis C
-
Q. Summarize the precipitating factors which can predispose to graves’ disease?
- HLA subtypes and genes- HLA DR8
- Female sex – moderate estrogen influence
- Postpartum status – Fetal micromimicry
- Infection- Yersinia, Retrovirus, hepatitis C
- Drugs
- Smoking
- Stress
-
Q. Summarize the pathogenesis of Graves’ disease?
Please consider donating to "Notes in Endocrinology" to keep us going. Please visit our DONATION page to know more