- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
- Abbreviations
- GO = Graves' orbitopathy
- TAO= Thyroid associated orbitopathy
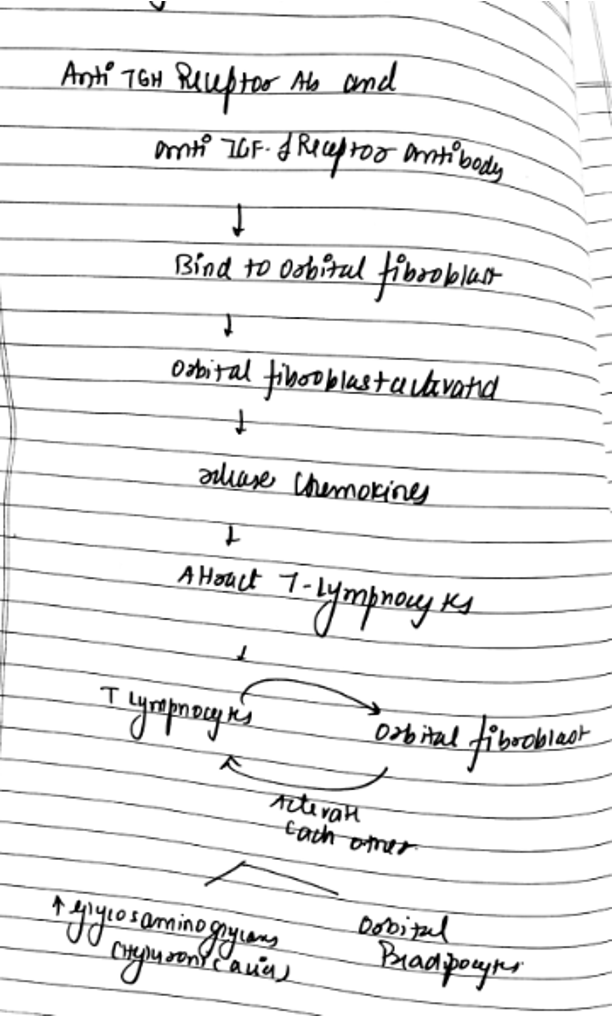
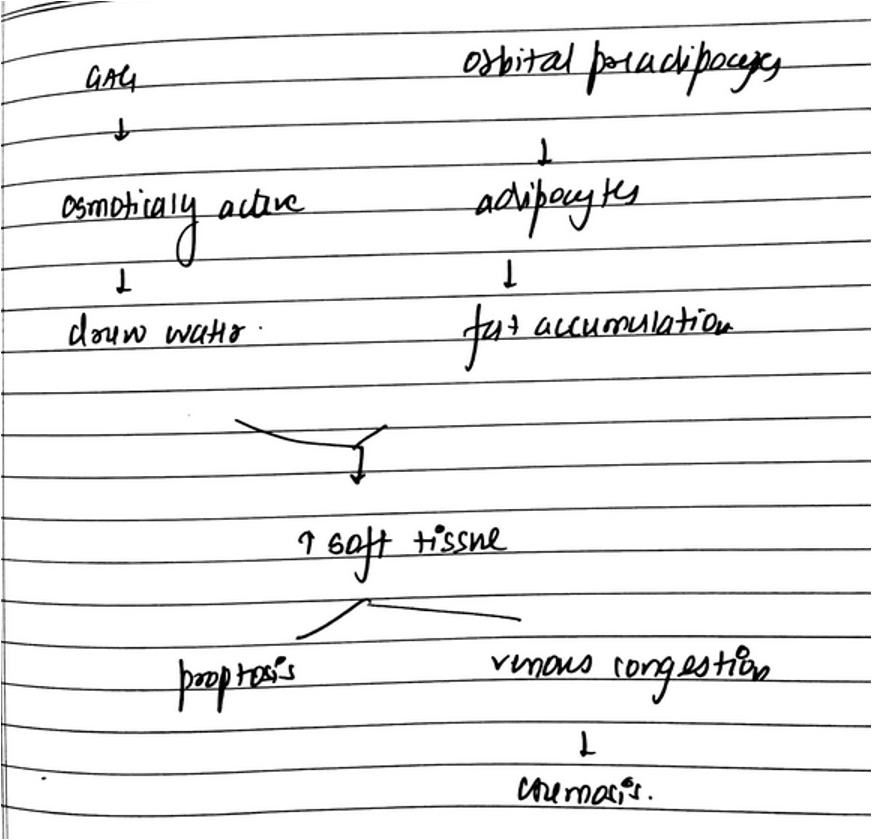
- Q. Describe the pathogenesis of GO ?
- **Epidemiology **
- Sex
- It is more common in females
- It is more severe in males
- Age
- More common in 40-60 years of age
- More severe in elderly
- Sex
- **RISK FACTORS **
- Q. What are the risk factors for GO ?
- Age- older the age- worse the disease
- Sex- more severe in males
- TSH Receptor antibody- higher the titer- more severe the disease
- Radioactive iodine therapy – may worsen the disease
- Smoking – worsening of the disease
-
**ASSOCIATION WITH THYROID DISORDER **
-
Association with Grave's disease
- 20-25% with Grave's disease have overt TAO
- 30-40% of patients with Grave's disease may have changes on CT Scan or ultrasound but no overt disease
- Timing with Grave's
- 20% - Precedes hyperthyroidism
- 40%- diagnosed concurrently
- 20%- Follows the diagnosis of hyperthyroidism
- 20%- Occurs after Radioactive iodine therapy
- With patients having TAO
- 80%- Hyperthyroid
- 10-20%- Euthyroid
- 1-10%- Hypothyroid
- Q. What are the symptoms of GO ?
- Proptosis
- Watering and redness of eyes
- Photophobia
- Diplopia
- Retro-orbital pain
- Pain on movement of eyeballs
- Loss of color vision
- Vision loss
-
**SIGNS **
-
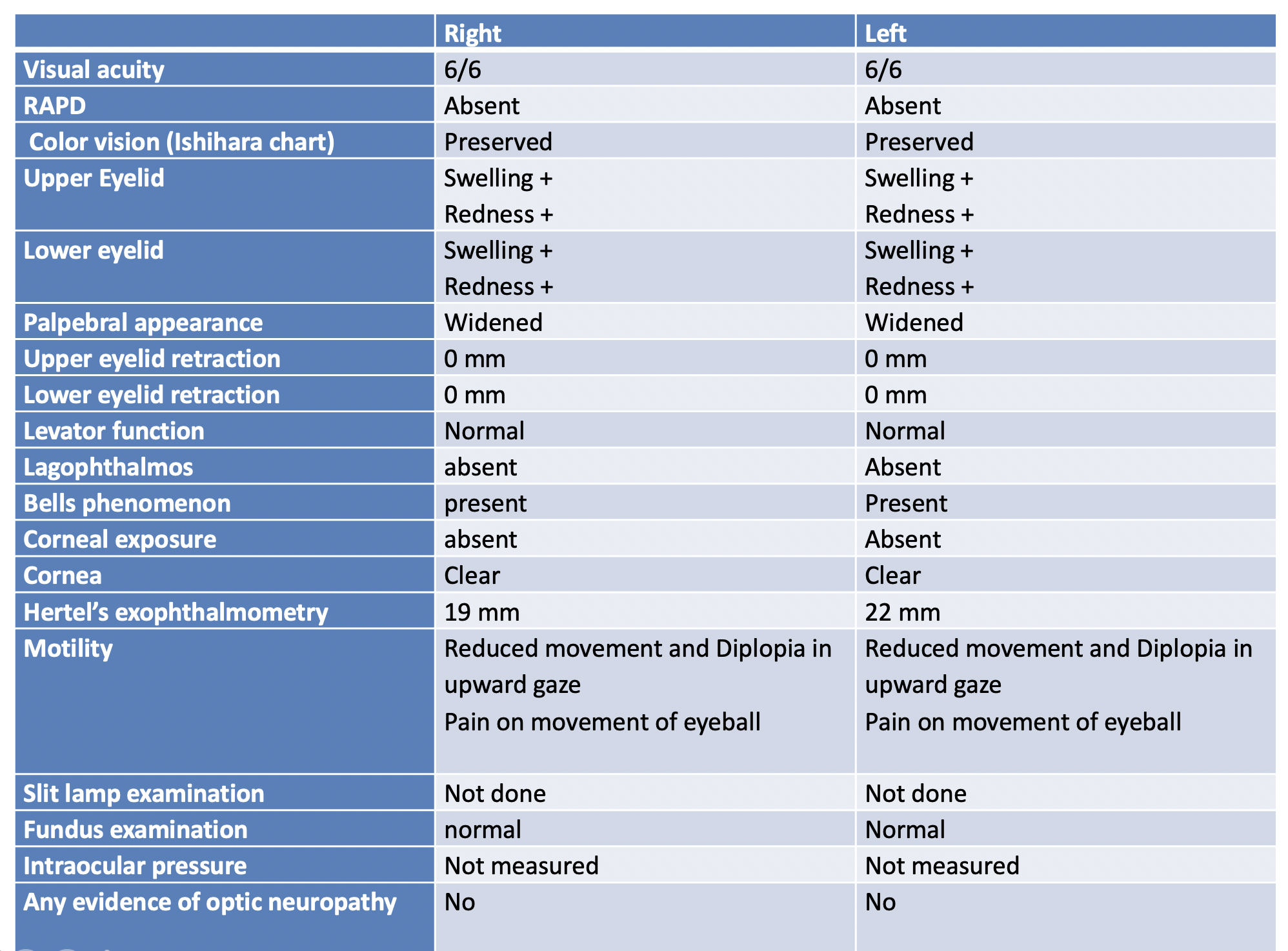
Q. Enlist the signs to look for in a patient with GO ?
- Here is a sample clinical examination sheet enlisting the signs of GO
- Here is a sample clinical examination sheet enlisting the signs of GO
- Q. What are the clinical features of optic neuropathy in patients with Grave's ophthalmopathy?
- Loss of color vision
- Disc swelling or optic atrophy
- RAPD
- Loss of visual acuity
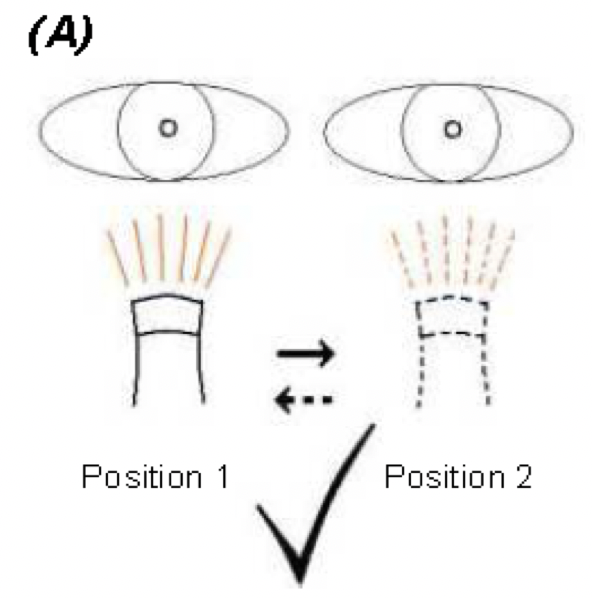
- Q. How to test for RAPD? (Marcus Gunn Pupil)
- Step 1
- Ask the patient to fixate in the distance
- Ask him to hold the light source for 3 seconds in that position
- Assess the degree of contraction and how long it sustains.
- Step 2
- Now Move the light source to position 2 shown below. and hold for 3 seconds.
- Assess the degree of contraction and how long it sustains.
- Compare with what you remember from the other eye.
- Step 3
- Move light source back to position 1 and hold for 3 seconds. Assess the degree of contraction and how long it sustains.
- Compare with what you remember from the other eye.
- Step 4
- Repeat the swing from side to side until you are sure whether one side contracts less or sustains for less time (+ RAPD), or whether the pupil reflexes are equal in these respects (-RAPD).
- Step 1
- Q. What is RAPD suggest?
- The presence of RAPD suggests compression of the optic nerve (proximal to the chiasma)
- Q. How is the retraction of eyelid measured?
- Normally the upper eyelid covers the sclero-corneal junction by 1-2 mm.
- If the sclera is visible above the sclero-corneal junction – then there is at least 1.5 mm retraction and suggests upper eyelid retraction.
- Eyelid retraction >1-2 mm is significant.
- Q. What is the importance of upper eyelid retraction?
- It is mainly due to sympathetic overactivity. It can be present in other causes of thyrotoxicosis other than Graves. It is one of the early signs of eye involvement.
- Q. Which other autoimmune diseases must be looked for while dealing with GOc?
- Look for Ptosis, which may be associated with Myasthenia gravis.
- Q. What distance is measured by Hertel's exompthalmometer?
- Between the lateral canthus of the eye and the orbital apex.
- Q. What is the normal distance here?
- Normal is 20 mm in whites and 22 mm in blacks.
- Q. How is the Bells phenomenon assessed?
- Bells phenomenon is the rotation of the eyeball on the closure of the eyelid
- Examiner holds the patient's eyelid tightly and asks her to attempt to close the eyes
- The eyelid doesn't close, but the eyeball rotates upward
- This is a normal bells phenomenon
- Absent bells phenomenon is seen in 10 % of patients
- They have a higher risk of corneal ulceration of eyelid doesn't close properly.
- Q. What is Lagophthalmos ?
- Lagophthalmos is defined as the inability to close the eyelids completely.
- Ask the patient to look down and gently close both eyes.
- Lagophthalmos is present when space remains between the upper and lower eyelid margins in extreme downgaze.
- Document the degree of lagophthalmos by measuring this space, in millimeters, with a ruler.
- Also, record the blink rate as well as the completeness of the blink.
- CLASSICAL THYROID EYE SIGNS
- Q. Enlist the classical thyroid eye signs?
- Dalrymple's sign – lid retraction- gives the patient a staring look
- Von Gaffes' sign – lid lag in downgaze- ask the patient to look downwards- the upper lid lags behind the globe, exposing the sclera between the limbus and the eyelid
- Stellway's sign- infrequent blinking and incomplete blinking + proptosis
- Rosenbach's sign- the fine tremor of the eyelid on closure- esp the upper eyelid
- Mobius sign- failure of convergence of eyes on accommodation
- Kocher's sign- the reverse of von-grafe- on upward gaze the upper eyelid retract quickly
- Joffroy's sign- absent wrinkling of the forehead when the eyes are looked up
- Other lesser common
- Saiton's sign- on looking upwards, the frontalis muscle contracts after the upper eyelid is fully retracted
- Jellinek's sign- brownish pigmentation of upper-eyelid
- Topolansky's sign- pericorneal congestion in patients with Graves disease
- Q. Which is the earliest sign to appear?
- Lid retraction Dalrymple's sign
- Normally upper eyelid covers the iris by >1 mm – it <1 mm or sclera see above the limbus – this sign is present
- The upper sclera is seen- due to eyelid retraction
- The lower sclera is seen- due to exophthalmos
-Q. What is Gifford's sign?
- Unilateral exophthalmos has to be differentiated from thyroid involvement vs. orbital tumor
- Retract the eyelid of the patient
- In Orbital tumor- you would be able to do so
- In exophthalmos due to thyroid- it is not possible
- **Assessment of severity **
- Q. What is NO SPECS classification of severity of GO ? – also called the ATA classification
- NO SPECS CLASSIFICATION OF WERNER
- Class 0- No signs of Symptoms
- 1- Only Signs present but no symptoms
- 2- Soft tissue involvement
- 3- Proptosis
- 4- Extraocular muscle involvement
- 5- Corneal involvement
- 6- Sight loss
- NO SPECS CLASSIFICATION OF WERNER
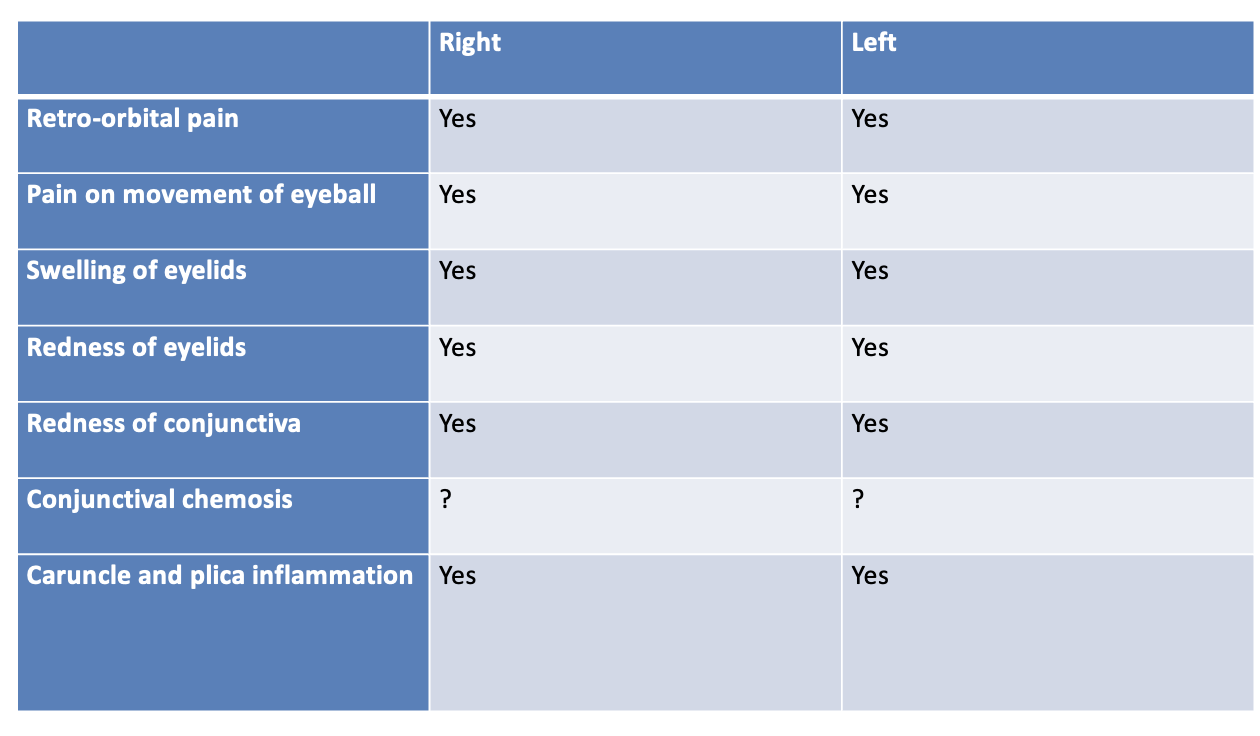
- Q. Describe the EUGOGO clinical activity score?
- EUGOGO Clinical activity score
- Here is a sample clinical assesment sheet for EUGOGO clinical activity
- Score > 3 /7 is suggestive of active ophthalmopathy
- Q. Which are additional points in EUGOGO on follow-up?
- 3 more points for follow up
- Reduce in visual acuity by 1 on Snellen chart
- More than 2mm increase of proptosis
- More than 8-degree reduction in eyeball movement in one direction
- Plus the usual 7 points taking total to 10 points
- Score >4/10 on follow up is suggestive of active GO
- 3 more points for follow up
- Q. What is the EUGOGO classification for the severity of GO ?
- Mild
- Moderate to severe
- Sight threatening
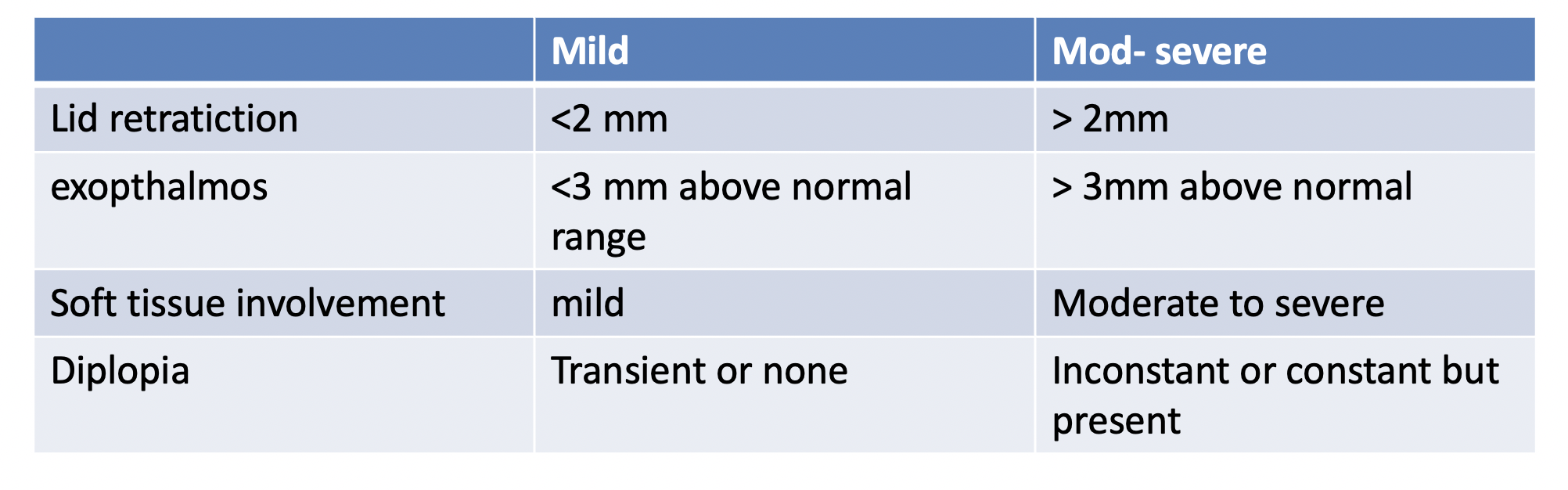
- Q. Describe the Mild vs Moderate to severe in EUGOGO severity classification
- Q. When is it considered sight threatening ?
- Sight threatening
- Also called DON- Dysthyroid optic neuropathy
- Optic neuropathy present
- Sight threatening corneal exposure
- Globe subluxation
- Sight threatening
- Q. What is the VISA classification?
- It is developed by the International Thyroid Eye Disease Society (ITEDS)
- It has 4 parameters
- V- vision
- I- inflammation and congestion
- S- strabismus and eyeball movement
- A- Appearance/ exposure
- **Diagnosis **
- Q. Which are the tests that you will order for a patient with GO ?
- Blood tests
- Thyroid function test
- TSH Receptor antibody
- Imaging – CT Scan Preferred
- Q. What is the classical CT scan picture of the patient with Grave's ophthalmopathy?
-
- Proptosis
-
- Thickening of extraocular muscles with sparing of the tendinous insertion
-
- Muscle diameter > 4 mm
-
- **DIFFERENTIAL DIAGNOSIS **
- Q. What is the differential diagnosis of bilateral exophthalmos?
- Cushing's syndrome
- Obesity
- Super vena cava syndrome
- Q. What is the Differentials of unilateral exophthalmos?
- Carotid- cavernous fistula
- Orbital neoplasm
- Infiltrative eye disease
- Cavernous sinus thrombosis
- Pseudotumor of orbit
- **COMPLICATIONS **
- Q. What are the causes of vision loss in GO ?
-
- Extreme proptosis leading subluxation of the globe
-
- Severe corneal ulceration
-
- Optic nerve involvement
-
- **NATURAL HISTORY **
- Q. What is the Natural history of GO ?
- 66%- Remains same
- 8-10%- Worsens
- 20 % - Improves spontaneously
- IMPACT OF TREATMENT OF HYPERTHYROIDISM
- Q. What is the impact of treatment of Hyperthyroidism on GO ?
- Impact of surgery and anti-thyroid drugs
- Little impact on TAO severity
- Hypothyroidism must be avoided- hypothyroidism will worsen the TAO
- Radioactive iodine
- Can potentially worsen the Ophthalmopathy
- It can also lead to new onset of clinical GO, which was not present or noticed earlier
- Impact of surgery and anti-thyroid drugs