-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Q. What is the definition of a thyroid nodule?
- A thyroid nodule is a discrete lesion in the thyroid gland which is radiologically distinct from surrounding tissues
-
Q. Broadly, Thyroid nodules of which size are evaluated?
- All thyroid nodules>1 cm – evaluate
- Selected thyroid nodules <1 cm – evaluate
-
Q. Should family members of patients with thyroid cancer (non-medullary) be screened for thyroid nodules?
- No recommendation by ATA 2015
- 5-10% of cases of DTC are familial
- Ultrasound screening may lead to early diagnosis. However, is no evidence that it will improve morbidity or mortality
-
Q. Thyroid nodules are more common in men or women?
- More in women
-
Q. How common is malignancy in thyroid nodules?
- 5% of thyroid nodules are malignant
-
Q. How common are thyroid nodules in India?
- 9.6% by ultrasound
- 1.6% by palpation
-
Q. Prevalence of malignancy in thyroid nodule is higher in which group of patients?
- Children
- Men
- Age >60 years or <30 years
- History of head and neck irradiation
- Family history of thyroid cancer
-
Q. Multinodular goiters have a higher risk of thyroid malignancy, True or false?
- False
- They have a lower risk of thyroid malignancy
-
History and physical examination
-
Q. Are history and physical examination accurate for evaluation of thyroid nodule?
- No
- It carries low sensitivity and specificity for predicting malignancy in a thyroid nodule
-
Q. Which points in history suggest cancer in thyroid nodule?
- Rapid growth of the nodule
- History of head and neck irradiation in childhood
- History of total body irradiation for bone marrow transplant
- Family history of thyroid cancer- Cowden’s syndrome, MEN 2, FAP
-
Q. Which findings in physical examination give a possibility of thyroid cancer?
- Hard fixed mass on palpation
- Vocal chord paralysis
- Cervical lymphadenopathy
- Obstructive symptoms
-
Algorithm for evaluation of thyroid nodule
-
Q. Which have a higher risk of malignancy- Non-palpable nodule or palpable nodule?
- Both have an equal risk of malignancy
-
Q. Which is the most accurate way for assessment of thyroid nodule?
- FNAC
-
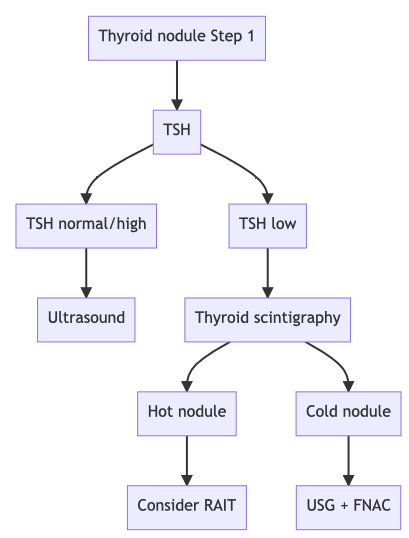
Q. Give the step-wise algorithm for evaluation of thyroid nodule?
-
Step 1
- Thyroid function test
- TSH- Normal / High → Go for Ultrasound
- TSH- low → thyroid scintigraphy
-
-
Step 2- TSH is normal or high or if you find a Cold nodule on scintigraphy- Use USG of thyroid for Risk categorization
- High risk of malignancy- More 70% risk
- Hypoechoic plus
- Microcalcification
- Incomplete halo
- Invading adjacent lymph node
- Extrathyroid extension
- Irregular margin
- Taller than wider
- Intermediate risk - 10-20% risk
- Hypoechoic with regular margin
- Low-risk risk 5-10%
- Hyperechoic with irregular margin
- isoechoic with a regular margin
- Partially cystic with an eccentric solid area
- Very low risk - <3%
- Spongiform
- Partially cystic with no suspicious features
- Likely Benign <1%
- Purely cystic
- High risk of malignancy- More 70% risk
-
Step 3a- FNAC Indications:
- High risk and intermediate-risk- Nodule >1 cm
- Low risk- >1.5 cm
- Very low risk - >2 cm
- Purely cystic- no need for FNAC
-
Step 3b - Follow-up
- If FNAC is not indicated- follow up with ultrasound
- High suspicion- repeat USG in 6-12 months
- Intermediate / low risk- rpt USG in 12- 24 months
- Very low suspicion >1 cm- repeat USG after 24 months
- Very low suspicion <1 cm – no need for repeat USG
-
Step 4- FNAC risk categorization- Bethesda method
- Non-diagnostic
- Benign
- FLUS- follicular lesions of unknown significance
- Follicular adenoma/carcinoma
- Suspicious of malignancy
- Confirmed malignancy
-
Step 5- Management based on Bethesda
- Bethesda 1- Non-diagnostic- Repeat FNAC
- If still, non-diagnostic consider lobectomy if high suspicious features present
- Else follow up
- Bethesda 2- Benign- Follow up with ultrasound
- High suspicion US pattern- repeat USG guide FNAC within 12 months
- Intermediate / low suspicion – repeat USG after 12-24 months. Repeat FNAC if :
- more 20% increase in size in 2 or more dimension
- more 50% increase in volume
- New suspicious features on ultrasound
- Very low suspicion on the US- no need to repeat FNAC – if required repeat after 24 months
- Two or more FNAC – suggestive of benign- no more follow up required
- Bethesda 3 and 4- FLUS/ AUS, Follicular adenoma
- Molecular marker
- Or Diagnostic lobectomy
- Bethesda 1- Non-diagnostic- Repeat FNAC
-
Bethesda 5 – Suspicious of malignancy
- Total thyroidectomy vs. diagnostic lobectomy vs. molecular marker
-
Bethesda 6- confirmed malignancy
- Thyroidectomy - Surgery
-
-
Q. What are the new ATA 2015 guidelines for follow-up of a lesion designated as benign on FNAC?
-
- High suspicion US pattern- repeat USG guide FNAC within 12 months
-
- Intermediate/low suspicion – repeat USG after 12-24 months. Repeat FNAC if :
- More 20% increase in size in 2 or more dimension
- More 50% increase in volume
- New suspicious features on ultrasound
-
- Very low suspicion on the US- no need to repeat FNAC – if required repeat after 24 months
-
- Two or more FNAC – suggestive of benign- no more follow up required
-
-
Q. What are ACUS and FLUS?
- ACUS- Atypical cells of undetermined significance
- FLUS- Follicular lesion of undetermined significance
-
Q. Where does molecular testing for thyroid nodule fall under the algorithm of a thyroid nodule?
- They are used in patients with ACUS or FLUS
-
Lab investigations
-
Q. Does the TSH level have any correlation with the risk of thyroid cancer?
- Higher the TSH – higher the risk of thyroid cancer
- “Serum TSH is an independent risk factor for predicting malignancy in a thyroid nodule. In a study of 1500 patients presenting to a thyroid practice, the prevalence of malignancy was 2.8, 3.7, 8.3, 12.3, and 29.7 percent for patients with serum TSH concentrations <0.4 mU/L, 0.4 to 0.9 mU/L, 1.0 to 1.7 mU/L, 1.8 to 5.5 mU/L, and >5.5 mU/L, respectively. Other studies had shown that when cancer was diagnosed, a higher TSH was associated with a more advanced stage of cancer.”
-
THYROID SCINTIGRAPHY
-
Q. What are the roles of thyroid scintigraphy in the evaluation of thyroid nodules?
- It is done in case of low TSH
- To select the thyroid nodule for FNAC in case of multinodular goiter- cold nodules being preferred
-
Q. What can be the difference between pertechnetate scan and iodine scan in thyroid nodules?
- Most thyroid nodules show congruence in pertechnetate and iodine scan
- However, 5% of malignant nodules appear hot in pertechnetate scan but cold in iodine scan
- Hence hot nodules in pertechnate must be confirmed by radioiodine scan
- These are called DISCORDANT NODULES
-
Q. Does an autonomous nodule (on radioiodine) require FNAC ?
- No
- They are rarely malignant
-
Q. What are warm nodules (indeterminate nodules)?
- Nodules that have uptake same as surrounding tissue- i.e., neither cold nor hot
- They must be distinguished from hot nodules by the T4 suppression test
-
Q. What is the T3/T4 suppression test?
- Perform the Radioactive iodine uptake test (RAIU)
- GIVE T3 25 UG TID FOR 10 DAYS OR T4 125 UG OD FOR 14 DAYS
- REPEAT RAIU AFTER GIVING THIS
- If Autonomous functioning – Hot nodule will remain hot- background uptake is suppressed
- If Warm nodule- reduced uptake in the nodule in repeat scan- this suggests warm nodule- Warm nodule may be malignant
-
Q. Should calcitonin be measured routinely in all patients with MTC?
- It is controversial
- Lots of false positive
- ATA is not for or against it
-
Q. What type of stimulation test can be performed to differentiate MTC from C cell hyperplasia inpatient with raised basal calcitonin?
- Pentgastrin stimulation test
- Some people even advise calcium stimulation test
- Must be done if basal calcitonin is >10 pg/ml
-
Q. What are the causes of false-positive raised calcitonin?
- Hypercalcemia
- Hypergastrinemia
- Neuroendocrine tumors
- Renal failure
- PTC
- Goiter
- Chronic autoimmune thyroiditis
-
Q. Which drugs lead to false-positive calcitonin?
- Pantoprazole
- Glucocorticoids
- Beta-blockers
-
Q. What calcitonin level in adults is considered suspicious for MTC?
- basal calcitonin >20 pg/ml and pentgastrin >100 pg/ml is suspicious
- If pentagastrin is not available- basal >100 pg/ml – suspicious
-
THYROID INCIDENTALOMAS
-
Q. Define thyroid incidentaloma?
- They are non-palpable thyroid nodules incidentally detected in tests done for other reasons
-
Q. Is it true, most incidentalomas detected on PET scans are malignant?
- Yes
-
Q. Which cystic nodules are more likely to be malignant?
- Ideally, all cysts >2 cm – the fluid should be aspirated and sent for cytopathology. Cysts more likely to be malignant are
- Complex cyst
- Bloody aspirate
- Cyst accumulating after drainage
- Ideally, all cysts >2 cm – the fluid should be aspirated and sent for cytopathology. Cysts more likely to be malignant are
-
Q. What is done for an incidental lesion in the thyroid picked up by FDG PET?
- Focal uptake on FDG PET- increase risk of malignancy – if >1 cm – do FNAC
- Diffuse uptake- less risk of malignancy- no FNAC