- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
- Q. Should perioperative thyroid function be done in all patients routinely?
- No
- Only in patients with clinical signs and symptoms of thyroid dysfunction and/or a history of prior thyroid disorder
- Perioperative hypothyroidism management
- Q. Which is the chief organ that must be taken care of in the Perioperative state in a Hypothyroid patient?
- Cardiac involvement
- Hypothyroidism affects cardiac function predominantly
- Q. What are the cardiac effects of hypothyroidism?
-
- Increase Peripheral vascular resistance
-
- Reduced cardiac contractility
-
- Reduced cardiac output
-
- Decreased blood volume
-
- Q. What are the effects of Hypothyroidism on the cardiac cycle?
- The Projection phase is prolonged and the Ejection phase is narrowed
- This leads to a reduction of cardiac output by 30-50%
- Q. Why is there an increase in peripheral vascular resistance?
- T3 is thought to have a vasodilatory effect which is lost in hypothyroid patients
- Q. Why do hypothyroid patients become hypotensive on exposure to anesthetic agents?
- This is because there is a loss of change of Cardiac output with the change of intrathoracic pressure and vasalva
- Q. What are the effect of Hypothyroidism on catecholamines?
- There is catecholamine resistance like effect
- Catecholamines are increased by a reduced adrenergic tone
- Q. What type of tachyarrhythmia is seen in Hypothyroid patients perioperatively?
- Torasdes de pointes
- Ventricular tachycardia is also sometimes seen
- This is because of prolonged action potential
- Q. Which other test is a must in patients with Hypothyroidism as far as Cardiac function is concerned?
- A lipid profile should be done
- It is often abnormal and often associated with perioperative risk of cardiovascular disease
- Q. What is better in MI patients with Hypothyroidism? PTCA or CABG?
- PTCA
- Because hypothyroid patients undergoing CABG without achieving euthyroidism have more complications
- Q. What are the effects of Hypothyroidism on a respiratory drive?
- Both hypoxic and hypercapnic respiratory drive is blunted in hypothyroid patients
- Q. What is its effect on respiratory muscle action?
- Respiratory muscle weakness is generally seen in most patients
- Q. What is Hoffman’s syndrome?
- Hypothyroidism with reduce muscle strength but increase muscle size
- Q. Which other respiratory problem is common in hypothyroid patients?
- Obstructive sleep apnea is common in hypothyroid patients
- Q. What is the problem of medicating in Hypothyroid patients in the perioperative period?
- Patients with Hypothyroidism have reduced drug metabolism
- Hence drugs that reduce respiratory function often have prolonged action in these patients
- Q. What is the problem with respiratory in Hypothyroid patients who develop sepsis?
- They have reduced respiratory surfactant development
- Q. Does T3 have some role in Lung maturation?
- It is observed that intra-amniotic T3 administration in babies with a high risk of RDS, reduces the risk of RDS
- PEARL: thyroid hormone induces surfactant synthesis
- Q. Is there an increase or reduced plasma volume in patients with Hypothyroidism?
- Circulating volume is reduced
- More fluid moves to interstitial space
- This is because of increased capillary permeability
- Q. Which electrolyte imbalance is prominent in patients with Hypothyroidism?
- Hyponatremia
- ADH is often increases in these patients
- Q. What is the effect on renal function in patients with Hypothyroidism?
- Hypothyroidism reduces the renal perfusion
- This may lead to worsening of renal function post-op
- Q. What is the most common CBC abnormality because of hypothyroidism?
- Anemia
- It is seen in 25-50% of patients with hypothyroidism
- Q. What type of anemia is commonly seen?
- Normochromic normocytic
- Q. What is the effect of hypothyroidism on bleeding?
- It increases the tendency to bleed
- Q. Which clotting factor is dysfunctional in patients with Hypothyroidism?
- Factor VIII and they often have acquired von Willebrand factor deficiency
- Q. What is the effect of Hypothyroidism on GI perioperatively?
- Can often lead to ileus and constipation
- Some people called it myxedema ileus
- Q. What is the effect on QT interval?
- Prolonged QT interval
- Q. Can hypothyroidism cause cortical insufficiency?
- Yes
- Q. How much time does it take perioperatively for TSH to normalize?
- 2 weeks after T4 administration
- Q. Which is the induction agent of choice in Hypothyroidism?
- Ketamine
- It has positive inotropic action and increases sympathetic activity
- Q. Which agent is not preferred?
- Thiopental is not preferred
- It increases systemic vascular resistance
- Q. In which cases Central hypothyroidism must be suspected ?
- Patients undergoing neurosurgery for Sellar or nonsellar mass lesions
- Patients with a history of traumatic brain injury
- History of cerebrovascular accident
- Q. How does hypothyroidism produce hyponatremia ?
- By increase of ADH
- By increase of ANF- atrial natriuretic peptide
- by decreased RAAS activity
- Q. What is the impact of uncontrolled hypothyroidism on coagulation?
- It reduced coagulation by decreasing Factor VIII activity
- Increases the risk of bleeding
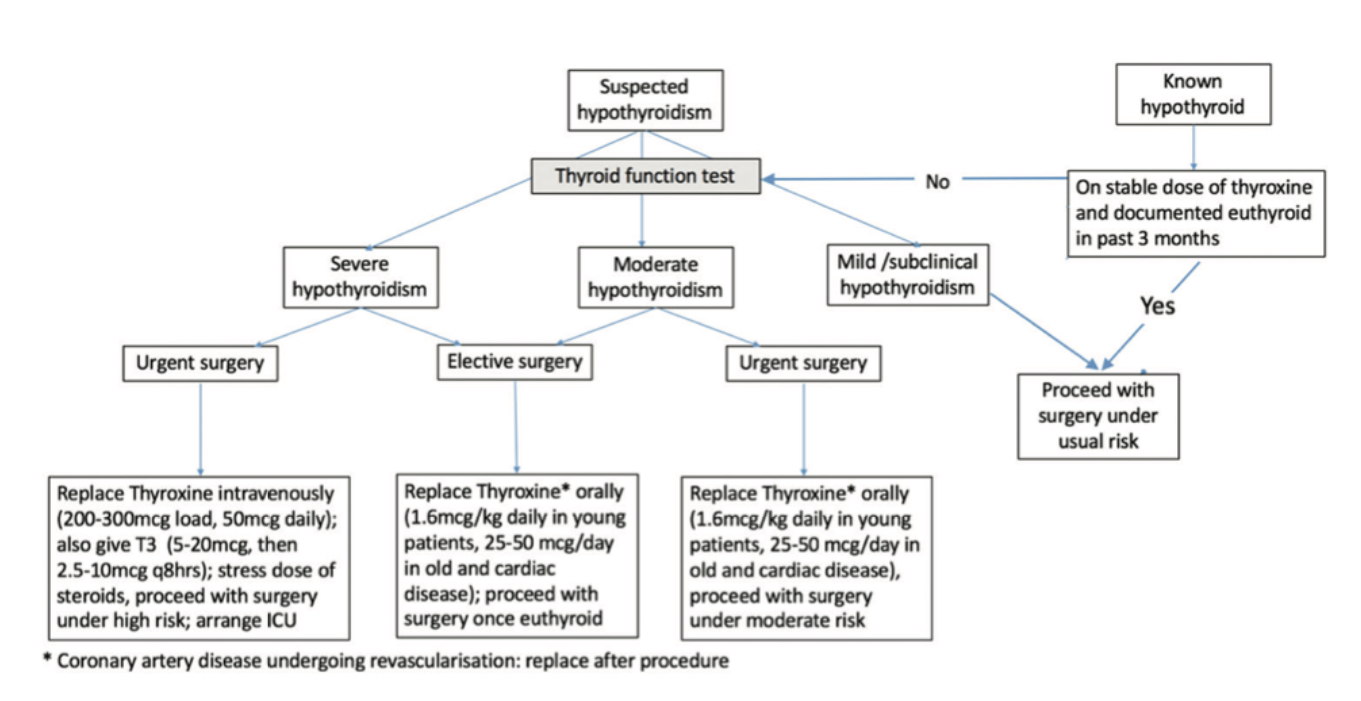
- Q. Give an algorithm for the management of perioperative hypothyroidism.
- Perioperative thyrotoxicosis management
- Q. What is the mainstay of perioperative thyrotoxicosis management?
- the mainstay is good beta-blocker coverage
- Q. Are thioamides useful?
- It is important to understand that thioamides block de novo synthesis of thyroid hormones and have little impact on already released hormone
- Hence in immediate situations thioamides may not have a significant role
- Q. What is the advantage of PTU in this setting?
- PTU blocks T4 --> T3 conversion in this setting
- However, it is not popular
- Q. What is the role of iodine in this situation?
- Iodine is useful in blocking the release of thyroid hormones
- However, it must be given only 1 hour after giving thioamides to prevent the iodine from being used as a substrate for de novo thyroid hormone synthesis
- This does not happen in Graves' disease but can occur in Toxic adenoma or Toxic MNG- hence in these situations it is better to give Thionamides first
- Q. What is done if a patient cannot take thionamides orally?
- Can be given per-rectally also
- Q. What kind of beta-blockers should be preferred?
- Long-acting ones are better than short-acting ones
- Hence Atenolol may be better as per this article
- Starting dose of 25-50 mg and can go up to 200 mg
- Keep pulse <80
- Q. What type of anesthetic agent is given in a perioperative setting?
- Sodium thiopental is preferred because it has anti-thyroid action
- ketamine and ephedrine increase sympathetic activity and must be avoided
- Pearl:
- hypothyroid patient- prefer Ketamine
- For hyperthyroid patients - prefer thiopental sodium
- Q. What agent is preferred in this setting for reversing neuromuscular blockage?
- Glycopyrrolate is preferred over atropine
- It has less chronotropic action
- Atropine may cause exaggerated tachycardia
- Q. Why is Aspirin avoided in these scenarios?
- They displace thyroid hormones from TBG and hence can precipitate a storm
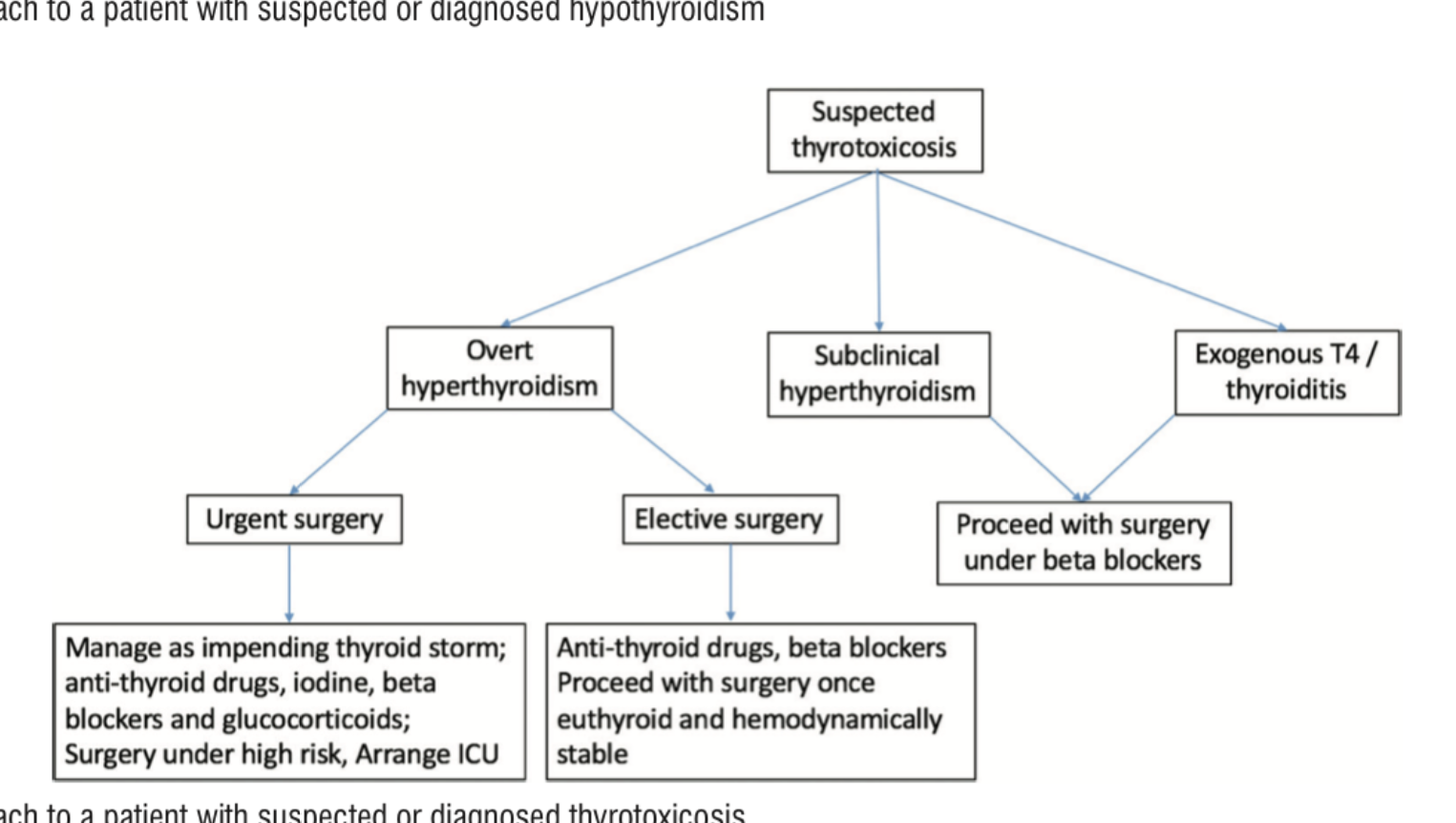
- Summarize the approach to thyrotoxicosis in perioperative settings
Reference:
- Malhotra, Bhanu; Bhadada, Sanjay K.. Perioperative Management for Non-Thyroidal Surgery in Thyroid Dysfunction. Indian Journal of Endocrinology and Metabolism: Sep–Oct 2022 - Volume 26 - Issue 5 - p 428-434 doi: 10.4103/ijem.ijem_273_22 & earlier notes