-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Video lecture
-
Q. What are the potential complications of hyperthyroidism in pregnancy?
- Abortion
- Low birth weight
- Premature labor
- Stillbirth
- Pre-eclampsia
- Heart failure
-
Q. Which are the two most common causes of hyperthyroidism in pregnancy?
- Graves’ disease
- HCG mediated hyperthyroidism
- Gestational transient thyrotoxicosis
- Hyperemesis gravidarum
- Trophoblastic hyperthyroidism
- Familial gestational hyperthyroidism
-
Q. What test is done to differentiate the above two diagnoses?
- TSH receptor antibody using 3rd generation TBII assay
-
Q. Using T3, T4, how will you distinguish the two?
- Graves disease has more T3 elevation
- HCG mediated have both T3 and T4 elevation but more of T4
-
Q. At what time does HCG peak, and by what time does it fall?
- Peaks at 10-12 weeks
- Falls by 14-18 weeks
-
Q. Which patients with hyperthyroidism in pregnancy are treated?
- Patients having overt moderate to severe hyperthyroidism due to Graves’ disease, gestational trophoblastic disease, and other causes are treated
- Patients with mild hyperthyroidism with T3/T4 < 1.5 times the ULN of the non-pregnant range are not treated
-
Q. Which is the only form of HCG-mediated hyperthyroidism that is treated?
- One secondary to gestational trophoblastic disease with overt hyperthyroidism and moderate to severe symptoms
-
Q. What is the goal of the treatment of hyperthyroidism in pregnancy (what are the TFT targets) ?
- T4 in upper limit or just above the trimester-specific normal range
- If a trimester-specific range is not available, keep free T4 in the upper limit of the normal range of non-pregnant women using the lowest possible dose
- TSH- lower limit or normal or suppressed
-
Q. What is the role of beta-blockers in the management of hyperthyroidism in pregnancy?
- IT IS GENERALLY AVOIDED
- Beta-blockers in low doses may be given in the initial part of the management of hyperthyroidism in pregnancy, mainly for symptomatic control (In special circumstances ONLY)
- They should be weaned off once ATD effects have taken over
- Typically, atenolol in a dose of 25-50 mg or Propranolol 20 mg TID may be given in the initial phase
- Generally not given for more than 2-6 weeks
-
Q. What are the potential adverse effect of beta-blocker on the fetus ?
- Bradycardia
- Hypoglycemia
- Low birth weight
- Respiratory depression
-
Q. Which of the two – PTU or Methimazole (MMI)/Carbimazole crosses the placenta?
- Both cross the placenta
- However, teratogenicity is more observed with Methimazole/Carbimazole and not PTU
-
Q. Which is the most common teratogenicity with MMI?
- Aplasia cutis
-
Q. Which are other potential manifestations?
- Choanal atresia
- Tracheoesophageal fistula
- Patent vitellointestinal duct
- Omphalocele
- Omphalomesntric duct
-
Q. What is the difference in potential liver toxicity of PTU vs. MMI ?
- PTU- produces hepatocellular inflammation- hepatitis while MMI produces cholestasis
-
Q. Which ATD are used when during pregnancy ?
- If women already on treatment with MMI becomes pregnant – switch to PTU as soon as pregnancy is confirmed
- In second trimester switch to MMI or Carbimazole again
- PTU 300 mg = 10-15 mg of MMI
-
Q. Should LFT be monitored while on PTU therapy ?
- No
- Because the hepatotoxicity is idiosyncratic and hence no point of LFT monitoring
- If however monitoring is done, PTU is stopped if Liver enzymes are >3 times ULN
- Stop PTU and monitor LFT, if it is rising – refer to hepatologist
-
Q. What is done in the third trimester ?
- Autoimmune thyroid disease often improves in 3rd trimester
- If a patient goes into remission in 3rd trimester than ATD can be potentially tapered and stopped if TFT is normal and TRAb is negative
- Some women switch from TSH stimulating to blocking antibody
- Stopping of drug is possible in 1/3rd of women
-
Q. What is the starting dose of PTU / MMI in pregnancy ?
- Start with lowest possible dose
- PTU- 50 mg TID
- MMI- 5-10 mg
- CBZ- 5-15 mg
- Start with lowest possible dose
-
Q. What are the consequence of under-treatment and over treatment of hyperthyroidism in pregnancy on the fetal thyroid function ?
- Undertreatment – may lead to central hypothyroidism due to negative feedback of excess T4/T3
- Overtreatment- fetal primary hypothyroidism
-
Q. Graves disease improves postpartum, True or false ?
- False
- It may worsen postpartum
- Also women in remission – may relapse in postpartum period
-
Q. Which are 2 important consequences of uncontrolled hyperthyroidism in 3rd trimester?
- Neonatal thyrotoxicosis
- Low birth weight
-
Q. What is the indication for surgery in hyperthyroidism in pregnancy ?
- When a patient has allergy or agranulocytosis due to ATD
- In such cases, surgery can be completed in 2nd trimester
- However, risk of surgical complications are higher
-
Q. What preparation is done before surgery ?
- Beta-blockers and
- Low dose of SSKI- 1-3 drops/day for 7-10 days before surgery
-
**Nursing mothers **
-
Q. Which is secreted more in breast milk- PTU or MMI ?
- MMI is excreted more in breast milk as it is less protein-bound unlike PTU
- However, since dose of MMI is much lower- risk of fetal complications are less
- There are very rare/ no cases of fetal complications due to drug presence in breast milk – for either drug
- Hence MMI is preferred in nursing mothers because of less risk of hepatotoxicity
-
Q. Should TFT of infant be monitored if mother is on MMI ?
- Generally no
- However, if MMI dose is >20 mg – then monitor TFT of infant every 1-3 months
-
**Fetal hyperthyroidism **
-
Q. What TRAb level in 2nd and 3rd trimester predict the occurrence of neonatal hyperthyroidism ?
- 2nd/ 3rd trimester TRAb levels > 3 times ULN or > 5 IU/l predict the occurrence of neonatal hyperthyroidism with 100% sensitivity and 40% specificity.
-
Q. When is the TRAb level typically determined during pregnancy ?
- TRAb level is tested typically at 18-22 weeks of pregnancy
-
Q. What is the risk of fetal hyperthyroidism in women with Graves disease in pregnancy ?
- 1-5% risk
-
Q. What are the signs of fetal hyperthyroidism ?
- Fetal HR >160 bpm
- Fetal goiter – with central blood flow on Doppler
- Craniosynostosis
- Advanced bone age
- Poor growth
- Rare cases- heart failure and hydrops
-
Q. When is TRAb monitoring done in 3rd trimester and what is its role ?
- It is done at 24-28 weeks
- TRAb levels >3-5 times the ULN suggest a high risk of fatal complication
-
Q. A woman has past history of Graves disease but currently in remission. Should TRAb be measured in such women?
- Yes
- TRAb must be measured at 20-24 weeks and if >3-5 times ULN fetal monitoring is required
- Women may be in remission but TRAb may persist and hence monitoring is necessary
-
Q. What are the types of assays for TRAb ?
- TBII assay- just tells about presence of antibodies but does not tell about function – it is less expensive and generally adequate test in pregnancy
- TSI assay – tells about function of the TRAb- stimulatory or not but more expensive
-
Q. How is the monitoring of the fetus done in case of TRAb antibodies being positive ?
- Fetal heart rate monitoring and regular ultrasound
-
Q. What is THE characteristic of goiter in fetal hyperthyroidism ?
- They have central flow on color doppler which is not seen in fetal goiter due to hypothyroidism
-
Q.. Can fetal thyroid function be measured ?
- Yes
- But umbilical vein sampling at 20 weeks
- However, this is not routinely recommended
-
Q. When is fetal thyroid function done ?
- It is done if there is fetal goiter and it is not sure whether the fetus has hypothyroidism or hyperthyroidism due to maternal ATD treatment
-
Q. If the mother is euthyroid, but fetal hyperthyroidism is confirmed- what is done ?
- Mother is treated with ATD despite being euthyroid
-
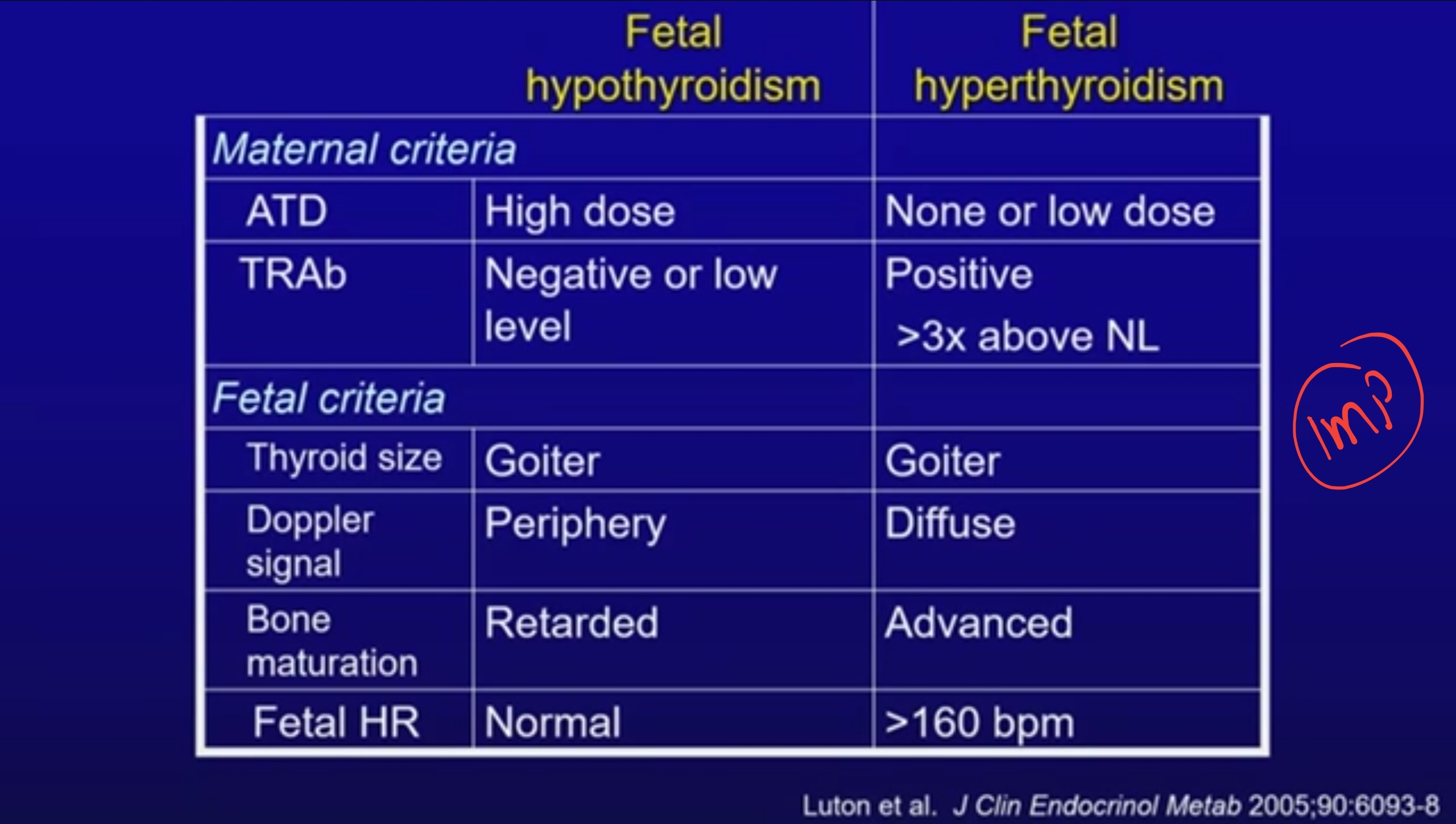
Q. How can you differentiate fetal hypothyroidism from fetal hyperthyroidism ?
- Fetal hypothyroidism vs Fetal hyperthyroidism
- Fetal hypothyroidism vs Fetal hyperthyroidism
Please consider donating to "Notes in Endocrinology" to keep us going. Please visit our DONATION page to know more