-
- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
- Credits
-
Authors Note:
- This topic is very well summarized by the talk given by me sometime back. It is best to start with that video first:
- This topic is very well summarized by the talk given by me sometime back. It is best to start with that video first:
Here are other videos on the same topic
-
-
Q. What is the upper limit of TSH cutoff to define hypothyroidism in pregnancy ?
- The earlier guidelines recommended cutoffs of 2.5 , 3.0 and 3.0 in 1st , 2nd and 3rd Trimester.
- The new guidelines recommend as follows:
- Use the cutoff obtained from normal pregnant women in your centre.
- If they are not available, use cutoff which are similar to your population.
- If again, they are un-available then use ULN of TSH as 4.0 mIU/l
-
Q. What is the trimester specific reference range of TSH as obtained from study done in Haryana ?
- In the study done by Rajput et al, the 2.5–97.5th percentiles for TSH obtained in this study were
- 1st Trimester- 0.37–3.69 μIU/ml
- 2nd Trimester- 0.54–4.47 μIU/ml
- 3rd trimester- 0.70–4.64 μIU/ml
-
Q. What is definition of isolated hypothyroxemia of pregnancy ?
- Free T4 in the range of lower < 2.5th – 5th percentile of population with normal TSH
-
Q. What were the free T4 cutoff ranges in study done in Haryana by Rajput et al ?
- FT4,
- 1st T - 0.88–1.78 ng/ml
- 2nd T- 0.91–1.78 ng/ml
- 3rd T - 0.83–1.73 ng/ml
- FT4,
-
Q. Is hypothyroidism associated with infertility ?
- Hypothyroidism in certain cases is associated with
- Anovulation
- Increase 1st-trimester abortion
- Hypothyroidism in certain cases is associated with
-
Q. What are the potential complications of hypothyroidism in pregnancy?
- Abortion
- Preterm delivery
- Increase perinatal morbidity and mortality
- Hypertension in pregnancy
- Increase LSCS
- Placental abruption
- Postpartum hemorrhage
- Neurocognitive impairment
-
Q. What are complications with Subclinical hypothyroidism (SCH) in
pregnancy?- Increase the risk of
- Preterm delivery
- Fetal loss
- Placental abruption
- Pre-eclampsia
- More with those who are TPO positive
-
Q. Is SCH in pregnancy associated with a higher risk of cognitive
impairment?- Observation studies have shown such a result
- But RCT has not shown any effect on cognitive impairment
-
Q. What is the definition of isolated maternal hypothyroxinemia of
pregnancy?- Free T4 in the lower 5th to 10th percentile of
reference range - TSH is a normal range
- Free T4 in the lower 5th to 10th percentile of
-
Q. Is isolated maternal hypothyroxinemia associated with poor outcomes?
- Studies have shown mixed results
- Some studies have shown an increased risk of preterm delivery
- Effect on IQ also has shown mixed results. However, an RCT has shown no
difference
-
**Treatment **
-
Q. Is the treatment of isolated hypothyroxinaemia indicated?
- No
-
Q. For hypothyroid women planning to be pregnant, what should be the
advice?- Keep TSH <2.5 before pregnancy – some suggest <1.2
- Increase of dose may be required once pregnancy is confirmed
- Patient can pre-exmptively increase the dose by 30%
-
Q. What is the simple way of increasing thyroid dose in women with
pre-existing thyroid disease who becomes pregnant?- Ask the patient to take the same dose nine times a week instead of 7!
- Double the dose on two days of the week
-
Q. What is the reason for the increase of thyroid hormone requirement during
pregnancy?- Increase of TBG and it's binding
- Transfer of T4 to the fetus
- Reduce iodine
- Increase destruction of T4 by the placenta
- Reduce absorption due to iron and calcium
-
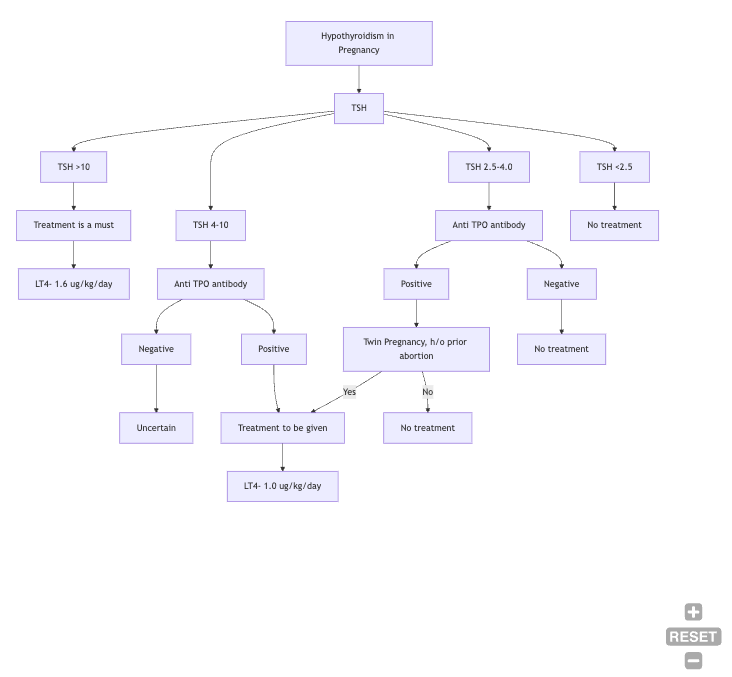
Q. What is the dose of levothyroxine in pregnancy?
- Moderate to severe hypothyroidism- full replacement dose of 1.6 mcg/kg
- TSH <10 – give 1 mcg/kg
-
**Pregnancy outcome in subclinical hypothyroidism (SCH) and pregnancy **
-
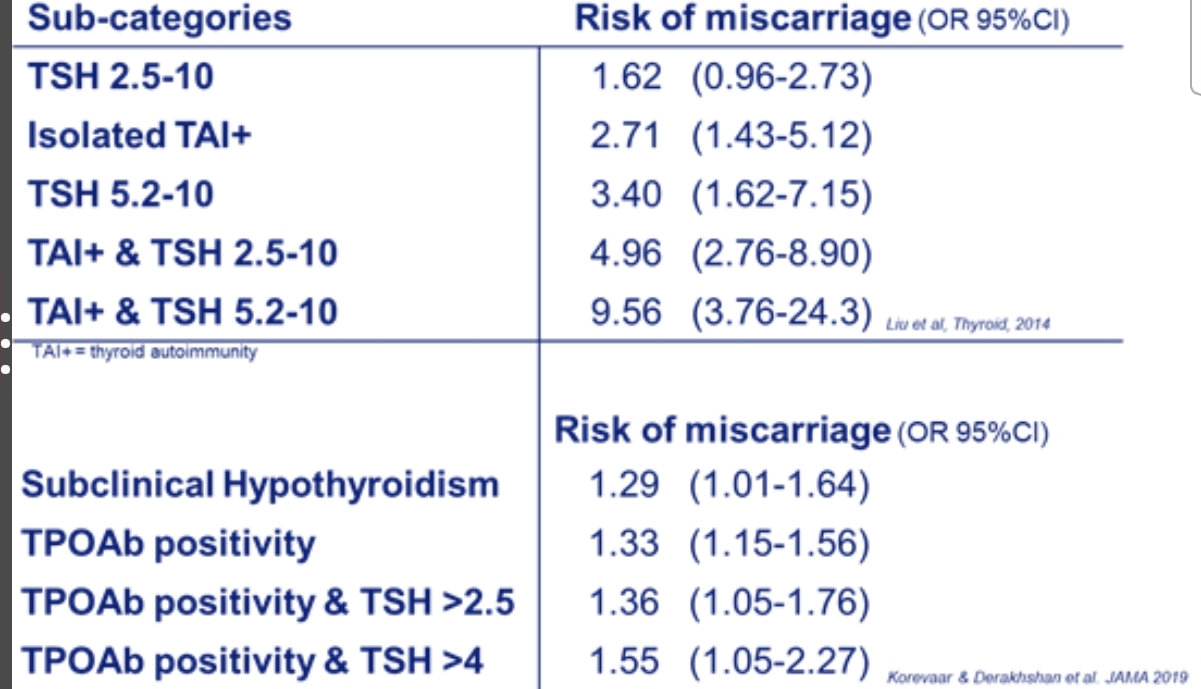
Q. Give the data for pregnancy outcome and SCH, which show more fetal
loss?-
- Chinese study
- Women with TSH 5-10 had more fetal loss compared to women with normal
thyroid function (7 % vs 2%) - Those with SCH and Anti TPO positive- had the highest risk – 15%
-
- Negro et al
- In Anti TPO negative women :
- TSH 2.5- 5.0 had higher fetal loss compared to those with TSH <2.5 in
1st trimester (6% vs. 3%)
-
- Baker et al
- Patients undergoing IVF – those with TSH <2.5 had better outcomes
than those with TSH >2.5
-
-
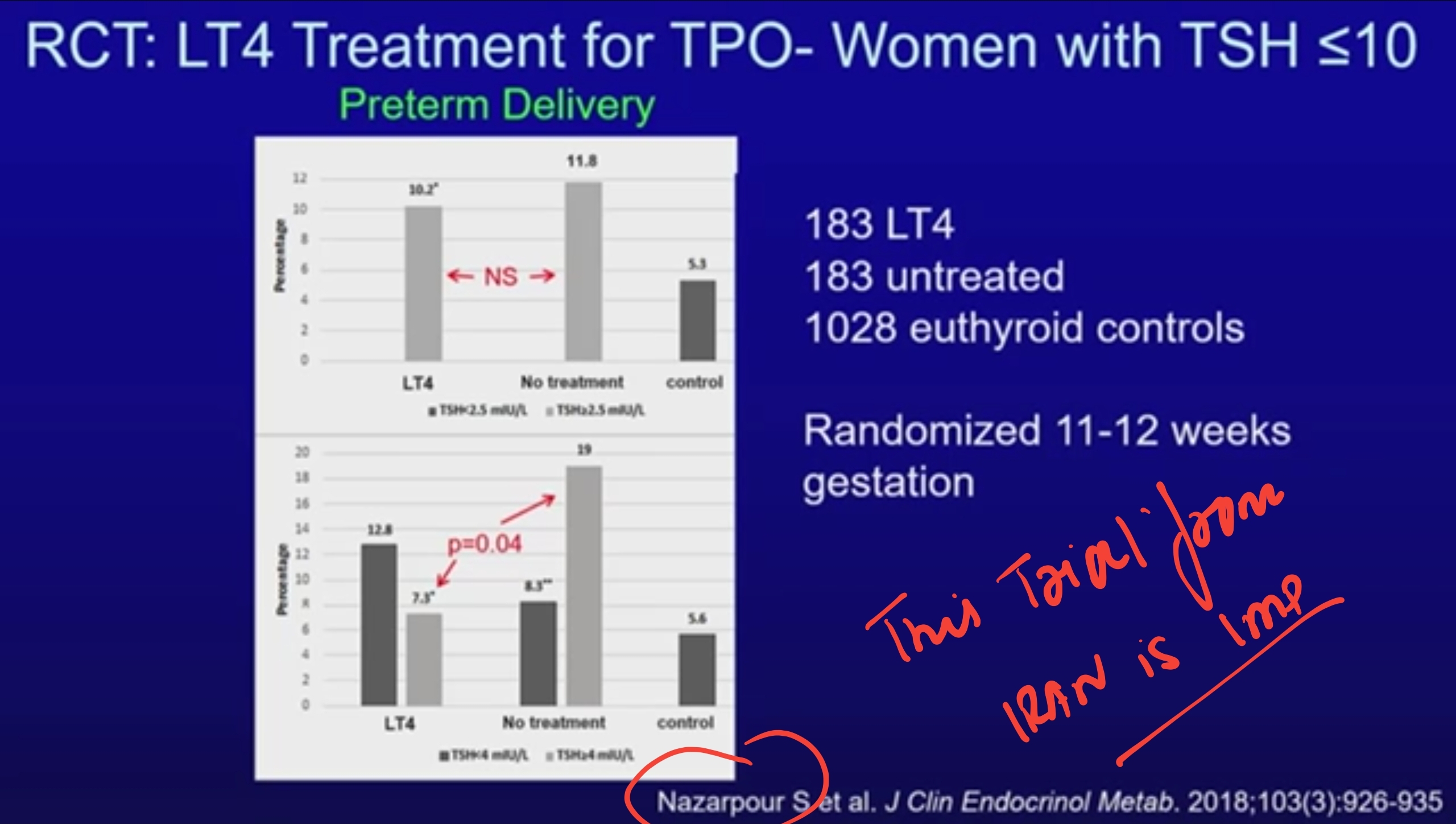
Q. Overall, Does treatment for Subclinical hypothyroidism in pregnancy have any benefit?
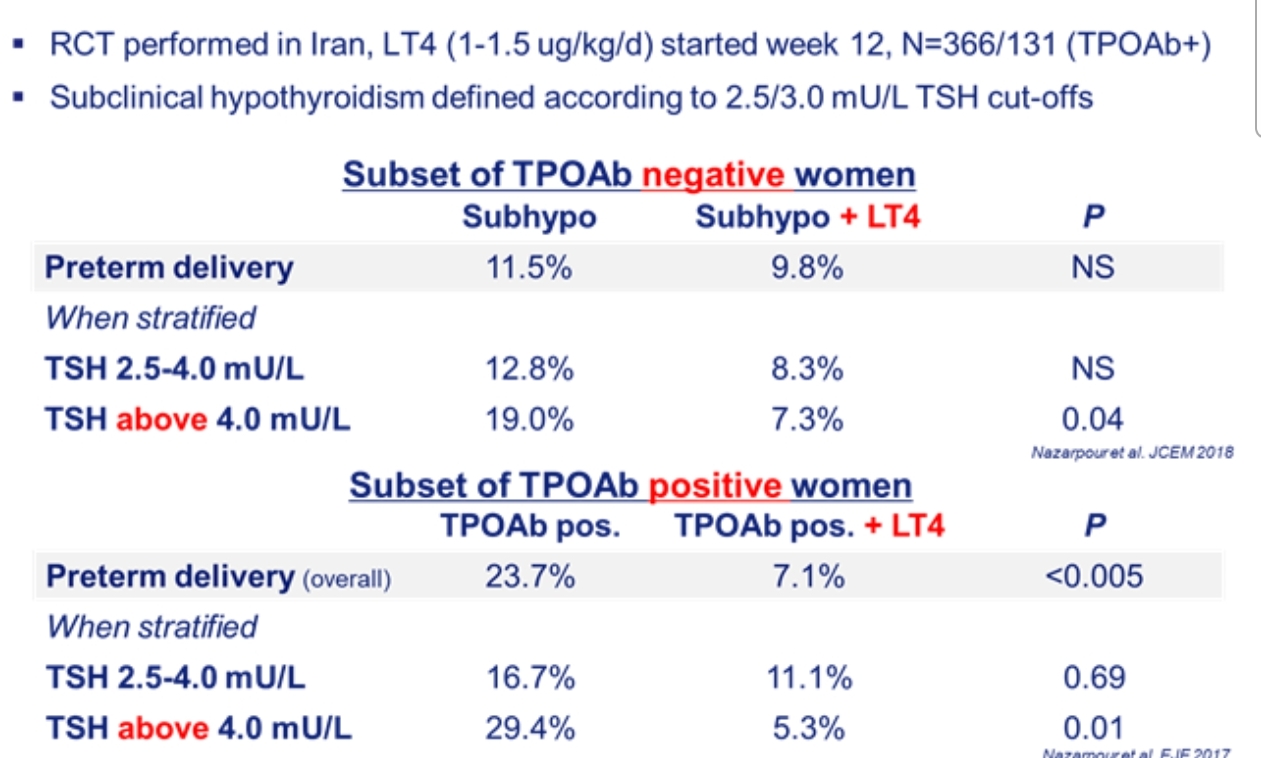
- The main results come from a trial in Iran which had shown that the risk of Preterm delivery is reduced if SCH is treated
- The Casey trial published in NEJM did not show any benefit in any parameter - this was a negative trial
- however, this trial started intervention at 17 weeks which was a little too late, right?
- The main results come from a trial in Iran which had shown that the risk of Preterm delivery is reduced if SCH is treated
-
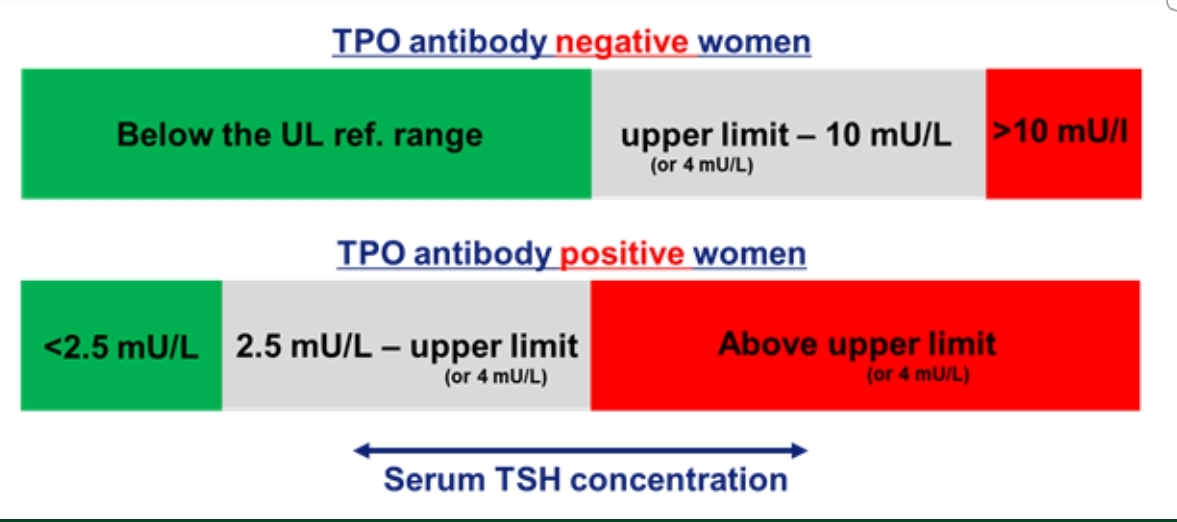
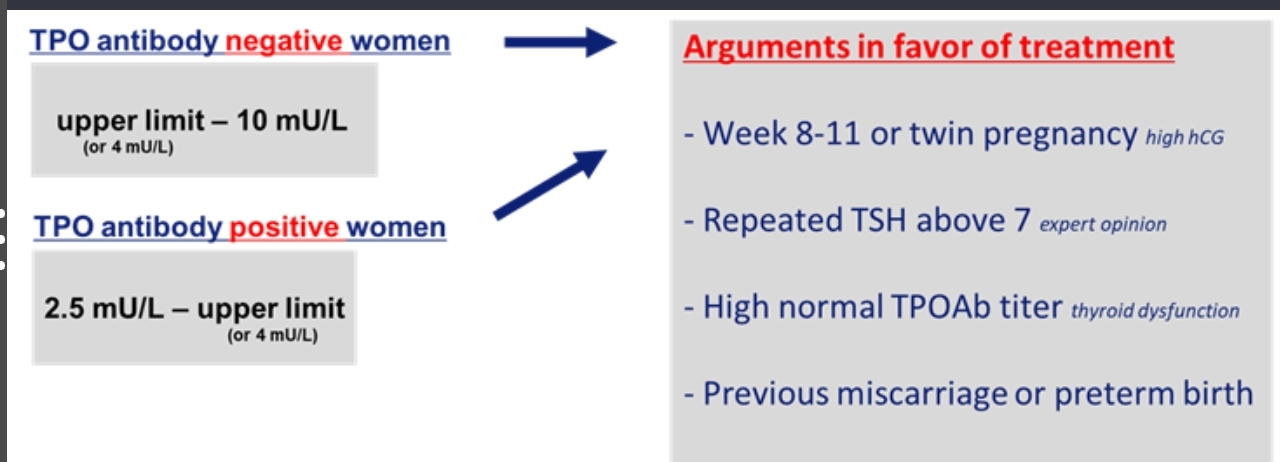
Q. What do the current guidelines say about treating Subclinical hypothyroidism in pregnancy
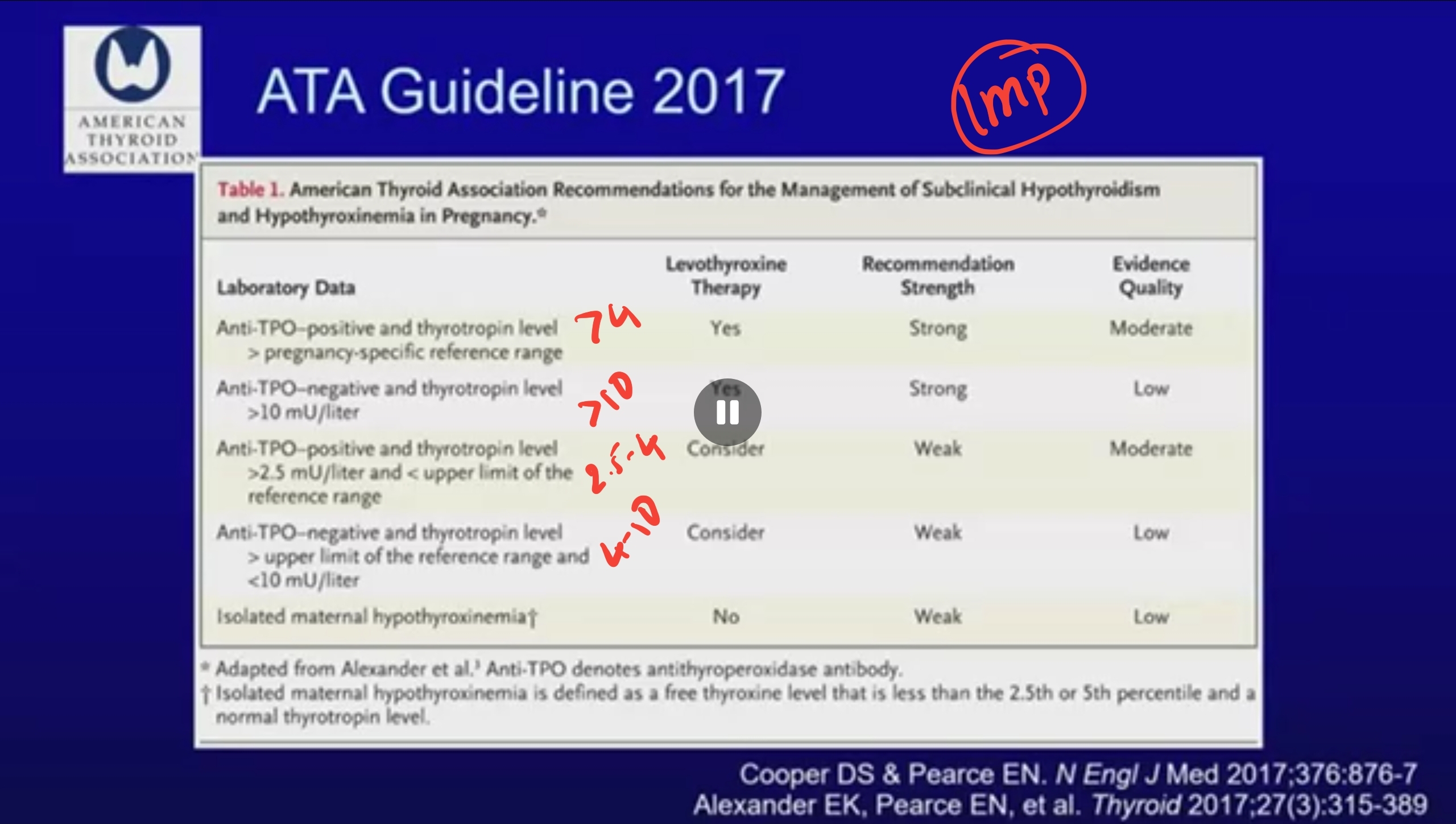
- TSH >10- treatment is a must
- TSH 4-10 with TPO positive - treatment MUST be given - moderate evidence to support this
- TSH 2.5-4 with TPO positive- weak evidence - it is the gray area
- TSH 4 to 10 with TPO negative - and again gray area
- Isolated maternal hypothyroxinemia- current guidelines do not recommend treatment
-
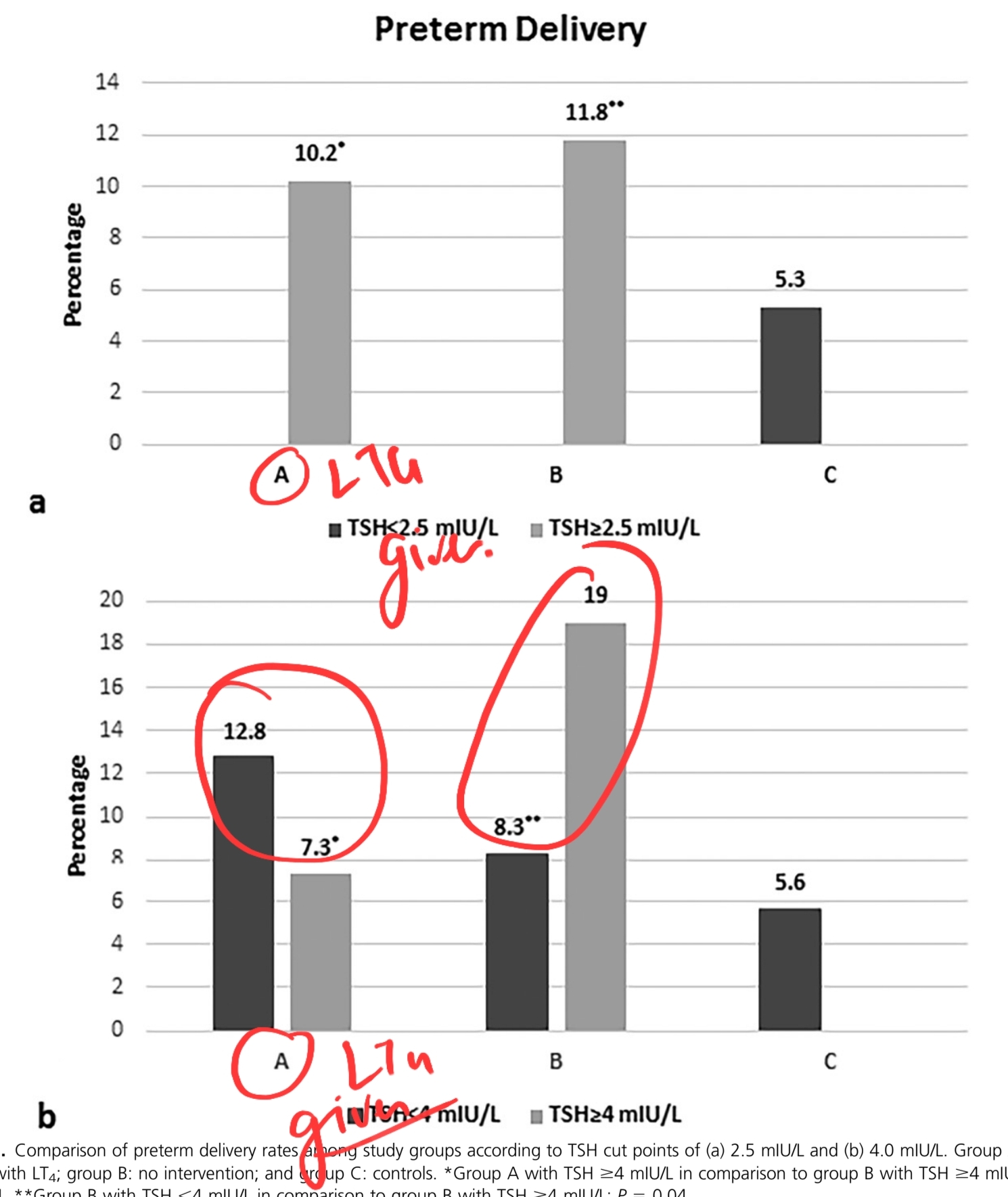
Q. What is the data about women with SCH with negative TPO antibodies?
- The data comes from a trial by Nazarpour et al. published in JCEM
- This is a trial done in SCH women with NEGATIVE TPO antibody
- So results of this trial were
- TPO negative women with TSH 2.5-4.0- no difference in preterm delivery on treatment
- those with TSH >4.0 had a significant benefit in terms of lesser preterm delivery on treatment
- the dose of LT4 given was 1 mcg/kg per day
- Notes from the study
- this is a well-conducted study and very well written
- so, in this study, they took three groups-
- A- treated with LT4
- B- not treated
- C- Control group
- Now, in this, they clearly showed that in TPO negative women
- If TSH >4 with anti-TPO negative- there is a clear benefit of treatment in terms of preterm delivery
- if TSH is 2.5-4.0, there is no benefit
- the graph below clearly summarizes the outcome
- Conclusion from the author
- So, this study targets an important subpopulation
- i.e., TPO negative women
- ^^In women with TSH 4 to 10 and TPO negative treatment with LT4 in the dose of 1 ug/kg shows clear benefit ^^
-
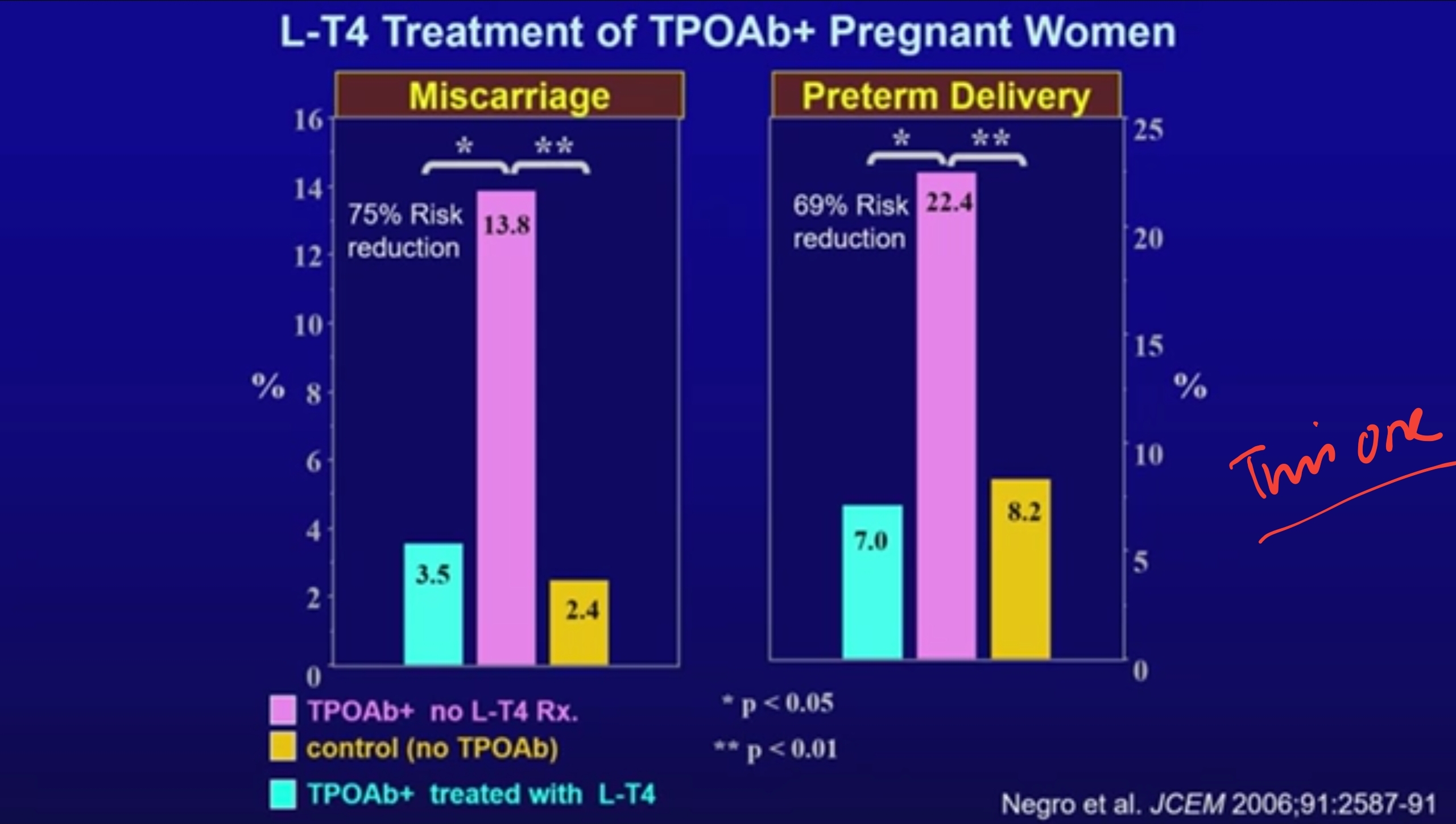
Q. Tell me more about Anti TPO antibody and pregnancy
- Studies have consistently shown a correlation between Anti TPO antibody and preterm delivery
- if the TSH is higher, the problem is worse
- We don't know if treatment is going to benefit in any way
- The study by Negro did show benefit with treatment - this study was published in 2006
- The study by Negro did show benefit with treatment - this study was published in 2006
- However, the recent TABLET trial published in the NEJM did not show any benefit
- the current guidelines suggest that Euthyroid anti-TPO positive women no treatment should be given
- However, if they have a prior history of misconception- then treatment may be considered
-
Q. Why does Anti TPO antibody cause fetal loss ? #ClinicalPearl
- There are two ways
- TSH dependent way
- Changes in endometrial T cells
- Less IL4 and IL10 secretion and increased interferon-gamma secretion
- increase cytotoxic T cell migration
- increase the immunogenicity of the uterus
- TSH independent way
- Reduced response of thyroid gland to HCG stimulation
- development of subclinical or overt hypothyroidism
- TSH dependent way
- There are two ways
-
Q. Tell me more about the TABLET trial ?
- Levothyroxine in Women with Thyroid Peroxidase Antibodies before Conception | NEJM
- This was a double-blind, placebo-controlled trial to investigate whether levothyroxine treatment would increase live-birth rates among euthyroid women who had thyroid peroxidase antibodies and a history of miscarriage or infertility.
- A total of 19,585 women from 49 hospitals in the United Kingdom underwent testing for thyroid peroxidase antibodies and thyroid function.
- They randomly assigned 952 women to receive either 50 μg once daily of levothyroxine (476 women) or placebo (476 women) before conception through the end of pregnancy.
- The primary outcome was live birth after at least 34 weeks of gestation.
- ^^There were no significant between-group differences in other pregnancy outcomes^^, including pregnancy loss or preterm birth, or in neonatal outcomes. Serious adverse events occurred in 5.9% of women in the levothyroxine group and 3.8% in the placebo group (P=0.14).
-
The use of levothyroxine in euthyroid women with thyroid peroxidase antibodies did not result in a higher rate of live births than placebo
- Levothyroxine in Women with Thyroid Peroxidase Antibodies before Conception | NEJM
-
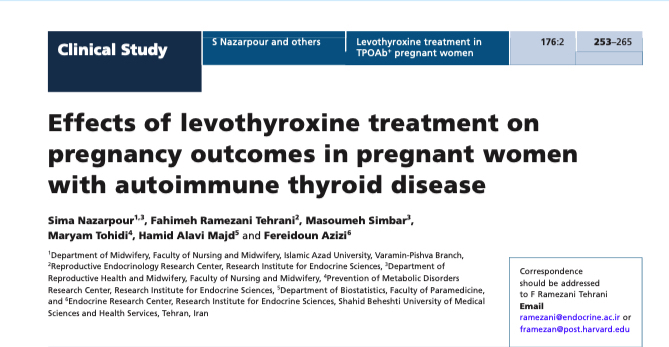
Q. Is there a study by Nazarpour et al for Anti TPO antibody positive women ?
- Yes
- Other studies by Nazarpour
- In this study, they studied the impact of LT4 in preventing preterm delivery in TPO positive women
- again, they found there was a benefit- but it was mainly confined to women with TSH >4.0
- No benefit in euthyroid women with TPO positive (i.e., TSH <2.5)

- The dose used in the above study was as follows:
- dose of 0.5 µg/kg/day if they had TSH<1.0 µIU/mL
- 0.75 µg/kg/day for TSH between 1.0 and 2.0 µIU/mL
- 1 µg/kg/day dose for TSH >2.0 µIU/mL or a TPOAb titer exceeding 1500 IU/mL; dosages were maintained throughout gestation
- One of the important things they have suggested, which has practical importance, is that the benefit is the most of the medication is started between 8 weeks when more of the abortions happen #ClinicalPearl
-
Q. So what is the story so far from the above trials about Subclinical hypothyroidism in pregnancy?
- So the story so far for Subclinical hypothyroidism in pregnancy
- SCH is definitely associated with poor obstetric outcome
- The outcome is worse in those with TPO positive
- both low Free T4 and high Free T4 are associated with low IQ in children
- But the question is - "Does treatment with LT4 offer benefit ?"
- The study done by Nazapour from Iran shows that women who are TPO negative and TSH is more than 4 have benefited from LT4 treatment in a dose of 1 ug/kg. But no benefit is seen if TSH is 2.5-4.0
- Another study by the same author in another journal shows TPO-positive women have benefits- especially those with TSH >4.0. The benefit in TSH 2.5-4.0 is minimal
- The dose used in the above study was as follows:
- dose of 0.5 µg/kg/day if they had TSH<1.0 µIU/mL
- 0.75 µg/kg/day for TSH between 1.0 and 2.0 µIU/mL
- 1 µg/kg/day dose for TSH >2.0 µIU/mL or a TPOAb titer exceeding 1500 IU/mL; dosages were maintained throughout gestation
- The dose used in the above study was as follows:
- So the story so far for Subclinical hypothyroidism in pregnancy
-
Q. How is adjustment done postpartum ?
- Postpartum reduce the dose to what patient was taking preconception.
- Or in other words, reduce the dose by 25-30% and repeat the thyroid function at 6 week post partum.
- Some patient who are treated during pregnancy may not require treatment post partum and LT4 may be discontinued in such patients. A repeat TFT at 6 weeks must be done. -
Q. Does uncontrolled maternal hypothyroidism impact lactation ?
- Yes. Uncontrolled hypothyroidism is associated with poor lactation.
- Additionally in women with poor lactation, additionally, hypothyroidism must be ruled out. -
#Updates: Summary from Tweetorial by Tim Korevaar
- Tweet by Tim Korevaar
- The incidence of SCH in pregnancy is 3.5% of pregnancy
- Etiology
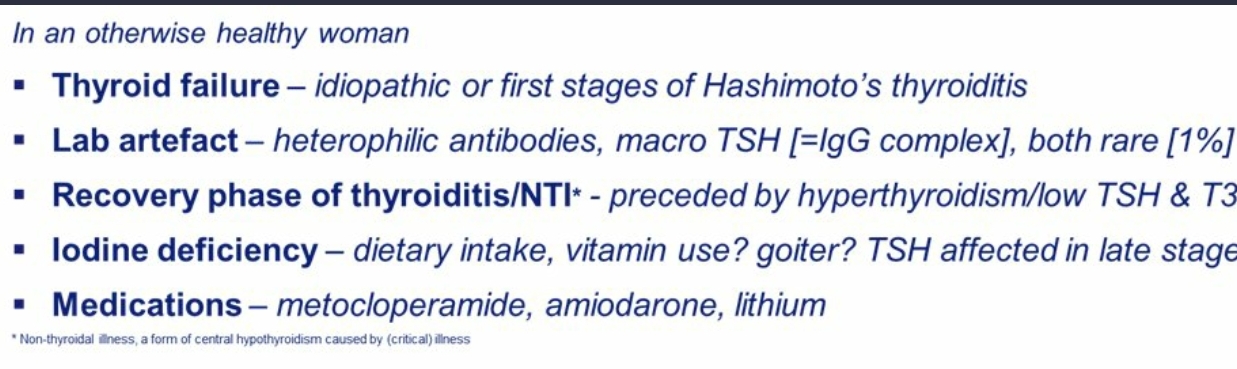
- Any value of TSH above 10 must be considered Overt hypothyroidism
- Prefer Free T4 to Total T4 for assessment
- Back to subhypo, why care?
- Because it is the opposite of normal physiology (fig):
- hCG➡️TSH receptor stimulation➡️FT4⬆️& TSH⬇️
- Also, hCG➡️pituitary TSH receptor stimulation➡️ultrashort feedback loop➡️TSH suppression
- AKA the Brokken-Wiersinga-Prummel Loop https://t.co/wtLxrCHSNh https://t.co/mJjUyszL9u
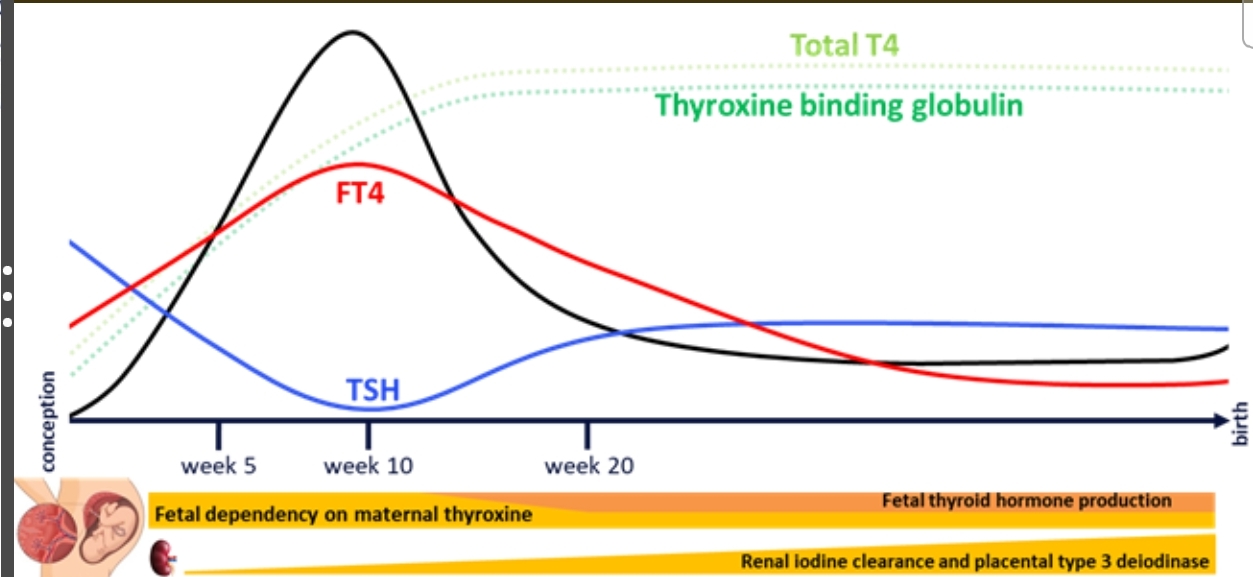
- Remember the TSH is lower due to HCG than it would be in a non-pregnant person
- Nice graphic from the ATA guidelines
- TPO positive women have a poor response of the thyroid gland to the HCG #important
- Hence classification based on the TPO makes sense
- TPO positive women have more risk of abortion
- So the risk is fine but does that translate the risk of benefit
- One RCT has shown that giving LT4 reduces the risk of preterm delivery

- "If you decide to treat, don't overtreat."
- Summary and take-homes
- Subclinical hypothyroidism during pregnancy:
- Reflects an abnormal physiology
- Use correct reference ranges to diagnose
- Risk stratify TPOAbs, gestational age, etc.
- If you treat, ➡️ Don’t overtreat
- My notes
- Anti TPO plays an important role in risk stratification because anti-TPO positive women don't respond to HCG
- Free T4 is more important for diagnosis and treatment
- In the gray area - look at situations where you wish to treat vs. not treat
- Don't over-treat it - that is a problem
- Only one RCT shows the benefit of LT4 in SCH in pregnancy in reducing preterm delivery
- The risk of SCH + Anti TPO and probability of miscarriage is very high
-
Additional Notes from the American Thyroid association 2017 guidelines
-
Q. What are the risk of overt hypothyroidism in pregnancy ?
- Low IQ of child
- Spontaneous pregnancy loss
- Low birth weight
- Premature birth
-
Q. How much IQ is reduced in overt hypothyroid women who are not treated ?
- 7 point reduction in IQ of the child in over hypothyroid women who are not treated.
-
Q. Is subclinical hypothyroidism with Anti TPO negative associated with increase pregnancy loss ?
- Yes
- There is some evidence to suggest this.
- Pearl
- Euthyroid women with anti TPO positive- increase risk of spontenous pregnancy loss
- Subclinical hypothyrodism with anti TPO negative- also increased risk of spontenous pregnancy loss.
-
Q. Is Subclinical hypothyroidism associated with increase risk of preterm delivery ?
- Subclinical hypothyroidism with anti TPO positive- increased risk of preterm delivery
- SCH without Anti TPO antibody – may have risk if TSH 5-10 but no risk if TSH 2.5-5.0
-
Q. Does treating subclinical hypothyroidism in mother improve the IQ in the offspring ?
- CATS study and other recent study donot show improvement in outcome in IQ in child of women with subclinical hypothyroidism or isolated hypothyroxemia who are treated with LT4.
- However, lack of positive outcome does not rule possibility of harmful effects in the offspring.
-
Q. Is isolated hypothyroxemia associated with lower IQ in children ?
- There is insuffienct evidence for or against this.
- However, there is no evidence that treating isolated hypothyroxemia
-
Q. Is treatment of overt hypothyroidism recommended in pregnancy ?
- Yes
-
Q. What should be the treatment TSH target for treatment while treating hypothyroidism in pregnancy ?
- The TSH target should be in the lower half of pregnancy specific range.
- If local pregnancy specific range is not available then it is recommend to keep TSH <2.5 mIU/l
-
Q. How frequently is monitoring of thyroid function done in women with hypothyroidism in pregnancy ?
- Monitoring of thyroid function should be done every 4 weeks till midgestation and then once near 30 weeks
-
Q. How is dose changed in women with preconception hypothyroidism on LT4 replacement ?
- One simple way is to ask patient to take 2 additional tablet in the week, for example instead of 7 tablets of LT4 take 9 tablets
- Or in other words increase the dose by 25-30% from the preconception dose as soon as pregnancy is confirmed.
-
Q. In hypothyroid women planning to get pregnant what should be the preconception TSH ?
- Preconception TSH should be kept <2.5
Please consider donating to "Notes in Endocrinology" to keep us going. Please visit our DONATION page to know more