-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Video Lecture:
-
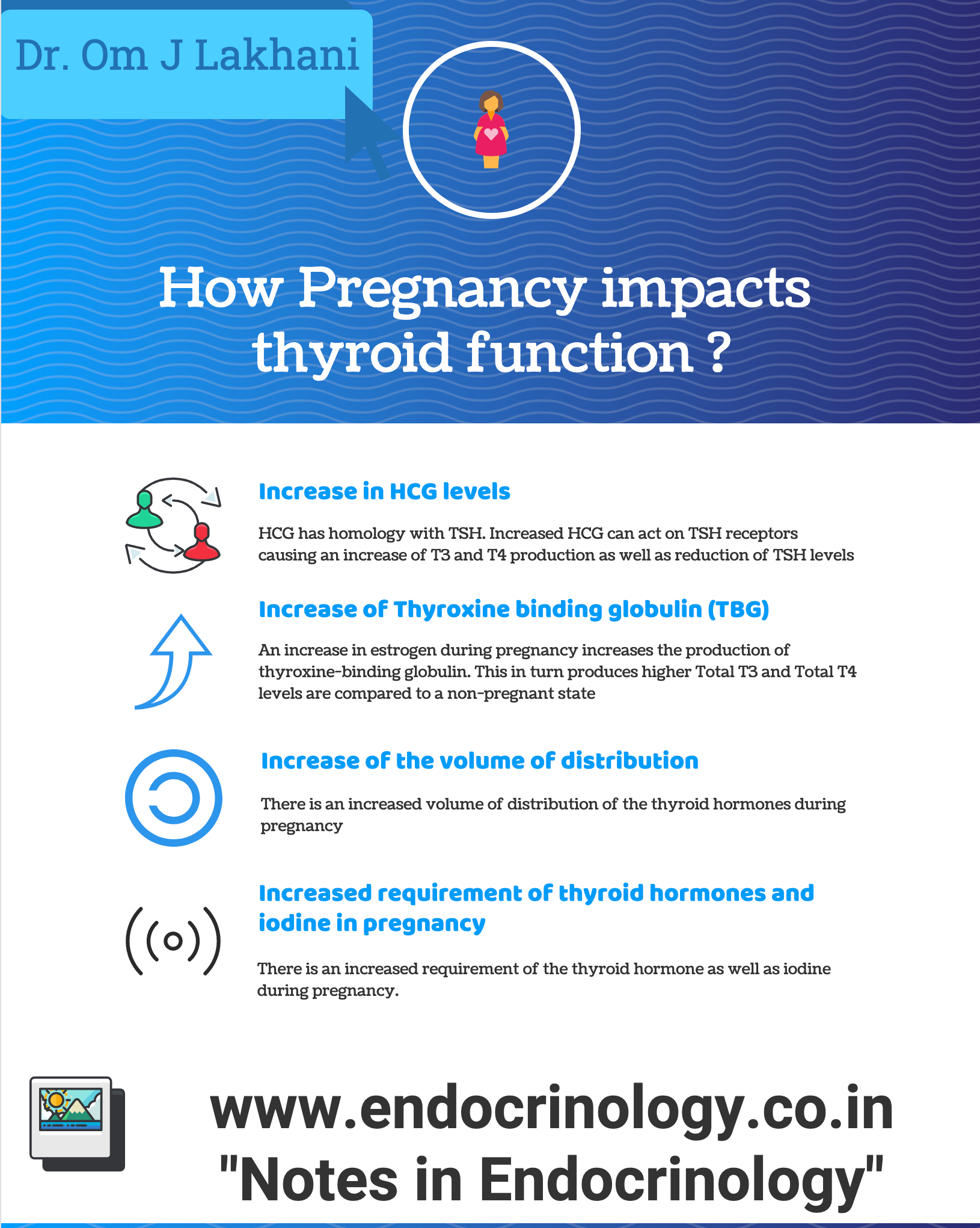
Q. What are the changes to thyroid function during pregnancy?
- Reduction of TSH in the first trimester due to increase of HCG
- Increase of total t3 t4 because of increase of TBG
- Mild increase of free T4 at the end of the first trimester because of HCG
- Mild reduction between 1st to 2nd trimester followed by a plateau
-
Q. Till how long do total t3 and t4 increase?
- Total t3 and t4 increases up to 20 weeks, then it plateaus
- Increase thyroid hormone requirement matches the increase of TBG, and hence it plateaus
-
Q. When does TBG rise in pregnancy, when does it peak and till when does it remain high ?
- It increase at 7 weeks of pregnancy
- Peaks at 16 weeks and remains high throughout the pregnancy
-
Q. Is there a significant reduction of upper limit of TSH in pregnancy ?
- Conventionally, based on studies from Europe and USA, the 1st Trimester TSH upper limit is set to 2.5 mU/l
- However, recent studies from India and China show that the fall in TSH in first trimester is modest and about 0.5-1 mU/l from UL in non pregnant patients
- There is no reduction in TSH upper limit in the first 7 weeks of pregnancy, a substantial reduction in 1st Trimester due to HCG with some rise in 2nd and 3rd T.
-
Q. What about the lower limit of TSH ?
- The lower limit of TSH is significantly lower compared to non pregnant reference ranges, sometimes may even be non detectable.
- Also, it is important to note that subclinical hyperthyroidism in pregnancy is not associated with adverse maternal or fetal outcomes and hence such subclinical cases are not treated.
-
Q. So what is the reference ranges suggested by the new guidelines ?
- The guidelines recommend to use local reference ranges if available derived from healthy pregnant women who are TPO –ve and iodine sufficient.
- For typical patient in 1st Trimester from 7-12 weeks, the guidelines suggest TSH lower limit be reduced by 0.4 and upper limit reduced by 0.5 mIU/l from the nonpregnant reference range.
-
Q. HCG and TSH have a common alpha subunit or beta subunit?
- They have a common alpha subunit
-
Q. What happens to total T4 in pregnancy?
- It is 1.5 times the non-pregnancy range
-
Q. What type of free T4 assay gives false results in pregnancy ?
- Automated immunoassay for free T4 gives false results in pregnancy.
- Measurement of Free T4 by ultrafiltration and Equilibrium dialysis gives normal results, however they are expensive and time consuming.
-
Q. Why do automated assay for Free T4 fail to perform adequately in pregnancy ?
- Trimester specific cutoff for free T4 is not provided by most manufacturers.
- There is disruption of normal equilibrium between bound and free T4 in pregnancy. This is caused by increase in TBG and NEFA in pregnancy and reduction of albumin. Hence the current immunoassay fail dilutional assessment.
-
Q. What is the effect of Non-esterified fatty acids NEFA on free T4 ?
- NEFA displaces free T4 from TBG.
- This is the reason why heparin causes interference of thyroid function, because heparin increase production of NEFA which displaces Free T4 from TBG.
-
Q. What is done by manufacturers of analog immunoassay to counteract this effect of NEFA ?
- Manufacturers of analog immunoassay sometimes add albumin to the reagent to neutralize the effect of NEFA.
- This performs well in non pregnant patients but may causes issues in pregnancy.
-
Q. What is the gold standard for measurement of Free T4 in pregnancy ?
- Separation of Free T4 using equilibrium dialysis and measurement of Free T4 in the dialysate using LC-MS/MS.
-
Q. What is the method for adjusting the total T4 value based on non pregnancy range to pregnancy range ?
- <7 weeks- no change
- 7-16 weeks- increase the upper limit of total t4 of non pregnancy range by 5% per week starting from 7 weeks upto 16 weeks. (Eg: at 10 weeks increase the ULN by 15%)
- After 16 weeks – increase the ULN of normal by 50% (1.5 times ULN)
-
Q. Why is iodine requirement higher in pregnancy?
- Increase synthesis of thyroid hormone
- Increase urine excretion of iodine
- Increase metabolism of thyroid hormone
-
Q. What is the recommended iodine intake during pregnancy?
- WHO – 220 mcg
- IOM- 250 mcg in pregnancy and 290 mcg postpartum
-
Q. What is the tolerable upper limit for iodine intake?
- 600-1100 mcg
-
Q. Why is Urinary iodine concentration an epidemiological tool and not used for individual measurement ?
- The daily intake of iodine and UIC varies day by day.
- Hence UIC only gives an accurate estimation of iodine in the population and is not reliable to see the iodine status of an individual.
-
Q. What is the impact of mild to moderate iodine deficiency in pregnancy (defined as UIC 50-150 mcg/day) on mother, fetus and child ?
- Mother- increased risk of goiter and thyroid disorder
- Fetus- reduced fetal weight and neonatal head circumference
- Child- Attention deficit hyperactivity disorder and impaired cognitive outcomes
-
Q. Is iodine supplementation of mothers before pregnancy or early pregnancy beneficial ?
- Yes
- RCT have shown benefit of iodine supplementation in mothers with severe iodine deficiency on neonatal outcomes
-
Q. Is iodine supplementation in mothers with mild to moderate iodine deficiency useful ?
- It is controversial and studies have shown mixed results for both mother and child.
- The timing of supplementation may be crucial and better effects in child are seen if mother is supplemented before 10-20 weeks of gestation.
-
Q. What is recommendation as far as iodine supplementation in women planning to get pregnant is concerned ?
- For women planning for pregnancy it is recommend that they be supplemented with iodine in dose of 150 ug/day in form of potassium iodide to be taken atleast 3 months prior to conception.
- In regions where this is not feasible, pregnant women or women of child bearing age should be supplemented with single dose of 400 mg of iodized oil annually.
-
Q. What is the safe upper limit of iodine intake in pregnancy ?
- WHO recommends that iodine intake >500 mcg in pregnancy may be deemed as excessive.
-
Q. We know that iodine can induce thyroid autoimmunity. What dose of iodine can induce thyroid autoimmunity ?
- This depends on variable factors and importantly on historical intake of iodine.
- Those who have been exposed to high iodine from beginning are less likely to develop thyroid autoimmunity when iodine exposure is increased.
- Having said that, there is a U shaped curve of iodine intake and thyroid autoimmunity.
- Both low and high amount of iodine intake may have link with thyroid autoimmunity.
-
Q. Give the timeline for thyroid hormone synthesis in the fetus?
- 10-12th week – fetal TSH first appears
- 18th -20th week – a significant amount of thyroid hormone synthesis take place
-
Q. What happens to TSH after birth?
- Rapid rise to 50-80 mIU/ml after birth
- Comes to 10-15 within 48 hours
-
Q. What substances cross the placenta and what do not?
- TRH crosses the placenta
- TSH – does not cross the placenta
- Thyroid hormones- cross placenta- congenital agenesis patients have 20-50% of thyroid hormones compared to normal infant
- TRAb antibody – crosses the placenta
-
- TSH in the first trimester may be as low as 0.03
- Value <0.01 generally overt hyperthyroidism only
-
Q. What is the definition of overt hypothyroidism and subclinical hypothyroidism in pregnancy?
- Overt hypothyroidism- TSH above trimester-specific range and low T4
- Subclinical hypothyroidism- TSH above trimester-specific range with normal T4
-
Q. Should all women be screened for hypothyroidism in the first trimester?
- No
-
Q. What are the indications for screening for hypothyroidism in 1st trimester?
- ATA guidelines:
- Symptomatic women
- Previous history of hypothyroidism
- Previous evidence of TPO positive
- Family history of hypothyroidism
- Previous head and neck irradiation
- History of abortion
- History of preterm delivery
- Morbid obesity – BMI> 40
- Type 1 diabetes
- Coming from an area of moderate to severe iodine deficiency
- ATA guidelines:
-
Q. What percentage of the patient will be missed with this screening?
- 1/3rd of women
-
Q. What test should be done for screening?
- TSH is enough
- If TSH >2.5 in 1st trimester, then do T4
-
**TPO antibody positivity **
-
Q. What are risks associated with TPO antibody positive in pregnant women who are euthyroid (isolated TPO positive)?
- Spontaneous miscarriage
- Preterm delivery
- Large for gestational age
- Higher risk of developing subclinical hypothyroidism during pregnancy
- Higher risk of postpartum thyroiditis
-
- Even if within normal range, TSH is higher in TPO positive vs. TPO negative women
-
Q. Is there any effect on long-term cognitive behavior in children?
- A Netherlands study should increase the risk of Attention deficit hyperactivity disorder in children of TPO positive women
-
Q. Is there any recommendation to screen for or treat Euthyroid women with TPO positive?
- Presently no
- Only careful monitoring of thyroid function is recommended during pregnancy
- Some uptodate authors recommend treating with LT4 50 mcg in women who are euthyroid with Anti TPO positive and have a history of abortion
-
Q. How frequently to test thyroid function in euthyroid women who are TPO positive?
- Monitor TFT every month in 1st half of pregnancy and then at least once a trimester. In 2nd half of pregnancy
- If subclinical hypothyroidism develops – then treat
-
Q. Summarize the recommendation for euthyroid women with TPO positive?
- No evidence to treat
- Monitor TFT every month in 1st half and every trimester in 2nd half
-
**Goiter **
-
Q. Do pregnant women develop Goiter?
- In the absence of iodine deficiency, they should not develop goiter
- In areas of iodine deficiency, they develop goiter in up to 20-70% of cases
-
**Thyroid cancer **
-
Q. Do pregnant women diagnosed to have thyroid cancer in pregnancy have a worse prognosis?
- No
-
Q. Give the approach to thyroid cancer diagnosed during pregnancy?
- If thyroid cancer is diagnosed during pregnancy, monitor with ultrasound in each trimester
- If Thyroid cancer increases in volume by 50% or 20% in two dimensions by 24 weeks- perform surgery in 2nd trimester
- If Thyroid cancer does not increase in size or diagnosed after 2nd trimester, defer surgery till after pregnancy
- In cases that are not operated – keep TSH in the range of 0.1-1.5
-
Q. If surgery is performed, is there a higher risk of endocrine complications?
- Yes
- One study showed an increased risk of complications
-
Q. What is done in women previously diagnosed to have thyroid cancer and treated?
- Defer pregnancy till disease stabilized and at least 6 months after radioiodine therapy
-
Q. If a patient has low Tg and no residual tissue, is there a chance of recurrence in pregnancy?
- No
-
Q. if there is a residual disease, is there a chance of worsening in pregnancy?
- Yes
- Hence such cases, regular Tg and Ultrasound monitoring in each trimester of pregnancy is recommended
- Also, TSH suppression should be kept in the range as pre-pregnancy
- Patient may require a higher dose to achieve the same pre-pregnancy TSH suppression
-
Postpartum thyroid dysfunction
-
Q. What are the two types of thyroid dysfunction that occur postpartum?
-
- Postpartum thyroiditis
- Occurs in TPO positive women
- They develop transient Hyperthyroidism, then hypothyroidism, and then euthyroidism
-
- Postpartum worsening of Hashimoto's
- Occurs in women with a previous history of Hashimoto’s – there is worsening of hypothyroidism with increase LT4 requirement due to increased autoimmune activation
-
-
Q. What happens to Grave’s disease postpartum?
- It can worsen
- Even in patients with remission- it can relapse
-
Thyroid antibodies and pregnancy
(Also see 2. Hypothyroidism in pregnancy)
-
Q. Why is recommended that women with Anti TPO positive be kept on close surveillance with thyroid dysfunction during pregnancy ?
- Negro et al and other have observed that women with Positive Anti TPO antibody are more likely to have rapid increase in TSH during pregnancy and may develop overt hypothyroidism in pregnancy.
- Hence they are to be kept under close surveillance during pregnancy.
-
Q. What is the recommendation for TFT assessment in women who are anti TPO positive and become pregnant ?
- Women with Anti TPO positive who become pregnant should undergo thyroid function test every 4 weeks during pregnancy starting from time of pregnancy confirmation to mid-pregnancy.
-
Q. Does Anti TPO and Anti Tg antibody cross the placenta ?
- Yes.
- They do cross the placenta and the cord blood Anti TPO correlates with the maternal Anti TPO antibody in the 3rd trimester.
- However, this anti TPO has not been associated with thyroid dysfunction in the fetus.
-
Q. Is there any benefit of selenium supplementation in women who are anti TPO positive ?
- Some studies have shown that selenium supplemenation may lead to reduction of anti TPO antibody levels.
- However, this is not consistently found in all studies.
- Also the effect of selenium is also dependend on the iodine status and hence the results cannot be generalized to all population.
- Additionally, selenium is known to increase risk of development of type 2 diabetes mellitus.
- Hence, seeing the risk benefit, it is currently not recommended to supplement selenium in these patients.
-
Q. Is there a link between Anti TPO positivity and sporadic or recurrent pregnancy loss in euthyroid women ?
- The link between Sporadic spontenous pregnancy loss and Anti TPO antibody is clearly seen.
- The link between recurrent spontaneous pregnancy loss and anti TPO also does exist but data is less robust.
-
Q. What are the potential mechanism by which anti TPO antibody positivity is associated with increase spontenous pregnancy loss ?
- 1. Studies have shown than anti TPO positivity is associated with high likelihood of having APLA syndrome with anticardiolipin antibody being positive. Hence it may be APLA which may be causing the loss and not anti TPO itself.
- 2. Cross reaction of anti TPO antibody with HCG receptors on zona pellucida
- 3. Presence of non specific autoimmunity
- 4. Antibody mediated mild thyroid hypofunction.
-
Q. What are the potential treatment options for preventing spontenous pregnancy loss in women with Anti TPO antibody positivity ?
- Two options are proposed.
- One is administration of low dose of thyroxine in dose of 25-50 mcg/day.
- Second is use of IVIG.
-
Q. What is the recommendation of this guidelines as far as treatment of anti TPO is concerned ?
- Guidelines donot recommend the use of IVIG.
- The guidelines suggest that women with Anti TPO antibody positive and history of prior spontaneous pregnancy loss should be given LT4 in dose of 25-50 mcg/day. (Weak recommendation)
-
Q. Is thyroid antibody positivity associated with increase risk of Preterm delivery ? Does therapy with LT4 reduce this risk ?
- Yes. There is sufficient evidence to suggest that thyroid antibody positivity is associated with increase risk of preterm delivery.
- However, evidence to suggest that treatment with this reduces the risk is lacking.
- Hence the guidelines give no recommendation to use of LT4 to prevent preterm delivery in TSH receptor positive women to prevent preterm delivery.
-
Q. Which other diseases have been implicated in children of mothers having TPO positive and Euthyroid during pregnancy ?
- Increase risk of autism
- Attention deficit hyperactivity syndrome
- Sensorineural hearing loss.
Please consider donating to "Notes in Endocrinology" to keep us going. Please visit our DONATION page to know more