-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Q. What is the definition of subclinical hypothyroidism?
-
- Free T4 and Free T3 are normal
-
- TSH is above the upper limit of normal for the age, gender, and clinical situation
-
- Symptoms of hypothyroidism may or may not be present
-
-
Q. What is the prevalence of subclinical hypothyroidism in India?
- It is around 8-9%

-
Q. What is the most common cause of subclinical hypothyroidism?
- Hashimoto's thyroiditis
-
Q. Is one TSH level enough to confirm the diagnosis?
- No
- To label a person as having Subclinical hypothyroidism at least 1-2 times, the TSH must be repeated over a period of 1-3 months
-
Q. Does the TSH level increase with age?
- Yes
- TSH levels tend to increase with age
- A level of 6-8 mIU/l may be considered normal in older individuals
-
Q. What are the differential diagnosis of subclinical hypothyroidism?
-
- Heterophile antibodies
-
- Macro TSH
-
- Recovery from illness- recovery of the sick euthyroid syndrome can cause transient TSH elevation
-
- Recovery from subacute/destructive thyroiditis
-
- TSH producing adenoma
-
- Untreated adrenal insufficiency
-
- Central hypothyroidism - 25% of cases may have mildly elevated TSH
-
- Obesity
-
- Resistance to thyroid hormones
-
- Assay variability
-
- Rheumatoid factors
-
-
Q. What are the various analytical interferences that one has to be aware of in Endocrinology?
- Endogenous Antibodies
- Heterophilic antibodies
- Anti-animal antibodies ( HAMA )
- Autoantibodies. eg: Macroprolactin, RA factor
- Therapeutic antibodies
- Cross- reactant
- Similar proteins (Drugs & and their metabolites)
- Alkaline phosphatase
- Biotin (Exogenous factors)
- Endogenous Antibodies
-
Q. What are Heterophilic antibodies?
- Heterophilic antibodies are human antibodies that interact with assay antibody interferences.
- Heterophilic antibodies may arise in a patient in response to exposure to certain animals or animal products or due to infection by bacterial or viral agents, or non-specifically.
- If a patient is exposed to animals or animal products or suffers from an autoimmune disease, the patient may have heterophilic antibodies in circulation.
-
Q. Which are the most common Heterophilic antibodies?
- Among heterophilic antibodies, the most common are human anti-mouse antibodies HAMA because of the wide use of murine monoclonal antibody products in therapy or imaging.
-
Q. What is HAMA?
- It is a Human anti-mouse antibody
- It is a form of Heterophilic antibodies
- Human anti-mouse antibody or human anti-murine antibody (HAMA) is an antibody found in humans which reacts to immunoglobins found in mice.
- This is particularly important in Laboratory Endocrinology because most of the assays use mouse antibodies in their assays
- They mainly produce false-positive results
-
Q. Which are two everyday clinical situations where these antibodies cause false results?
-
- Tumor markers
-
- Endocrine assays
-
-
Q. What is the impact of Heterophilic antibodies on Sandwich assay or immunometric assays?
- In the sandwich-type immunoassays, heterophilic antibodies can form the“sandwich complex” even in the absence of the target antigen; this generates primarily false-positive results
- They mainly cause issues with large molecules like HCG and TSH etc. and generally do not impact competitive assay

-
Q. Do they cause false-negative results?
- False-negative results are generally rare
-
Q. What is the importance of correlation with urine tests in such cases (especially HCG)?
- Heterophilic antibodies are absent in urine.
- Therefore, if a serum specimen is positive for an analyte, for example, human chorionic gonadotropin (hCG), but beta-hCG cannot be detected in the urine specimen, it indicates interference from heterophilic antibodies in the serum hCG measurement.
-
Q. What is another common way to detect Heterophilic antibodies interference?
- If serial dilution produces a non-linear result, it indicates interference in the assay.
-
Q. How do commercial labs deal with the interference?
- Interference from heterophilic antibodies may also be blocked by adding any commercially available heterophilic antibody blocking agent in the specimen before analysis.
-
Q. Which tests are impacted by Heterophilic antibodies?
- TSH
- ACTH
- Calcitonin
- Thyroglobulin
- HCG
-
Q. What has the Rheumatoid factor got to do with this?
- Rheumatoid factor is a form of Heterophilic antibodies
- It is an autoantibody
- It cross-reacts with animal antibodies
-
Hence people with RA factor positive are more likely to have cross-reactivity and false values #Clinicalpearl
-
Q. What is an example of an autoantibody acting as a heterophile antibody in practice?
- Macroprolactin
- Macro- TSH
-
Q. How high can the TSH go in cases of Macro TSH?
- The TSH can be as high as >100
- It is found in 1.6% of patients labeled as overt hypothyroidism
-
Q. How do you diagnose Macro TSH?
- It is diagnosed by removing the IgG- TSH concentration using Polyethylene glycol precipitation
-
Q. Why is obesity associated with high TSH?
-
-
Q. Give the TSH cut-off based on BMI?
- <20 kg/m2 - 0.6 to 4.8 pUI/mL
- 20-24.9 kg/m2 - 0.6 to 5.5 JUI/mL
- 25-29.9 kg/m2 - 0.6 to 5.5 pUI/mL
- 30-39.9 kg/m2- 0.5 to 5.9 pUI/mL
- More 40 kg/m2 -0.7 to 7.5 pUI/mL
-
Clinical consequences of Subclinical hypothyroidism
-
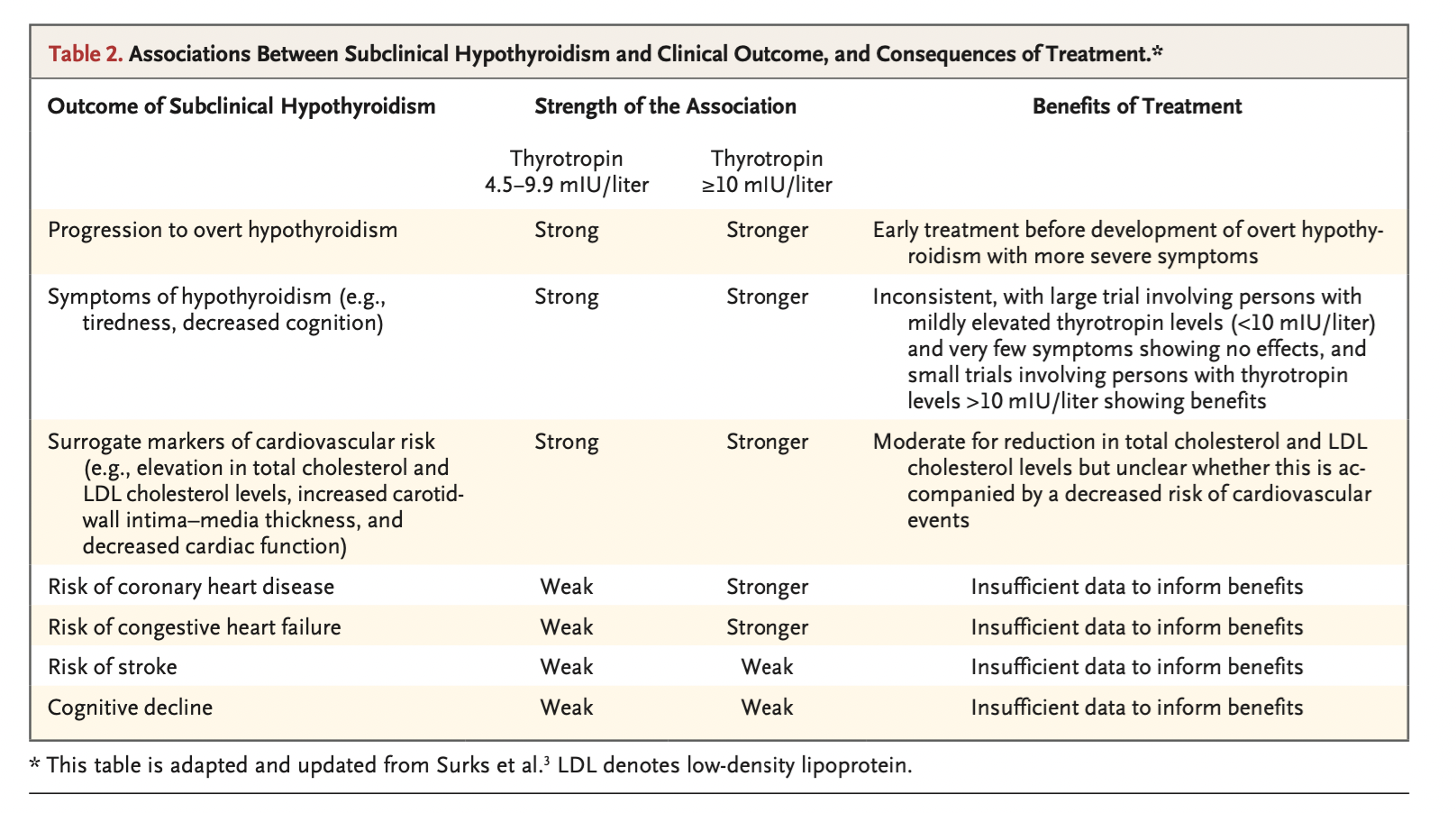
Q. Enlist the consequences of Subclinical hypothyroidism?
-
- Progression to Overt hypothyroidism
-
- Increased risk of cardiovascular disease
-
- Reproductive abnormalities and infertility
-
- NASH/NAFLD
-
- Neuropsychiatric symptoms
-
-
Q. What is the annual rate of progression from subclinical to overt hypothyroidism?
- 2-4% per year
-
Q. What are the factors on which conversion to overt hypothyroidism is dependent?
- It is dependent upon the initial TSH value (Higher the value- more likely to progress)
- Presence of Anti TPO antibody and Anti Tg Antibody - the presence of antibody - is more likely to progress
- Underlying cause- Autoimmune, Post Radioactive iodine therapy, surgery, etc
-
Q. Is spontaneous normalization possible?
- Yes
- in 62% of patients with TSH <10 - spontaneous normalization can occur within the first 2 years
-
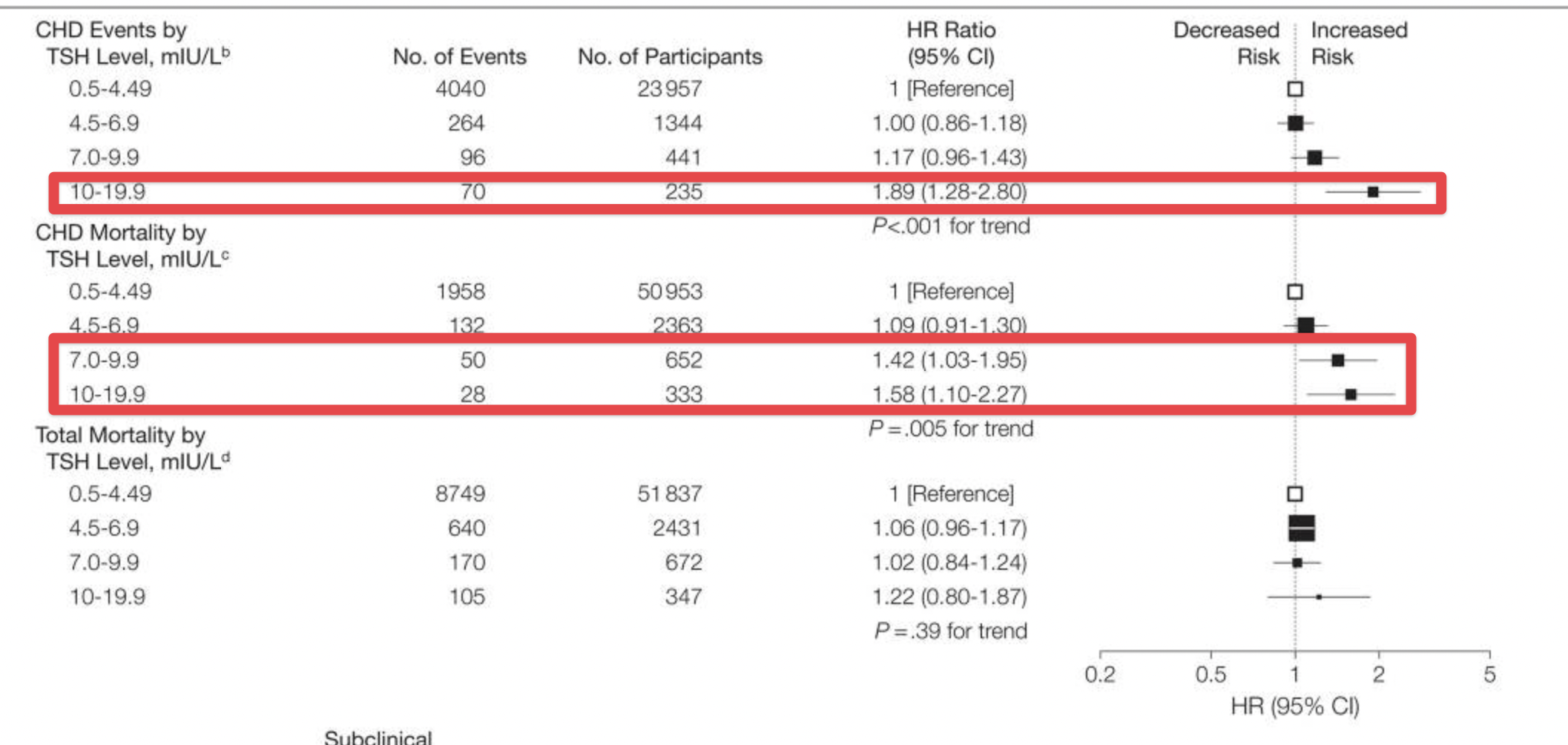
Q. Do patients with Subclinical hypothyroidism have an increased risk of cardiovascular disease?
- Yes
- This is mainly for those patients with TSH >10
- The hazards ratio is 1.89 (CI, 1.28-2,80) for CHD events in patients with TSH >10, according to a meta-analysis by Rodondi et al [1]
-
Q. Based on the TSH values, what are the Hazard ratio of Cardiovascular mortality based on the meta-analysis by Rodondi et al. [2] ?
- TSH - 4.5-6.9 -HR- 1.09 (CI, 0.91-1.30)
- TSH - 7-10 - HR- 1.42 (CI, 1.03-1.95)
- TSH - 10-19.9 - HR- 1.58 (CI, 1.10-2.27)
-
Q. Is there a relation between Subclinical hypothyroidism and Heart failure?
- Yes
- Again, for patients with TSH >10- there is an increased risk of developing heart failure (HR-1.86, CI- 1.27-2.72)
- The risk is increased in TSH of 7-9.9, but it is NOT statistically significant
-
Q. Is there a correlation between Subclinical hypothyroidism and stroke?
- Yes
- There is a correlation between Subclinical hypothyroidism and stroke.
- However, it is limited to a relatively younger age group, 18-65 years of age. The same was not seen in the older age groups
-
Q. What is the impact of Subclinical hypothyroidism on lipid profile?
- It is well known that Subclinical untreated hypothyroidism is associated with higher LDL-C levels
-
Q. Is there an increased risk of mortality in patients with Subclinical hypothyroidism?
- The data is conflicting because of the contradictory nature of studies
- Broadly, there is undoubtedly increased cardiovascular mortality in patients with TSH >10
- However, in older individuals with TSH <10, treatment is associated with higher mortality compared to no-treatment
- Hence both the age and the TSH level has to be taken into consideration for looking at the mortality parameters
-
Q. What is the correlation between subclinical hypothyroidism and reproductive abnormalities in women?
- For this, please see Female Infertility and Thyroid dysfunction
-
Q. Is there a correlation between NASH/NAFLD and hypothyroidism?
- Yes
- Both Subclinical hypothyroidism as well as Overt hypothyroidism is associated with an increased likelihood of having NASH/NAFLD
- Also, amongst patients with NASH, the presence of hypothyroidism is associated with increased progression of fibrosis and development of cirrhosis
-
Q. Is there a correlation between subclinical hypothyroidism and depression?
- For this, please see Hypothyroidism and Depression (Coming soon)
-
Q. Summarize the clinical consequences of Subclinical hypothyroidism
-
Treatment of Subclinical hypothyroidism
-
Q. Summarize the treatment algorithm for Subclinical hypothyroidism based on the NEJM review article and current evidence?
-
Q. Give the algorithm from UptoDate
-
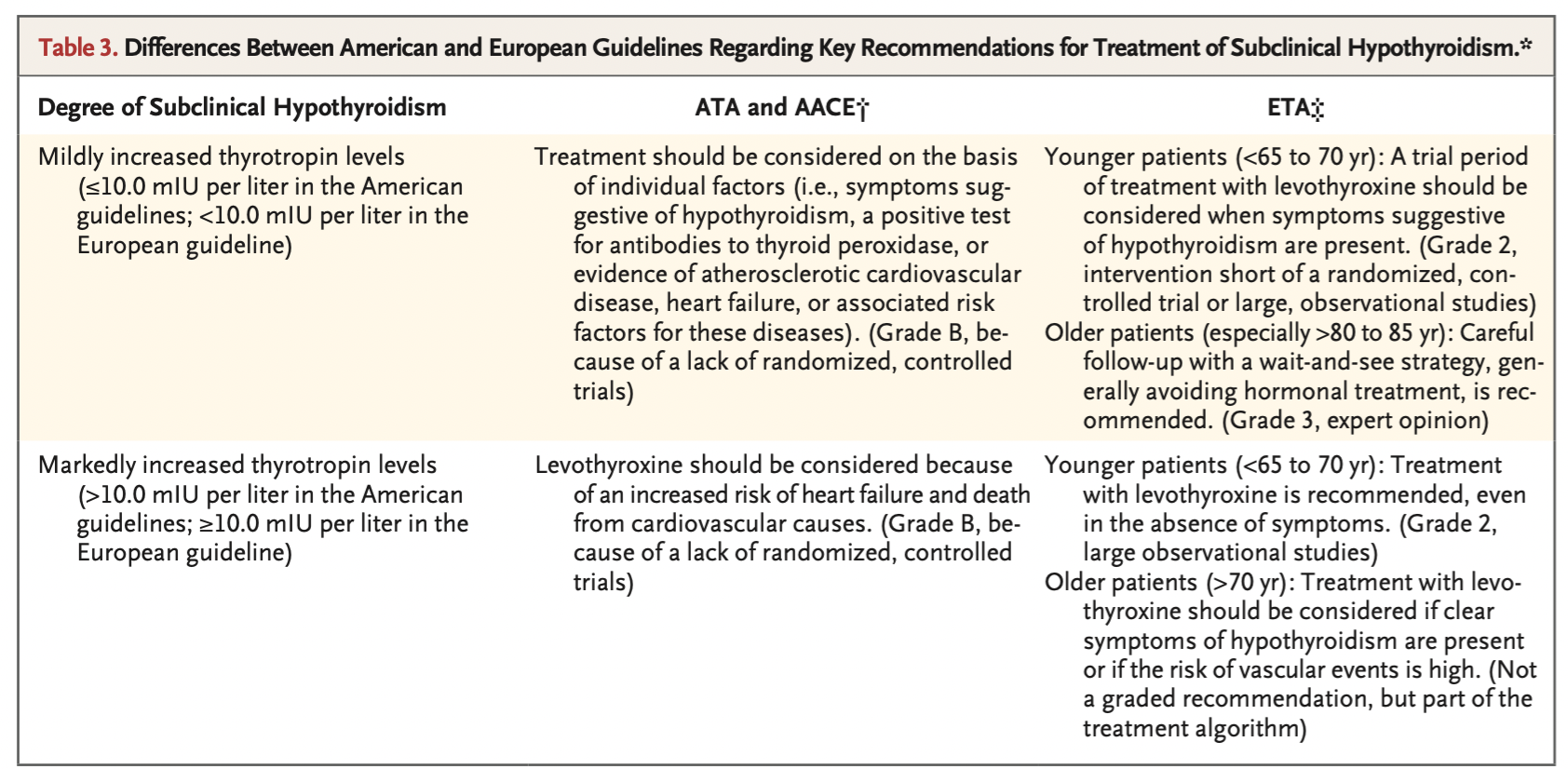
Q. Summarize the recommendations from the ETA and ATA guidelines for subclinical hypothyroidism?
-
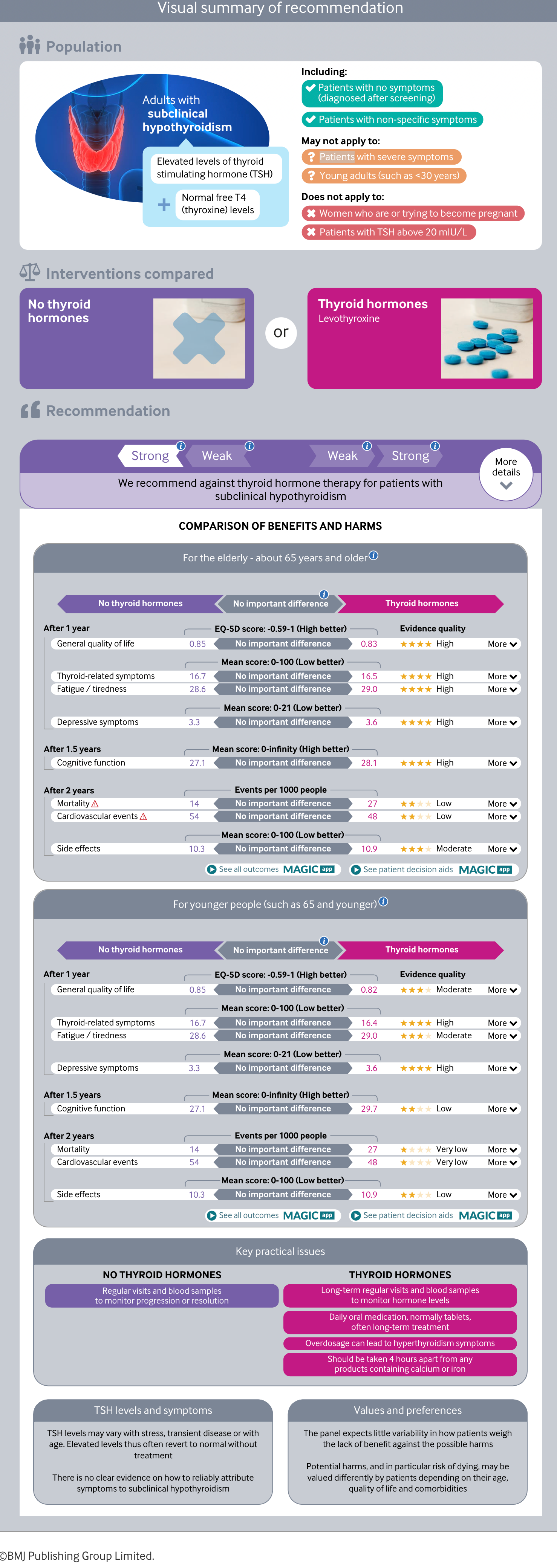
Q. What do the BMJ guidelines on subclinical hypothyroidism recommend?
- The BMJ guidelines published in 2019 suggest that NO TREATMENT SHOULD BE GIVEN FOR SUBCLINICAL HYPOTHYROIDISM [3]
- These guidelines as applicable for
- Patients with no symptoms (diagnosed after screening)
- Patients with non-specific symptoms
- These guidelines do not apply for
- Patients with severe symptoms
- Young adults (such as <30 years)
- Women who are or trying to become pregnant
- Patients with TSH above 20 mlU/L
-
Q. Assuming the patient is "symptomatic" and has a TSH <10, does the treatment with LT4 reduce the symptoms?
- No
- Clinical trials have shown no benefit in the "symptoms" or quality of life on treatment with LT4 in patients with Subclinical hypothyroidism and TSH <10
-
Q. What about patients having TSH >10?
- Those with TSH >10 and having symptoms- there is improvement in symptoms according to several guidelines and recommendations
-
Q. Is there a reduction in goiter size in patients having goiter and Subclinical hypothyroidism?
- Yes
- There is an 80% reduction in goiter size in patients with Subclinical hypothyroidism having a goiter
-
Q. Is there any evidence or improvement in cardiovascular outcomes in patients with subclinical hypothyroidism treated with LT4?
- As discussed above, there is a correlation between Subclinical hypothyroidism and cardiovascular disease, especially in those patients with TSH >10.
- However, treatment with LT4 to reduce the cardiovascular risk has NOT been demonstrated in any RCT
- This is the fundamental flaw
- However, observational studies have shown benefit and improvement in cardiovascular outcomes, mainly in adults <70 years of age
- However, the data is often conflicting
-
Q. Do we see improvement in the lipid profile in patients with Subclinical hypothyroidism treated with Levothyroxine?
- In patients with TSH >10, RCT has shown improvement in the LDL and Apo B-100 levels for patients treated with levothyroxine
-
Q. Name two significant but under-recognized outcomes of treating Subclinical hypothyroidism?
-
- Trails have shown improvement in the renal function in patients with Subclinical hypothyroidism and CKD treated with Levothyroxine
-
- Patients with Subclinical hypothyroidism and iron deficiency anemia have an improvement in hemoglobin levels when treated with Levothyroxine
-
-
Q. Which group of patients with Subclinical hypothyroidism MUST be treated?
- All patients with TSH >10, irrespective of age, must be considered for treatment with Levothyroxine
-
Q. What about those patients with TSH of 7-9.9 mIU/l?
- Younger patients (<70 years of age) with TSH of 7-9.9 must be treated
- Treatment with LT4 does provide cardiovascular benefit to some extent in this group of patients
- However, for those of >70 years of age, treatment pro and cons of treatment with LT4 must be looked at closely
-
Q. What about those patients with TSH of 5-6.9 mIU/l?
- Patients >70 years of age with the above TSH levels MUST NOT be treated
- Selected patients with TSH <70 years may be treated. These include
- Those with goiter
- Those with high titer of Anti TPO antibody or Anti Tg Antibody
-
Q. What about those women with infertility?
- Please see Female Infertility and Thyroid dysfunction
-
Q. What should be the dose of Levothyroxine if treatment IS considered?
- In older individuals - we can start with lower doses of 25-50 mcg/day and up titrate if required
- In younger patients- a total replacement dose of 1.5-1.6 mcg/kg/day may be considered
- In our center, we start with a 1 mcg/kg dose (as per ETA recommendation)
-
Q. What should be the TSH target?
- younger symptomatic individuals- target TSH <2.5-3.0
- Older individuals TSH 3.0-6.0 mIU/l
-
Q. How is the dose titrated?
- Typically, the TSH levels are measured again after six weeks
- Those with TSH more than target the dose of Levothyroxine may be increased by 12.5-25 mcg
- If the TSH is lower, the dose is reduced in similar proportions
-
Q. Summarize the treatment recommendations for Subclinical hypothyroidism as per your expert views, guidelines, and current recommendations?
Rodondi N, Den Elzen WP, Bauer DC, Cappola AR, Razvi S, Walsh JP, Åsvold BO, Iervasi G, Imaizumi M, Collet TH, Bremner A. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. Jama. 2010 Sep 22;304(12):1365-74. ↩︎
Rodondi N, Den Elzen WP, Bauer DC, Cappola AR, Razvi S, Walsh JP, Åsvold BO, Iervasi G, Imaizumi M, Collet TH, Bremner A. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. Jama. 2010 Sep 22;304(12):1365-74. ↩︎
Bekkering GE, Agoritsas T, Lytvyn L, Heen AF, Feller M, Moutzouri E, Abdulazeem H, Aertgeerts B, Beecher D, Brito JP, Farhoumand PD. Thyroid hormones treatment for subclinical hypothyroidism: a clinical practice guideline. Bmj. 2019 May 14;365 ↩︎