- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
-
Q. What is the definition of Refractory hypothyroidism?
- Refractory hypothyroidism is defined as the presence of biochemical signs (serum TSH > 4.5 mU/L, 6 weeks after the dose increase) or clinical hypothyroid symptoms of an LT4 dose > 1.9 μg/kg/day. Some other definitions have used a cutoff of > 2.5 mcg/kg.
- It is a clinical challenge often encountered, even though hypothyroidism is generally considered an easy condition to manage.
- Truly refractory hypothyroidism only accounts for a small proportion of refractory cases, with the remainder being "pseudo-refractory."
-
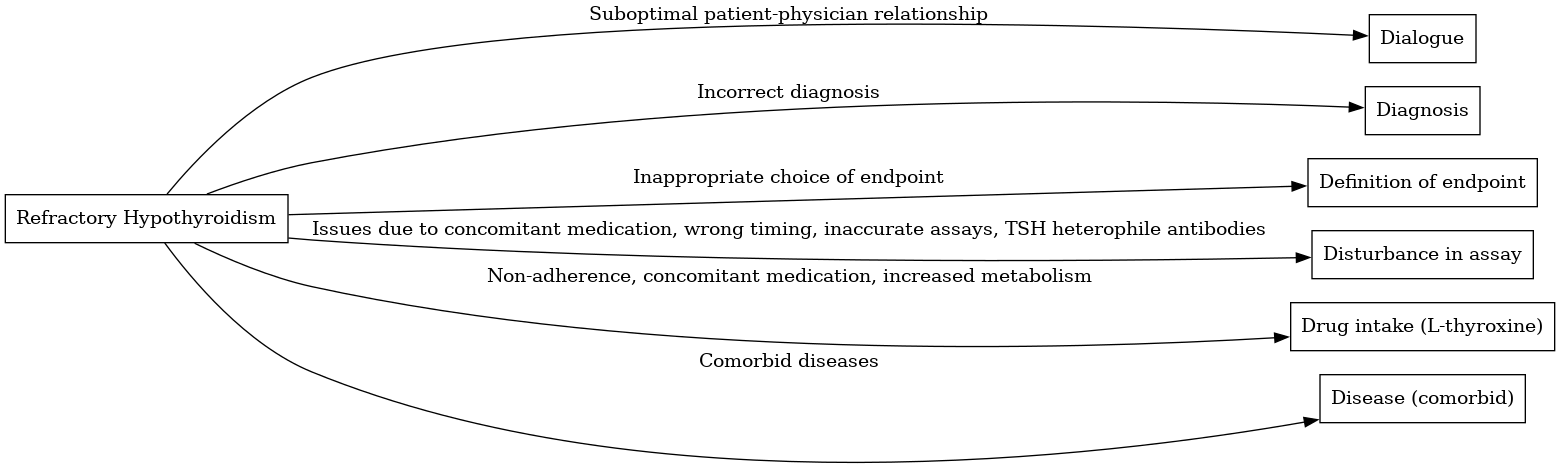
Q. What are the 6 D's of refractory hypothyroidism?
- Dialogue: This refers to the suboptimal relationship between patient and physician, leading to poor adherence or persistence in treatment.
- Diagnosis: Incorrect diagnosis of the disease can lead to refractory hypothyroidism. For example, the inability to recognize central hypothyroidism, sick euthyroid syndrome, obesity-related thyroid dysfunction, thyroid resistance, and pregnancy physiological increased demands.
- Definition of endpoint: Inappropriate choice of endpoint can contribute to refractory hypothyroidism. For instance, testing TSH at short intervals, testing only TSH in central hypothyroidism, and testing T4 in states of hypoalbuminemia.
- Disturbance in assay: This can occur due to concomitant medication like biotin, wrong timing of sampling, use of inaccurate assays, and the presence of TSH heterophile antibodies.
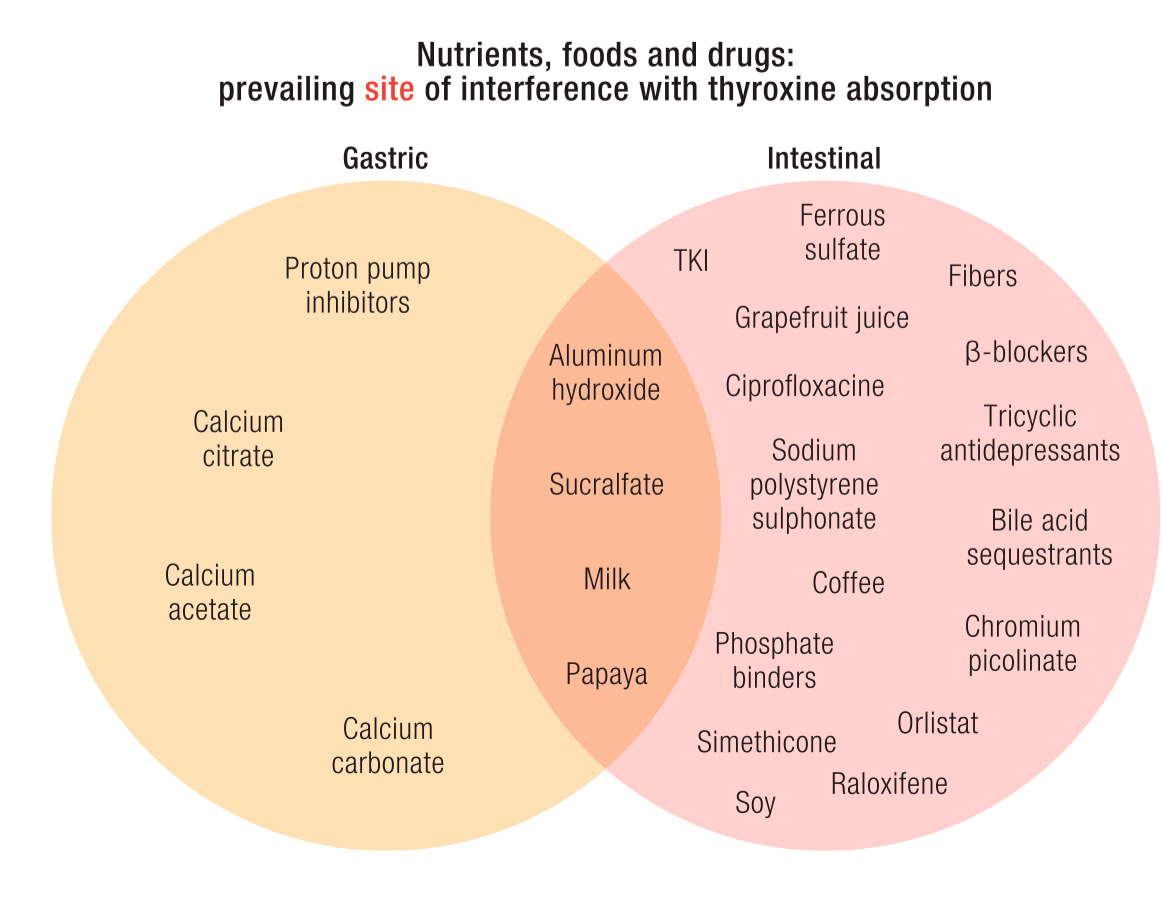
- Drug intake (L-thyroxine): Lack of adherence to the suggested therapeutic regimen, concomitant administration of medication that may impair absorption (antacids, iron, calcium), or increase the metabolism of L-thyroxine can lead to refractory hypothyroidism.
- Disease (comorbid): Comorbid diseases, such as malabsorption syndromes, renal/liver impairment, and hypocortisolemia, can contribute to refractory hypothyroidism.
-
Q. Which is the most common cause of Refractory hypothyroidism?
- Noncompliance with therapy
- As much as 50% of patients are partially or completely non-compliant with treatment.
-
Q. How is Levothyroxine absorbed from the GI tract?
- Levothyroxine (LT4) absorption primarily occurs in the small intestine, specifically in the jejunum and ileum.
- The process is an active one, facilitated by transporters such as monocarboxylate transporter 8 (MCT8) and organic anion-transporting polypeptide 1C1 (OATP1C1).
- The absorption process is most efficient in a fasting state. Food and certain medications can interfere with LT4 absorption.
- Calcium salts, iron salts, aluminum salts, and bile acid sequestrants are known to impair LT4 absorption.
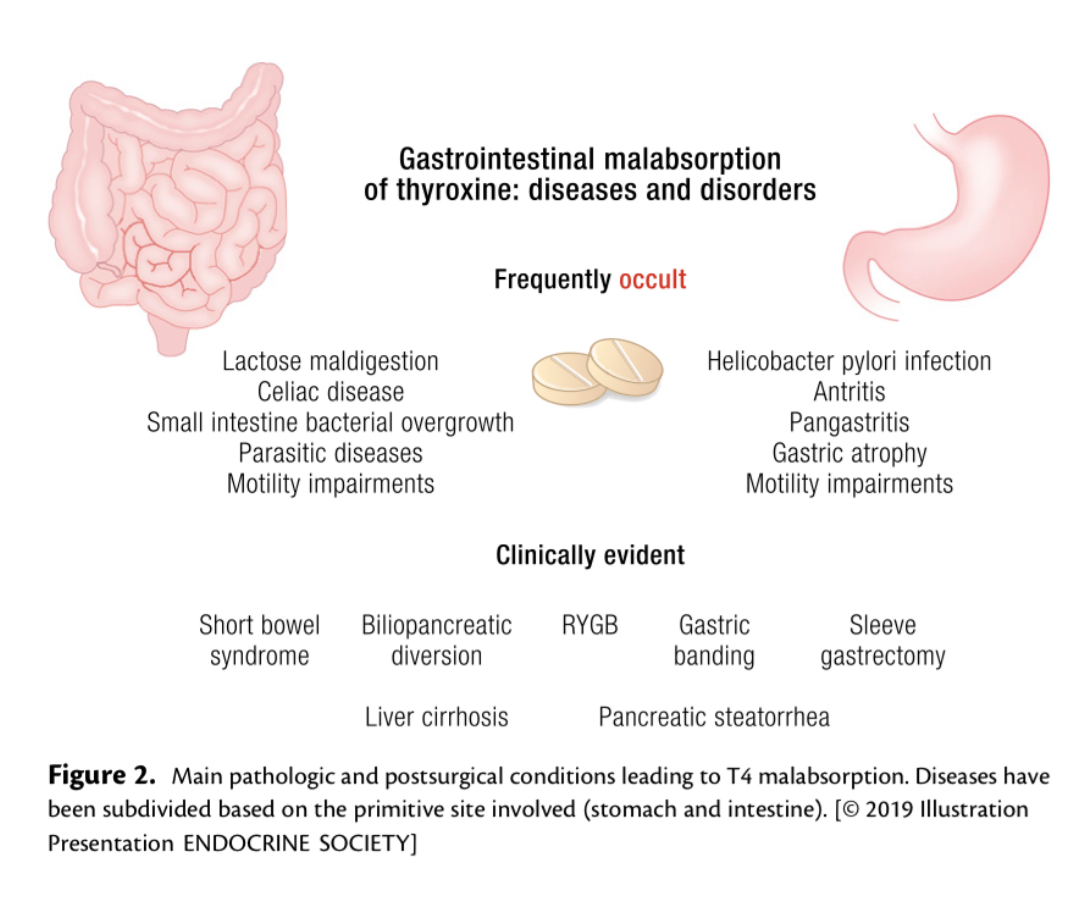
- Gastrointestinal disorders such as Helicobacter pylori infection, gastritis, celiac disease, lactose intolerance, and biliary/pancreatic disorders can also affect LT4 absorption.
- LT4 absorption can be unpredictable, varying drastically between individuals and even within the same individual at different times.
a
-
Q. What percentage is absorbed from what part of the GI Tract?
-
Q. Give the step-by-step process for Oral absorption for T4?
-
Q. LT4 falls in which biopharmaceutics classification category?
- Levothyroxine, a thyroid hormone replacement therapy, is an example of a Class III drug.
- In the Biopharmaceutics Classification System (BCS), a Class III drug is characterized by:
- High solubility: This means the drug readily dissolves in gastrointestinal fluids, facilitating its absorption into the body.
- Low permeability: This refers to the drug's limited ability to cross biological membranes, such as the intestinal wall, which can hinder its absorption into the systemic circulation.
-
Q. How is LT4 absorbed via the small intestine - is it via passive diffusion or is it via active transport?
- The absorption of Levothyroxine (LT4) in the small intestine is not solely via passive diffusion, as was previously thought due to the high lipophilicity of the molecule.
- Current understanding indicates that LT4 absorption involves active transport mechanisms.
- Different categories of transporters act as LT4 carriers at the level of the small intestine. These include the monocarboxylate transporter (MCT) family, the organic anion-transporting polypeptide (OATP) family, the ATP-binding cassette transporter superfamily, and the large neutral amino acid transporter family.
- Two MCTs involved in LT4 transport have been identified in the small intestine mucosa: MCT8 and MCT10. Both of these transporters are responsible for cellular influx and efflux of LT4.
- MCT8, the primary transporter of thyroid hormone, is expressed in many tissues, but its activity is mainly devoted to thyroid hormone transport across the blood-brain barrier and to the development of the human brain.
- Therefore, the absorption of LT4 in the small intestine is a complex process involving both passive diffusion and active transport mechanisms.
-
Q. Of MCT8 and MCT10, which is more likely to be involved in the intestinal transport?
- Both MCT8 and MCT10 are involved in the transport of thyroid hormones, but their roles differ in various tissues.
- MCT8 is the primary transporter of thyroid hormone and is expressed in many tissues. Its activity is mainly devoted to thyroid hormone transport across the blood-brain barrier and to the development of the human brain.
- However, a specific localization of MCT8 in the human intestine has not been identified, and its possible functions have not been extensively studied.
- On the contrary, MCT10 is highly expressed at the small intestine level and, in particular, in the basolateral membrane of mucosal cells. This leads to the hypothesis of its possible role in the intestinal T4 resorption.
- Therefore, based on current knowledge, MCT10 is more likely to be involved in the intestinal transport of thyroid hormones.
-
Q. How does transport of thyroid hormone via OATP1A2 explain its potential interactions?
- Organic anion-transporting polypeptide 1A2 (OATP1A2) is a transporter protein that plays a significant role in the absorption, distribution, and elimination of a wide range of drugs, including thyroid hormones.
- OATP1A2 is expressed in various tissues, including the small intestine, which is a primary site for drug absorption.
- Thyroid hormones are substrates for OATP1A2, meaning they can bind to and be transported by this protein.
- The interaction of thyroid hormones with OATP1A2 can be influenced by other substances that also use this transporter. For instance, certain drugs, dietary components, and herbal supplements can compete with thyroid hormones for binding to OATP1A2, potentially affecting the absorption and bioavailability of the hormones.
- Beta-blockers and tricyclic antidepressants, for example, have been found to use the same transporter, which could lead to a novel site of interaction with thyroid hormones.
- Flavonoids such as naringin and hesperidin, components of grapefruit and orange juice, respectively, may interfere with OATP1A2, affecting the oral availability of its substrates, including thyroid hormones.
- Therefore, understanding the role of OATP1A2 in thyroid hormone transport can help predict and manage potential drug-drug or drug-food interactions that could impact thyroid hormone levels in the body.
-
Q. How do the intestinal microbiota contribute to LT4 absorption?
- The intestinal microbiota plays a significant role in the metabolism of thyroid hormones, including Levothyroxine (LT4), through several mechanisms:
- The intestinal microbial flora allows the binding of iodothyronine, creating a hormonal reservoir. This reservoir can serve as a source of thyroid hormones, contributing to the overall pool available for absorption.
- The intestinal microbiota also possesses sulfatase and glucuronidase activities. These enzymes can deconjugate thyroid hormones that have been conjugated with sulfuric and glucuronic acid in the liver, making them more soluble and allowing their renal and biliary clearance.
- After deconjugation by the intestinal microbiota, these hormones can potentially be reabsorbed into the bloodstream through the hepatic portal circulation, contributing to the overall levels of thyroid hormones in the body.
- Changes in the intestinal microbiota, known as dysbiosis, can affect these metabolic steps. Dysbiosis may alter the balance of bacterial species that possess sulfatase and glucuronidase activities, potentially affecting the deconjugation and reabsorption of thyroid hormones.
- Therefore, the intestinal microbiota plays a crucial role in the absorption and metabolism of LT4, and changes in the microbiota can potentially impact LT4 levels in the body.
-
Q. What should be the gap between Levothyroxine medication and food and other medications?
- Food: Gap of 1 hour
- Other medication: Gap of 4 hours
-
Q. What type of pH is required for GI absorption of Levothyroxine?
- LT4 absorption is highly dependent on gastric pH. An acidic environment in the stomach is necessary for LT4 to dissolve before it can be absorbed in the small intestine.
-
Q. How much of the oral levothyroxine is absorbed in optimal conditions?
- It's estimated that approximately 60-80% of an oral dose of LT4 is absorbed under optimal conditions.
-
Q. True or false, there is increased absorption seen in overt hypothyroidism?
- True
-
Q. How does the absorption issue explain the increased requirement during pregnancy?
-
Q. Is there any impact of T4 absorption with aging ?
- Yes with aging T4 absorption is reduced
- There is 4% reduction in T4 absorption with every 10 years of age
- However, this is an area of debate
-
Q. What are the important GI conditions that impede the absorption of levothyroxine from the GI tract ?
- Celiac Disease: This autoimmune disorder damages the small intestine lining, impairing the absorption of levothyroxine.
- Gastroparesis: Delayed gastric emptying can affect the dissolution and absorption of levothyroxine.
- Lactose Intolerance: Some formulations of levothyroxine contain lactose, which can hinder absorption in individuals with lactose intolerance.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn's disease and ulcerative colitis can affect the absorption of levothyroxine due to inflammation and damage to the intestinal lining.
- Short Bowel Syndrome: This condition results in less functional small intestine surface area, reducing the absorption of levothyroxine.
- Gastric Bypass Surgery: This weight loss surgery alters the anatomy of the stomach and small intestine, potentially affecting levothyroxine absorption.
- Biliopancreatic Diversion: This is another type of weight loss surgery that can interfere with levothyroxine absorption by reducing contact time with the intestinal mucosa.
- Atrophic Gastritis and Helicobacter pylori Infection: These conditions decrease gastric acid production, which is necessary for levothyroxine dissolution and absorption.
-
Q. What are the potential screening tests for refractory hypothyroidism ?
- Malabsorption Syndromes: Anti-tissue transglutaminase antibodies test and endoscopic biopsy can be used to screen for conditions like celiac disease that can affect levothyroxine absorption.
- Atrophic Gastritis: Gastroscopy with biopsy, gastric pH, gastric acid measurement, and parietal cell antibody/intrinsic factor antibody tests can be used to diagnose this condition which can affect the stomach's ability to produce acid necessary for levothyroxine absorption.
- Helicobacter pylori Infection: Invasive methods such as histology, culture, and rapid urease test on endoscopic biopsy specimens can be used. Noninvasive tests such as urea breath test and stool antigen test can also be used to diagnose this infection which can affect gastric acid production.
- Renal/Liver Disease: Renal function tests, liver function tests including serum albumin, and urine albumin: creatinine ratio can be used to screen for these conditions which can affect the metabolism and clearance of levothyroxine.
- Addison's Disease: 8 am serum cortisol and adrenocorticotropic hormone (ACTH) levels can be used to screen for this condition which can affect the body's response to stress and can coexist with autoimmune thyroid diseases.
-
Q. How is H. pylori infection diagnosed ?
- H. pylori infection is initially screened as it is the most prevalent disorder.
- Diagnostic methods include a 14C-urea breath test or fecal H. pylori antigen detection.
- Measurement of antibodies against H. pylori is also performed.
- If the tests are positive, the involvement of gastric mucosa is investigated by endoscopy with multiple biopsies.
- After appropriate treatment, if the symptoms persist, the H. pylori infection is re-evaluated.
-
Q. Enlist the various breath tests used in diagnosis of GI disorders ?
-
- Hydrogen breath test: This test is used to diagnose lactose intolerance and small intestine bacterial overgrowth (SIBO).
-
- Methane breath test: This test is used to diagnose constipation related to SIBO.
-
- Carbon-14 urea breath test: This test is used to diagnose Helicobacter pylori infection, a bacterial infection that causes ulcers.
-
- Fecal breath test: This test is used to diagnose digestive disorders such as inflammatory bowel disease (IBD) and colon cancer.
-
- Volatile organic compound (VOC) breath test: This test is used to diagnose various GI disorders such as IBD, colitis, and Crohn’s disease.
-
- Fructose breath test: This test is used to diagnose fructose malabsorption, a condition where the body has difficulty digesting fructose.
-
- Lactulose breath test: This test is used to diagnose bacterial overgrowth in the small intestine.
-
- Glucose breath test: This test is used to diagnose bacterial overgrowth in the small intestine.
- Of the above 4 are most important:
- Urea breath test- H. pylori
- Lactose breath test- Lactose intolerance
- Glucose breath test- bacterial overgrowth
- Lactulose breath test- altered gut transit time
-
-
Q. How is autoimmune gastrtis diagnosed ?
- Autoimmune gastritis is suspected when there are high serum gastrin levels and the presence of anti-parietal cell antibodies (anti-PCAs).
- Endoscopy with multiple biopsies of the gastric body and antrum is strongly suggested to confirm the diagnosis.
- The biopsies help in identifying the atrophic changes in the gastric mucosa, which is a characteristic of autoimmune gastritis.
- In some cases, the presence of concurrent conditions like iron-deficient anemia or autoimmune hypothyroidism (as part of type III polyglandular autoimmune syndrome) may also point towards autoimmune gastritis.
-
Q. How are renal diseases associated with Refractory hypothyroidism ?
- Renal diseases can lead to decreased peripheral metabolism of T4 to T3: The kidneys play a significant role in the conversion of inactive T4 to active T3. In renal impairment, this conversion process can be hindered, leading to decreased T3 levels. This can make it difficult to optimize thyroid function even with higher doses of levothyroxine.
- Decreased thyroxine-binding proteins: In conditions like nephrotic syndrome, there can be a decrease in thyroxine-binding proteins such as albumin. This can affect the volume of distribution of levothyroxine, making it less available for use by the body.
- Altered drug pharmacokinetics: Renal diseases can affect the absorption, distribution, metabolism, and excretion of drugs, including levothyroxine. This can lead to suboptimal drug levels and response.
- Co-existing autoimmune diseases: Autoimmune thyroid diseases and certain renal diseases, such as IgA nephropathy and membranous nephropathy, often coexist due to shared autoimmune mechanisms. This can complicate the management of hypothyroidism.
- Electrolyte imbalances: Renal diseases can lead to electrolyte imbalances, such as hyponatremia, which can affect thyroid hormone function and contribute to refractory hypothyroidism.
-
Q. How is liver dysfunction associated with Refractory hypothyroidism ?
- Impaired Conversion of T4 to T3: The liver plays a crucial role in the conversion of inactive T4 to active T3. Liver dysfunction can impair this conversion, leading to decreased levels of T3, which can be difficult to optimize even with increased doses of levothyroxine.
- Altered Thyroxine-Binding Proteins: Liver diseases, especially severe cirrhosis, can lead to a decrease in thyroxine-binding proteins such as albumin. This can affect the volume of distribution of levothyroxine, reducing its availability for use by the body.
- Altered Drug Metabolism: Liver dysfunction can affect the metabolism and clearance of drugs, including levothyroxine. This can lead to suboptimal drug levels and response, contributing to refractory hypothyroidism.
- Co-existing Autoimmune Diseases: Autoimmune thyroid diseases and certain liver diseases, such as autoimmune hepatitis, often coexist due to shared autoimmune mechanisms. This can complicate the management of hypothyroidism.
-
Q. Give the step-by-step process of Levothyroxine absorption test ?
- This is as per the protocol by Ghosh et al:
- The patient comes with an overnight fast.
- Levothyroxine (LT4) is administered in a dose of 10 mcg/kg or 600 mcg, whichever is lower.
- Blood samples are collected for baseline Free T4 (FT4) and TSH levels.
- Another blood sample is collected for Free T4, 3 hours after taking the medication.
- FT4 increase of >0.40 ng/dl after 3 hours has 97% sensitivity and 80% specificity for ruling out malabsorption.
- This is as per the protocol by Ghosh et al:
-
Q. Is there any other protocol for India ?
- Yes, by Subramaniam et al
- The patient comes with an overnight fast.
- Blood samples are collected for baseline Total T4 and TSH levels.
- Levothyroxine (LT4) is administered in a dose of 15 mcg/kg
- Hour samples of total T4 and TSH are taken for 5 hours
- The % absorption is calculated from the formula:
- % absorption = [[maximum increment in T4 (mcg/dL) × 10]/ total dose of thyroxine administered (mcg)] × Vd × 100
- Here, Vd represents the volume of distribution, which is calculated as BMI (in kg/m^2) × 0.442.
- Absorption >60% was considered normal
-
Q. Can allergy to excipients cause Refractory hypothyroidism ?
- Yes, allergies to excipients in levothyroxine tablets can potentially cause refractory hypothyroidism. Here are some key points:
- Excipients are inactive substances used as carriers for the active ingredients of a medication. In some cases, patients may have an allergic reaction or sensitivity to these excipients, which can interfere with the absorption of the active ingredient, in this case, levothyroxine.
- If a patient is allergic to an excipient in a levothyroxine tablet, it could lead to poor absorption of the medication, resulting in persistently high TSH levels despite adequate dosing. This situation could be misinterpreted as refractory hypothyroidism.
- It's important to consider this possibility in patients with persistent hypothyroid symptoms and high TSH levels despite taking what should be adequate doses of levothyroxine.
- If an allergy to an excipient is suspected, switching to a different brand of levothyroxine, or to a liquid or gel cap formulation that contains fewer excipients, may help improve absorption and thyroid hormone levelss
- Yes, allergies to excipients in levothyroxine tablets can potentially cause refractory hypothyroidism. Here are some key points:
-
Q. In the above article by Subramaniam et al, what tests were done if absorption was <60% ?
- In the study by Subramaniam et al, if the calculated levothyroxine absorption was ≤60%, indicating potential malabsorption, the following tests were performed:
- Fasting serum gastrin test: This test measures the level of gastrin in the blood. High levels can indicate certain medical conditions including autoimmune gastritis.
- Helicobacter pylori – immunoglobulin G test: This test is used to detect antibodies against Helicobacter pylori, a bacteria that can cause infections in the stomach.
- Tissue transglutaminase – immunoglobulin A test: This test is used to detect antibodies against tissue transglutaminase, which can indicate celiac disease.
- Total Immunoglobulin A test: This test measures the amount of Immunoglobulin A (IgA) in the blood. IgA is an antibody that plays a crucial role in the immune function of mucous membranes.
- Stool examination for parasites: This test is used to detect the presence of parasites in the gastrointestinal tract that could be causing malabsorption.
- Lactose breath test: This test is used to diagnose lactose intolerance, a common cause of malabsorption.
- Gastroduodenal biopsies: If all the above tests were negative, gastroduodenal biopsies were taken and subjected to histopathology to look for any abnormalities in the tissue that could explain the malabsorption.
- If all of the above investigations turned out negative, the patient was labeled as having no detectable cause of malabsorption.
- In the study by Subramaniam et al, if the calculated levothyroxine absorption was ≤60%, indicating potential malabsorption, the following tests were performed:
-
Q. If a patient is detected with H. pylori infection and that is thought to be the cause of malabsorption, does the treatment of H. pylori infection solve the problem of LT4 malabsorption?
- The treatment of H. pylori infection can potentially improve LT4 absorption.
- In the study, two patients with H. pylori infection were treated with antibiotics and subsequently achieved euthyroid TSH levels.
- The production of ammonia by H. pylori bacteria neutralizes the gastric pH, which can interfere with LT4 absorption. Treating the infection can, therefore, help restore normal gastric pH and improve LT4 absorption.
- However, individual responses to treatment can vary, and other factors such as compliance, nutrient deficiencies, and drug interferences should also be considered.
- Some patients may develop pangastritis or gastric atrophy due to H. pylori and continue to have absorption issues even after treatment of the infection.
-
Q. According to the above study, what percentage of patients with refractory hypothyroidism had true malabsorption?
- 63% of the patients in the study had low absorption.
-
Q. According to the above study, what was the absorption of the patient who has true malabsorption versus those having pseudomalabsorption?
- True malabsorption: average absorption was 36%.
- Pseudomalabsorption: average absorption was 77%.
-
Q. How common is celiac disease in patients with autoimmune thyroid disorder?
- Celiac disease is seen in 5-7% of patients with autoimmune thyroid disorder.
-
Q. What percentage of patients with autoimmune thyroid disorder have autoimmune gastritis?
- Approximately 10-40% of patients with autoimmune thyroid disorder have autoimmune gastritis.
-
Q. What is the specific treatment for patients with autoimmune gastritis and refractory hypothyroidism?
- Liquid thyroid preparation is specific for these patients.
- However, it is not yet available in India.
-
Q. What are the various excipients used in levothyroxine preparations?
- Various excipients are used in the formulation of levothyroxine tablets. Some of them include:
- Binders: These are used to hold the tablet together and give it shape. Common binders include microcrystalline cellulose, povidone, and starch.
- Disintegrants: These help the tablet break apart in the digestive tract to release the active ingredient. Examples include croscarmellose sodium and sodium starch glycolate.
- Lubricants: These prevent the tablet from sticking to the machinery during production. Magnesium stearate is a commonly used lubricant.
- Glidants: These improve the flowability of the powder mixture before it is compressed into a tablet. Silicon dioxide is often used for this purpose.
- Fillers or diluents: These are used to bulk up the tablet to a manageable size. Lactose and microcrystalline cellulose are common fillers.
- Coloring agents: These are used to give the tablet a distinctive color for easy identification. Various dyes may be used for this purpose.
- Coating agents: These are used to make the tablet easier to swallow and to protect it from moisture. They can also be used to control where in the digestive tract the active ingredient is released. Common coating agents include hypromellose and polyethylene glycol.
- Please note that the exact composition of excipients can vary between different brands and formulations of levothyroxine.
- Various excipients are used in the formulation of levothyroxine tablets. Some of them include:
-
Q. How do these excipients differ in different preparations?
- Excipients can differ in different preparations of levothyroxine. The specific excipients used and their quantities may vary between different brands and formulations. The excipients chosen depend on various factors such as the manufacturing process, stability requirements, and desired tablet characteristics.
- Different formulations may use different binders, disintegrants, lubricants, glidants, fillers, coloring agents, and coating agents. The specific excipient composition can impact factors such as tablet hardness, disintegration time, dissolution properties, and stability.
- It's important to consult the package insert or product information for a specific levothyroxine preparation to know the exact excipients used in that formulation.
-
Q. What do we know when a tablet is disc-shaped?
- When a tablet is disc-shaped, it indicates that it is a solid dispersion of the active ingredient and disintegrable excipients.
- Disc-shaped tablets are typically produced by compressing or compacting a powder mixture into a solid dose form.
- The excipients in these tablets serve several functions, such as improving powder flowability, promoting cohesion of different substances, facilitating tablet disintegration in the gastrointestinal tract, and preventing the tablet from sticking.
- To facilitate swallowing and enhance stability, the tablet is often coated with a polymer.
- Excipients commonly used in disc-shaped tablets include glidants (e.g., magnesium stearate and talc), binders (e.g., lactose, starch, cellulose, and polyvinylpyrrolidone), disintegrants (e.g., polyvinylpyrrolidone and sodium carboxymethyl cellulose), and lubricants (e.g., talc, silica, and magnesium stearate).
- Granulation of the ingredients is usually necessary before compression to ensure even distribution of the active ingredient and achieve the desired dosage in each tablet.
-
Q. Does poor storage of T4 tablets impact its function?
- Yes, poor storage conditions can significantly impact the function of T4 tablets.
- Exposure to high temperatures can degrade the active ingredient, levothyroxine, reducing its potency and effectiveness.
- High humidity can also affect the stability of T4 tablets. Moisture can cause the tablets to break down and lose their effectiveness.
- Light exposure can also degrade levothyroxine, leading to reduced efficacy of the medication.
- Therefore, T4 tablets should be stored in a cool, dry place, away from direct sunlight, to maintain their efficacy.
- It's also important to keep the medication in its original container with the lid tightly closed to protect it from moisture and light.
- Patients should be advised not to store their medication in places with high heat and humidity, such as bathrooms or kitchens.
-
Q. Does switching from branded to generic preparation impact thyroid function?
- Switching from branded to generic levothyroxine preparations can potentially impact thyroid function.
- Different brands and generic preparations of levothyroxine may have slight variations in bioavailability, which could lead to changes in thyroid hormone levels in the body.
- These changes may be significant enough to necessitate dosage adjustments to maintain therapeutic levels of thyroid hormone.
- The Endocrine Society has expressed concern about switching between brands and from a brand to a generic preparation and generally recommends avoiding such switches to ensure pharmacologic homeostasis in patients.
- If a switch is necessary, it is recommended to monitor thyroid function closely and adjust the dosage as needed to maintain euthyroid status.
- Patient compliance and symptom control may also be affected by a switch from branded to generic preparations, as some patients may perceive a difference in efficacy or experience different side effects.
- Therefore, any decision to switch should be made in consultation with the patient, taking into consideration their clinical status, preferences, and potential cost implications.
-
Q. Which food items impair LT4 absorption?
- Several food items can impair LT4 absorption when taken concurrently or shortly after LT4 administration. These include:
- Soybean: Soy products have been shown to decrease the absorption of LT4, potentially leading to an increase in TSH levels.
- High-fiber foods: Foods high in dietary fiber can also interfere with LT4 absorption.
- Walnuts: These nuts contain substances that can affect the absorption of LT4.
- Certain fruits: Consuming large amounts of certain fruits like papaya, prunes, and grapefruits may affect LT4 absorption.
- Coffee: Drinking coffee or espresso at the same time or shortly after taking LT4 can significantly decrease the absorption of the medication.
- It's important to note that these foods do not need to be completely eliminated from the diet but should not be consumed within a few hours of taking LT4 to ensure optimal absorption.
- Patients should be advised to take LT4 on an empty stomach, ideally an hour before breakfast or at bedtime, several hours after the last meal of the day, to maximize absorption.
- Several food items can impair LT4 absorption when taken concurrently or shortly after LT4 administration. These include:
-
Q. At what time does the peak absorption occur, and within what time does maximum concentration reach?
- The peak absorption of LT4 occurs within approximately 60 minutes after oral administration.
- The maximum concentration of LT4 in the bloodstream is typically reached within 2 hours.
-
Q. Should the gap between tablet and meal be 30 minutes or 60 minutes?
- The recommended gap between taking the LT4 tablet and having a meal is generally 60 minutes.
-
Q. Is lean body mass a better way of calculating LT4 dose compared to actual weight?
- The use of lean body mass as a basis for calculating LT4 dose is an area of debate.
- According to a study by Santini et al., total body weight is commonly used to determine the dosage of LT4 for patients with thyroid diseases.
- The study aimed to assess the impact of body composition on LT4 requirements.
- It found that the average daily LT4 dose was lower in normal-weight individuals compared to overweight and obese subjects.
- There was a stronger correlation between LT4 dosage and lean body mass compared to fat mass.
- Regional tissue composition analysis revealed that peripheral lean mass had the highest correlation with LT4 dosage.
- No correlation was found between peripheral fat mass and LT4 dosage.
- Individual LT4 requirements depend on lean body mass, with age and gender influencing the proportion of lean mass in relation to total body weight.
- Estimating lean mass could help establish a stable LT4 dose more quickly, especially in individuals with a high body mass index due to increased muscular mass or obesity.
-
Q. Does the use of PPI impact LT4 absorption?
- Yes, the use of Proton Pump Inhibitors (PPIs) can impact LT4 absorption.
- PPIs such as omeprazole and lansoprazole have been shown to increase serum Thyroid Stimulating Hormone (TSH) levels when used concomitantly with LT4 in patients with goitrous or serum TSH > 5 mU/L.
- The effect of PPIs on LT4 absorption is believed to be related to changes in gastric pH, as variations in gastric juice pH, such as during PPI treatment, may affect LT4 absorption.
- Therefore, it is important to consider the potential impact of PPIs on LT4 absorption when prescribing these medications together.
-
Q. How does the ingestion of calcium carbonate impact LT4 absorption?
- Calcium carbonate ingestion can significantly impact the absorption of Levothyroxine (LT4).
- Calcium carbonate has been shown to adsorb LT4 in vitro and decrease its bioavailability in healthy volunteers.
- In patients replaced with LT4, calcium carbonate therapy can increase serum Thyroid Stimulating Hormone (TSH), sometimes above the normal range.
- Other phosphate binders like sevelamer and lanthanum carbonate, used in chronic renal failure, have also been shown to reduce LT4 bioavailability in healthy subjects and necessitate dose adjustments in patients on LT4 therapy.
- Therefore, it is important to consider the potential impact of calcium carbonate and other phosphate binders on LT4 absorption when prescribing these medications together.
-
Q. How does the intake of papaya impact LT4 absorption?
- The intake of papaya can potentially impair the absorption of Thyroxine (T4).
- A case report described the impairment of T4 homeostasis in a thyroidectomized patient after consuming large amounts of papaya fruit for two weeks.
- The authors hypothesized that a component of the fruit might affect intestinal motility or deconjugating bacterial enzymes, leading to increased fecal T4 loss.
- Papaya fruit contains proteolytic enzymes, including papain, which can decrease histamine-induced acid secretion. Fibers in papaya may also bind T4 in the intestine.
- Therefore, it is important to consider the potential impact of papaya intake on T4 absorption, especially in patients on levothyroxine therapy.
-
Q. How does the impact of milk impact LT4 absorption?
- Milk ingestion can significantly impact the absorption of Levothyroxine (LT4).
- Studies have shown that simultaneous milk ingestion can decrease oral LT4 absorption and alter its pharmacokinetic parameters.
- Naive cow's milk, with a pH around 6.6/6.7, and containing calcium, fat, proteins, and lactose, may interfere with LT4 absorption and maintain it in the intestinal lumen.
- Therefore, it is generally recommended that patients on LT4 therapy should avoid consuming milk at the same time as taking their medication to ensure optimal absorption.
-
Q. What is the impact of coffee on LT4 absorption?
- Coffee consumption can significantly impact the absorption of Levothyroxine (LT4).
- Studies have shown that simultaneous ingestion of coffee can alter the pharmacokinetics of LT4, delaying the time of maximal incremental rise of serum T4.
- In vitro studies have confirmed that coffee can bind to LT4 and reduce its absorption.
- Therefore, it is generally recommended that patients taking LT4 should avoid consuming coffee or other caffeinated beverages around the time of their medication to ensure optimal absorption.
-
Q. What about soy?
- Soy products can interfere with the absorption of Levothyroxine (LT4).
- Soy contains isoflavones, which are phytoestrogens that can inhibit the activity of thyroid peroxidase, an enzyme involved in the synthesis of thyroid hormones.
- Additionally, soy protein can bind to LT4 in the gastrointestinal tract, reducing its bioavailability.
- Studies have shown that patients consuming soy supplements may require higher doses of LT4 to achieve the same therapeutic effect.
- Therefore, it is generally recommended that patients on LT4 therapy should avoid consuming soy products around the time of their medication to ensure optimal absorption.
- However, the clinical significance of this interaction can vary among individuals, and further studies are needed to fully understand the impact of soy on LT4 absorption.
-
Q. Use of which substance can increase LT4 absorption?
- Intake of LT4 with Vitamin C can increase its absorption.
- Vitamin C can reduce gastric pH, potentially enhancing the absorption of LT4.
-
Q. Summarize the various drugs, nutrients, and dietary substances that can impact T4 absorption.
-
Q. Does gastroparesis impact LT4 absorption?
- Yes, gastroparesis can significantly impact the absorption of Levothyroxine (LT4).
- Gastroparesis, a condition characterized by delayed gastric emptying, can lead to malabsorption of LT4 due to the prolonged gastric residence time.
- The residual food in the patient's stomach, which may adsorb the ingested LT4, might represent a further mechanism of malabsorption.
- A study confirmed the link between T4 malabsorption and gastroparesis by observing a faint response of Free T4 during a T4 absorption test in a patient with gastroparesis.
- In this case, the weekly intramuscular injection of T4 led to the improvement of the thyroid hormonal profile.
- Therefore, in patients with gastroparesis, alternative routes of LT4 administration may need to be considered to ensure adequate thyroid hormone levels.
-
Q. How does systemic sclerosis contribute to poor LT4 absorption in a patient with concomitant hypothyroidism?
- Systemic sclerosis (SSc) can significantly impact the absorption of Levothyroxine (LT4) in patients with concomitant hypothyroidism.
- SSc is a connective tissue disease characterized by fibrosis and vascular abnormalities in the skin, joints, and internal organs, including the gastrointestinal tract.
- Gastrointestinal involvement in SSc is common and can affect any part of the digestive tract, leading to various complications such as dysphagia, gastroesophageal reflux disease, gastroparesis, small bowel bacterial overgrowth, and malabsorption.
- The fibrotic changes and motility disorders associated with SSc can impair the absorption of LT4, leading to inadequate thyroid hormone levels despite appropriate dosing.
- In addition, SSc can cause changes in the gut microbiota, which may further impact LT4 absorption.
- Therefore, in patients with SSc and concomitant hypothyroidism, careful monitoring of thyroid hormone levels and potential adjustments in LT4 dosage may be necessary. Alternative routes of LT4 administration may also need to be considered in severe cases.
-
Q. In which situations are LT4 softgel capsules and liquid preparations useful?
- LT4 softgel capsules and liquid preparations are useful in the following situations:
- Gastric-related T4 malabsorption: Softgel T4 preparation has been shown to significantly reduce the effective dose required in about two-thirds of patients with gastric-related T4 malabsorption.
- Interference from coffee or proton pump inhibitors (PPIs): Softgel T4 preparation helps overcome the problem of coffee and/or PPI interference on tablet T4 treatment.
- Pediatric use: The liquid T4 solution is advantageous for administration in pediatric patients who may have difficulty swallowing tablets or capsules.
- Patients unable to swallow tablets or capsules: The liquid T4 solution is also beneficial for patients who are not able to swallow tablets or capsules, such as the elderly or those with dysphagia.
- Congenital hypothyroidism in newborns and infants: In these patients, the daily T4 dosage
is calculated according to age, and T4 tablets are usually crushed and given with liquids. In these very young patients, liquid T4 formulation is easily managed and administered and may also be better absorbed than the tablet formulation.
- Patients with gastroparesis: In these patients, alternative routes of LT4 administration, such as softgel capsules or liquid preparations, may need to be considered to ensure adequate thyroid hormone levels.
-
Q. Does sleeve gastrectomy increase or reduce LT4 dose?
- This is an area of debate with bilateral forces at play:
- Situations increasing the LT4 requirement:
- Reduction in acid-producing cells - leading to an increase in gastric pH
- Change in gut microbes
- Situations reducing LT4 requirement:
- Reduction in lead body mass
- Acceleration of gastric emptying
- Situations increasing the LT4 requirement:
- This is an area of debate with bilateral forces at play:
-
Q. What is the impact of RYGB bariatric surgery on LT4 absorption?
- RYGB bariatric surgery can significantly affect the absorption of Levothyroxine (LT4) in morbidly obese patients.
- Studies have shown improved LT4 pharmacokinetics after bariatric surgery, indicating better absorption of the medication post-surgery.
- However, the changes in lean body mass following bariatric surgery could potentially contribute to a change in LT4 doses.
- Some studies have demonstrated a decrease or no change in total LT4 dose but an increase in weight-based LT4 requirement in patients after bariatric surgery.
- The exact mechanisms behind these changes are not fully understood, but suggestions include accelerated gastric emptying, modified gastrointestinal motility, alterations in bile acid or gut microbiome composition.
- It's important to note that only weight-based evaluation may lead to reliable results regarding LT4 absorption post-surgery.
- Further controlled studies are needed before drawing definitive conclusions.
-
Q. Is celiac disease more common in patients with autoimmune hypothyroidism compared to the general population?
- Yes, celiac disease (CD) is more common in patients with autoimmune hypothyroidism compared to the general population.
- The prevalence of CD in the general population is estimated to be around 1%, but this rises to 2% to 5% in patients who also have a thyroid autoimmune pathology.
- Thyroid autoimmune disease is the most frequent autoimmune disorder, and a higher rate of Hashimoto's thyroiditis, the main cause of hypothyroidism, may be detected in patients with CD than in the general population.
- The joint presence of these two diseases is one of the more frequent associations included in polyendocrine autoimmune syndrome type 3B.
-
Q. What is the difference between lactose intolerance and lactose maldigestion?
- Lactose maldigestion and lactose intolerance are two different conditions related to the body's ability to digest lactose, a sugar found in milk and dairy products.
- Lactose maldigestion is a physiological condition where there is a decline in lactase activity, the enzyme responsible for the hydrolysis of lactose into glucose and galactose. This condition is mostly symptomless and affects approximately 70% of adult humans.
- Lactose intolerance, on the other hand, is a clinical syndrome with a pleiotropic clinical picture. It presents with symptoms such as diarrhea, bloating, flatulence, and abdominal pain. The intensity of these symptoms is related to the amount of lactose ingested, intestinal microbial composition, gastrointestinal motor activity, and the visceral sensitivity to fermentation products of lactose digestion.
-
Q. Can lactose intolerance be related to LT4 malabsorption?
- Yes, lactose intolerance can be related to Levothyroxine (LT4) malabsorption.
- Lactose intolerance can lead to an increased need for LT4. This is because when lactose is not properly hydrolyzed due to lactase deficiency, it accumulates in the intestinal lumen and attracts water, which can interfere with the absorption of LT4.
- In a case described by Muñoz-Torres, a patient with lactose intolerance showed an increased need for LT4, which was resolved by switching to a lactose-free LT4 formulation and starting a lactose-free diet.
- A systematic study later confirmed the increased need for LT4 in a larger group of patients with lactose intolerance, as compared with a control group without signs or symptoms of malabsorption.
- Therefore, lactose intolerance can indeed affect the absorption of LT4, leading to a need for higher doses or alternative formulations of the medication.
-
Q. Can lactose be an excipient in LT4 preparations?
- Yes, lactose can indeed be used as an excipient in Levothyroxine (LT4) preparations.
- Lactose is often used as a filler or binder in many pharmaceutical tablets, including some formulations of LT4.
- The amount of lactose used in these preparations is not often disclosed in the leaflets accompanying the medication.
- However, it's important to note that a study provided evidence that the ingestion of up to 400 mg of lactose does not trigger gastrointestinal symptoms or affect the lactose breath test in most individuals.
- For patients with lactose intolerance, the lactose content in these LT4 preparations could potentially represent a problem, leading to malabsorption of the medication. In such cases, lactose-free LT4 formulations may be considered.
-
Q. Ingestion of how much quantity of lactose generates symptoms in patients having lactose intolerance?
- More than 5 grams of lactose triggers symptoms of lactose intolerance.
-
Q. Which parasitic infection is associated with LT4 malabsorption?
- Giardiasis, an infection caused by the parasite Giardia lamblia, has been associated with Levothyroxine (LT4) malabsorption.
- This parasite colonizes the small intestine, which is the primary site of LT4 absorption.
- Giardiasis can cause damage to the intestinal mucosa, leading to malabsorption of nutrients and medications, including LT4.
- In a case reported by Cellini et al., a patient with hypothyroidism and persistent high TSH levels despite high-dose LT4 therapy was found to have Giardiasis. After treatment of the parasitic infection, the patient's TSH levels normalized with a lower dose of LT4.
- Therefore, in patients with unexplained LT4 malabsorption, it may be beneficial to consider and test for possible parasitic infections such as Giardiasis.
-
Q. Can pancreatic insufficiency lead to LT4 malabsorption?
- Yes, pancreatic insufficiency can lead to Levothyroxine (LT4) malabsorption.
- Pancreatic insufficiency, characterized by inadequate production or secretion of pancreatic enzymes, can result in malabsorption of fats and other nutrients, including medications like LT4.
- The pancreatic enzymes play a crucial role in digestion and absorption of nutrients. Their deficiency can disrupt the normal digestive process, leading to malabsorption.
- In a study by Centanni et al., patients with pancreatic insufficiency required higher doses of LT4 to achieve euthyroidism compared to those without pancreatic insufficiency.
- Therefore, in patients with unexplained LT4 malabsorption or those requiring unusually high doses of
LT4, it may be beneficial to consider and test for possible pancreatic insufficiency.
-
Q. What is the role of bile acids in LT4 metabolism?
- Bile acids play a significant role in the metabolism of Levothyroxine (LT4).
- They aid in the solubilization of LT4 in the intestinal lumen, which is a crucial step for its absorption.
- A study by Sinha and Van Middlesworth highlighted the role of bile in reducing the binding of T4 to intraluminal plasma proteins, thereby increasing the absorption of labeled T4 in a washed jejunal loop of rats.
- The authors postulated the presence of substances in the bile that compete for T4 binding with plasma proteins, which could potentially enhance the absorption of T4.
- In the liver, T4 and T3 are conjugated with sulfuric and glucuronic acid, which makes them more soluble, allowing their renal and biliary clearance. The presence of the intestinal microbial flora allows the binding of iodothyronine, thus creating a hormonal reservoir.
- However, conditions that disrupt bile acid synthesis or secretion, such as liver disease or bile duct obstruction, can potentially impair LT4 absorption.
- Furthermore, medications that bind to bile acids, such as cholestyramine and colestipol, can also interfere with LT4 absorption.
-
Q. How does the use of iron impact LT4 absorption?
- Iron salts can interfere with the absorption of Levothyroxine (LT4) when consumed together.
- This is due to the formation of insoluble complexes between iron and LT4, which reduces the bioavailability of LT4.
- Therefore, it is recommended that iron supplements and LT4 should be taken at different times, ideally with a gap of at least four hours between them.
-
Q. How does cholestyramine impact LT4 absorption?
- Cholestyramine, a bile acid sequestrant, can significantly interfere with the absorption of Levothyroxine (LT4).
- This is due to its ability to bind LT4 in the intestine, preventing its absorption into the bloodstream.
- An interval of 5 hours between LT4 and cholestyramine ingestion has been found to be insufficient to restore LT4 absorption.
- Cholestyramine may also act as an inhibitor of hormonal enterohepatic recycling, further impacting LT4 levels.
- Therefore, it is recommended that patients taking both LT4 and cholestyramine should have a longer interval between the two medications, ideally more than 5 hours.
- This interference can lead to elevated TSH levels in patients with hypothyroidism, despite taking supraphysiological doses of LT4.
-
Q. Do fluoroquinolones impact LT4 absorption?
- Fluoroquinolones, a class of antibiotics, can potentially interfere with Levothyroxine (LT4) absorption.
- This is due to the chelation of LT4 by fluoroquinolones, which forms insoluble complexes that are not easily absorbed in the gastrointestinal tract.
- Therefore, it is recommended that LT4 and fluoroquinolones should be taken at different times, ideally with a gap of at least four hours between them.
21-Jul-2023- Update
-
Source: Caron P, Declèves X. The use of Levothyroxine absorption tests in clinical practice. The Journal of Clinical Endocrinology & Metabolism. 2023 Mar 14:dgad132.
-
Q. What is the suggested protocol for Levothyroxine absorption test ?
- 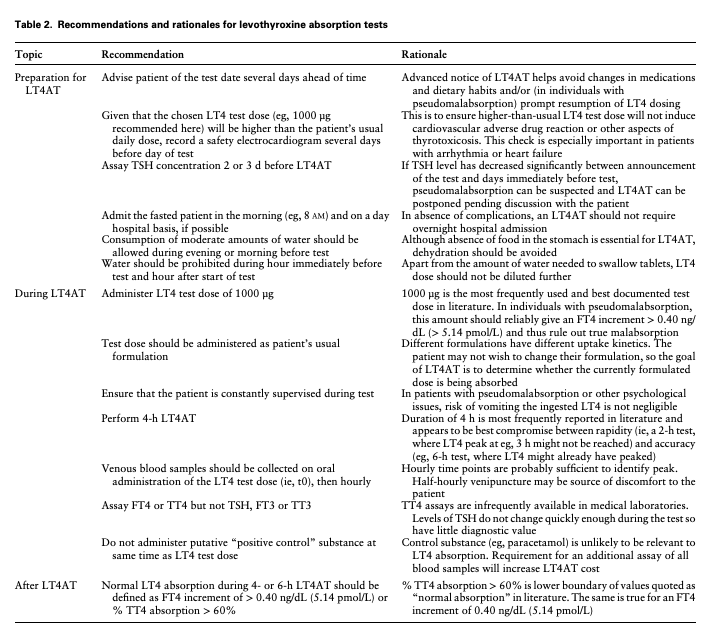
- Q. what was the average dose of LT4 used in various studies ?
- Based on the provided documents, the average dose of Levothyroxine (LT4) used in various studies for the Levothyroxine absorption test (LT4AT) varies. Here are some reported doses:
- The most frequently used and best-documented test dose is 1000 µg.
- Higher test doses have been reported, such as 2000 µg and 2500 µg.
- Some studies used a test dose that was "about twice" the patient's usual LT4 dose, capped at 1000 µg.
- One study standardized the LT4 test dose based on the patient's age and BMI, with doses ranging from 600 µg to 1500 µg.
- It is important to note that the choice of LT4 dose may depend on factors such as the patient's condition, the formulation of LT4 used, and the goals of the LT4AT.
- Q. What percentage of patient were found to truly have malabsorption ?
- Based on the provided documents, the percentage of patients found to truly have malabsorption in the context of Levothyroxine absorption test (LT4AT) varies. Here are some reported percentages:
- In the series described by Gonzales et al, absorption was impaired in only 1 out of the 14 evaluated patients, and this individual had known medical causes of malabsorption.
- Jauk et al diagnosed true malabsorption in a patient where a test dose of 500 µg resulted in a FT4 increment of just 0.1 ng/dL or so.
- The exact percentage of patients with true malabsorption is not explicitly stated in the provided documents.
- Overall, the documents suggest that true malabsorption appears to be less frequent than pseudomalabsorption, which is often related to poor adherence or factitious disorders. However, the specific percentage of patients with true malabsorption is not clearly defined in the provided documents.
- Q. What Is the Volume of Distribution for Levothyroxine, and How Are the Results of an Levothyroxine Absorption Test Adjusted for Other Clinical and Physiological Factors?
- According to the provided documents, the volume of distribution (Vd) for Levothyroxine (LT4) varies depending on the clinical and physiological factors. Here are some reported Vd values:
- In a study by Inada et al, the mean Vd for T4 was reported to be 8.7 ± 1.9 L in euthyroid individuals, 11.0 ± 0.7 L in untreated hypothyroid individuals, and 11.8 ± 0.3 L in treated hypothyroid individuals.
- Another study by Nicoloff and colleagues reported a mean distribution space (Vd) for T4 of 11 ± 0.6 L in euthyroid individuals.
- These values indicate the estimated volume of fluid that would be needed to contain the entire dose of Levothyroxine at the same concentration as it is in the blood. It suggests that Levothyroxine is distributed throughout the body beyond just the blood compartment.
- Q. What exactly is volume of distrubtuion ?
- Volume of distribution (Vd) is a pharmacokinetic parameter that helps us understand how a drug is distributed throughout the body. In simple terms, it tells us how much space the drug takes up in the body.
- Imagine you have a glass of water. The volume of the glass is the amount of space it occupies. Similarly, the volume of distribution is like the "glass" for a drug. It represents the theoretical volume of fluid that would be needed to contain the entire dose of the drug at the same concentration as it is in the blood.
- A high volume of distribution means that the drug is distributed widely throughout the body, indicating that it may be present in tissues and organs beyond just the blood. On the other hand, a low volume of distribution suggests that the drug is mainly confined to the blood.
- The volume of distribution is influenced by various factors, including the drug's properties, such as its size and solubility, as well as the body's characteristics, such as body weight, age, and health conditions.
- Understanding the volume of distribution helps healthcare professionals determine the appropriate dosage of a drug and how it will distribute in different body compartments.
- Q. Which drug has low volume of distribution ?
- Heparin is an anticoagulant medication that is commonly used to prevent blood clot formation. It has a low Vd, typically ranging from 0.02 to 0.1 L/kg. This indicates that heparin remains primarily within the blood plasma and has limited distribution into tissues.
- The low Vd of heparin is due to its large molecular size and strong binding to plasma proteins. These characteristics restrict its movement out of the blood and into other body compartments.
- Drugs with low Vd values like heparin are often administered intravenously and have a relatively short duration of action. They are designed to have a localized effect within the blood and are not intended to distribute extensively into tissues or organs.
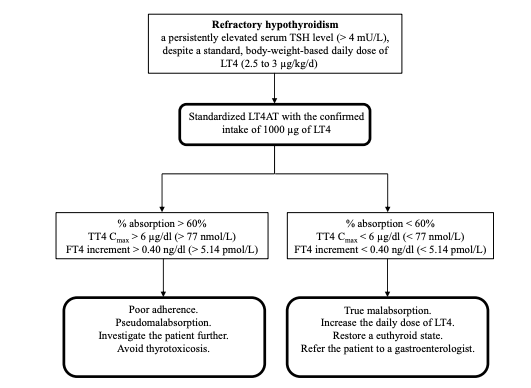
- Q. Give the key flowchart from the study ?
- 
- References:
-
- Kalra, Sanjay; Narayanan, Prem1,; Monteiro, Ana Soraya P.D.R.2. A 6 Dimensional approach to Diagnosing Refractory Hypothyroidism. Thyroid Research and Practice 17(2):p 53-55, May–Aug 2020. | DOI: 10.4103/trp.trp_14_20
-
- Subramaniam K, Babu T, Sreevalsan KC, Mathew S. Levothyroxine Absorption Test - Results and Follow Up of Patients from a Single Center. Indian J Endocrinol Metab. 2023 Jan-Feb;27(1):32-36. doi: 10.4103/ijem.ijem_188_21. Epub 2022 Apr 29. PMID: 37215266; PMCID: PMC10198188.
-
- Ghosh S, Pramanik S, Biswas K, Bhattacharjee K, Sarkar R, Chowdhury S, Mukhopadhyay P. Levothyroxine absorption test to differentiate pseudomalabsorption from true malabsorption. European Thyroid Journal. 2020;9(1):19-24
-
- Virili, C., Antonelli, A., Santaguida, M.G., Benvenga, S. and Centanni, M., 2019. Gastrointestinal malabsorption of thyroxine. Endocrine Reviews, 40(1), pp.118-136.
-
- Santini F, Pinchera A, Marsili A, Ceccarini G, Castagna MG, Valeriano R, Giannetti M, Taddei D, Centoni R, Scartabelli G, Rago T, Mammoli C, Elisei R, Vitti P. Lean body mass is a major determinant of levothyroxine dosage in the treatment of thyroid diseases. J Clin Endocrinol Metab. 2005 Jan;90(1):124-7. doi: 10.1210/jc.2004-1306. Epub 2004 Oct 13. PMID: 15483074.
-