m
Pituitary Apoplexy
Author: Dr. Om J Lakhani
Updated: #jan2025
If you find this useful, please use the link to see the various ways in which you can Support us →
-
Q. What is Pituitary Apoplexy?
- Clinical syndrome caused by acute ischemic infarction or hemorrhage within a pituitary adenoma.
- Typically occurs in the setting of an existing pituitary adenoma.
- Leads to rapid expansion of the adenoma.
- Causes acute onset of symptoms like headache, visual impairment, ocular paresis, altered mental status, and hormonal dysfunction.
- Results from compression of the normal pituitary gland or the hypothalamus.
-
Q. Is it because of infarct or hemorrhage in the pituitary?
- Could be either.
-
Q. Can it be asymptomatic?
- The infarct or hemorrhage can be asymptomatic.
- However, it is not under the umbrella definition of Pituitary Apoplexy.
-
Q. Is Sheehan a form of pituitary apoplexy?
- Since Sheehan is subclinical, it does not fall under the said definition.
- However, it is also a form of pituitary infarction.
-
Q. Is it reported in which most common subtype of Pituitary Adenoma?
- It is most commonly reported in non-functioning pituitary adenomas.
- Among functional tumors, it is most common in prolactinomas.
-
Q. Can it also occur in conditions not associated with Pituitary Adenoma?
- Rarely, it can occur in the absence of a pituitary adenoma in conditions such as Rathke's cleft cysts, pituitary hyperplasia, or inflammatory lesions.
-
Q. What are the outcomes of pituitary apoplexy?
- Deterioration:
- Subarachnoid hemorrhage (SAH) or cerebral vasospasm.
- Improvement:
- With sequelae: Pituitary insufficiency, neurological disorder, or visual deficit.
- Without sequelae.
- Deterioration:
-
Q. What are the precipitating factors?
- Angiographic procedures.
- Anticoagulants.
- Increase in blood pressure.
- Dopamine agonists.
- Pituitary dynamic testing.
- High dose of estrogens.
- Trauma.
- Bleeding disorders.
- Cardiac surgery.
- Increase in intracranial pressure.
-
Q. What are the pathophysiological reasons for pituitary apoplexy?
- Tumor outgrowing its blood supply.
- Superior hypophyseal artery compressing against the diaphragmatic sellae.
- Inferior hypophyseal artery entrapment against the diaphragmatic notch.
-
Q. Is there a change in the blood supply between a normal pituitary and that of an adenoma?
- Yes.
- Normal pituitary is supplied by the superior hypophyseal artery.
- However, when there is a pituitary tumor, the blood supply comes from the inferior hypophyseal artery.
- The latter blood vessel is more vulnerable to pressure changes.
-
Q. Enlist the clinical features of pituitary apoplexy.
- Headache.
- Visual disorders.
- Loss of consciousness.
- Cranial nerve involvement: 3rd, 4th, 6th, and V1.
- Focal neurological deficit: Due to internal carotid involvement in the cavernous sinus.
- Endocrine dysfunction.
-
Q. What is the typical headache seen in patients with pituitary apoplexy?
- It is frontal and retroorbital in nature.
- It is often severe and described as "thunderclap" or "worst ever" headache.
- This headache is frequently associated with nausea and vomiting.
-
Q. What are the features of 3rd nerve palsy?
- Ptosis.
- Loss of light and accommodation reflex.
- Eyeball is downward and outward.
- Pupil: Mid-dilated.
-
Q. Can it produce facial nerve palsy?
- Yes.
-
Q. What are the points in the pituitary apoplexy score?
- Consciousness:
- Normal – GCS 15: 0.
- Mild – GCS 8-14: 2.
- Severe – GCS <8: 4.
- Visual acuity:
- Normal: 0.
- Unilateral: 1.
- Bilateral: 2.
- Ocular paresis:
- Absent: 0.
- Present – Unilateral: 1.
- Bilateral: 2.
- Visual field defect:
- Absent: 0.
- Unilateral: 1.
- Bilateral: 2.
- Consciousness:
-
Q. What is the use of this score?
- The score is useful for conservatively managed patients.
- A score of ≥4 or an increasing score would suggest the need for surgical intervention.
-
Q. Can DI occur in pituitary apoplexy?
- Yes.
-
Q. In case of suspected apoplexy, what is done first – CT or MRI?
- CT is done first, as MRI cannot diagnose fresh blood early.
- MRI is more useful in the subacute setting (4 days to 1 month).
-
Q. How will blood appear in a CT scan in various time frames?
- Acute (0-10 days): Hyperdense (60-80 HU).
- Subacute (10-20 days): Isodense (40 HU).
- Chronic (>20 days): Hypodense (10 HU).
-
Q. What about MRI?
- In T1:
- Acute (<24 hours): Isointense.
- Subacute (3-5 days): Hyperintense.
- Chronic (>3 weeks): Hypointense.
- In T1:
-
Q. What suggests hemorrhage and necrosis in subacute MRI?
- In T1:
- Hyperintense: Hemorrhage.
- Hypointense: Necrosis.
- In T1:
-
Q. What is the importance of knowing the timing of the origin of symptoms?
- To determine the best imaging approach.
-
Q. Which imaging must be done when the patient presents with symptoms within 6 hours of origin?
- CT scan.
-
Q. What do you see in this picture?
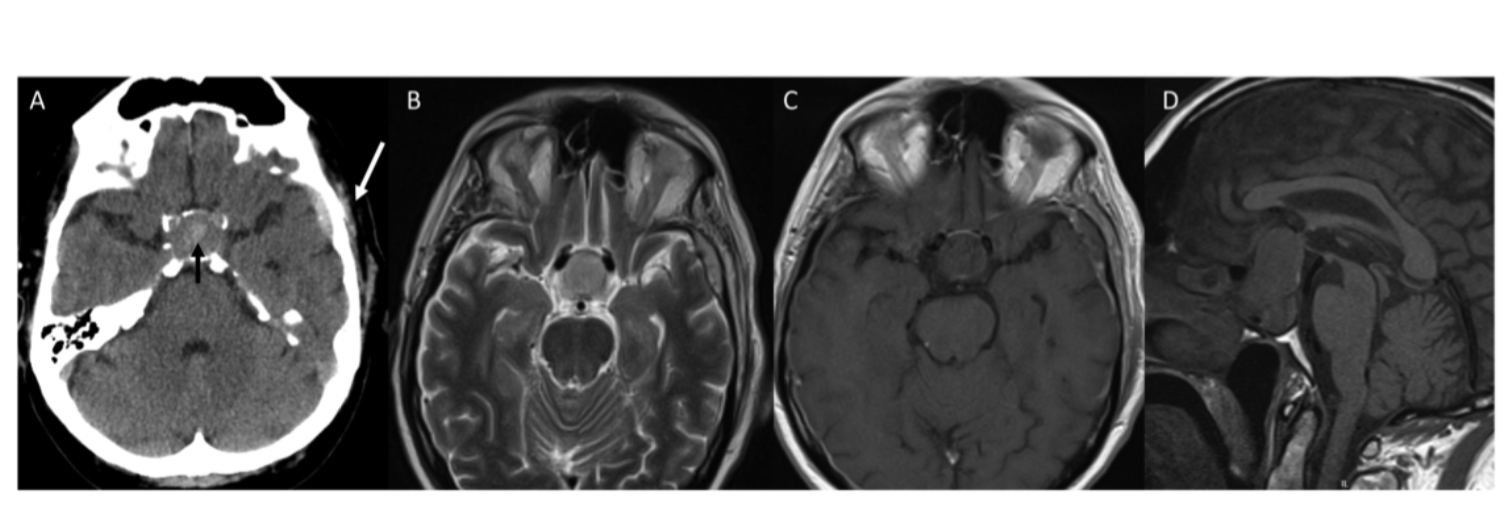
- The CT scan shows a hemorrhage in the pituitary, while the MRI of the same patient done within the same time frame misses the bleed.
-
Q. Enlist the differential diagnosis of pituitary apoplexy.
- Subarachnoid hemorrhage.
- Infectious meningitis.
- Migraine.
- Rathke's cyst hemorrhage.
- Cavernous sinus thrombosis.
Management
-
Q. Give the management guidelines for pituitary apoplexy.
- Step 1.1 – Assessment:
- Note the time of onset of symptoms:
- If <4 days: Go for a CT scan.
- If >4 days: Go for an MRI sella directly.
- Note the following features on clinical examination:
- Consciousness (GCS).
- Visual acuity.
- Visual field.
- Ocular paresis.
- Calculate the Pituitary Symptom Score.
- Note the time of onset of symptoms:
- Step 1.2 – Cortisol Management:
- Collect a sample for cortisol.
- Start empirical corticosteroids if the following conditions are met:
- Loss of consciousness.
- Hemodynamic instability.
- Reduced visual acuity.
- Severe visual field defect.
- Lower cortisol documented previously.
- Patient already on glucocorticoid replacement.
- Hydrocortisone:
- 100 mg IV bolus followed by 50 mg IV every 6 hours OR
- 50 mg in 50 ml of normal saline at 4 ml/hr (4 mg/hr infusion) – continuous.
- If conditions for empirical hydrocortisone are not met:
- Send 8:00 am cortisol the next morning.
- If cortisol <20 µg/dl: Start hydrocortisone.
- Step 2 – Conservative vs. Surgical Management:
- Surgical management is considered in the following conditions:
- Loss of consciousness.
- Severe loss of visual acuity.
- Severe visual field defects.
- Pituitary Symptom Score ≥4.
- Timing of surgery: Must be done within 1 week.
- Surgical management is considered in the following conditions:
- Step 3.1 – Conservative Management:
- Daily visual field and visual acuity monitoring.
- Hemodynamic monitoring and neurological status monitoring.
- Step 3.2 – Surgical Management:
- Transsphenoidal approach – preferred.
- Step 4 – Postoperative Management:
- Continue glucocorticoids postoperatively.
- Post-op day 3: Withhold hydrocortisone dose in the afternoon and evening, and check cortisol the next morning at 8:00 am.
- If cortisol >20 µg/dl: Discontinue glucocorticoids.
- If cortisol 14-20 µg/dl: Glucocorticoids only during stress.
- If cortisol <14 µg/dl: Glucocorticoids required.
- Thyroid function on day 3: If low, replace thyroid hormone.
- Visual assessment 48 hours after surgery: Bedside reassessment with perimetry at a later date.
- Step 5 – Long-term Postoperative Management:
- 6 weeks post-op: Reassess anterior pituitary function.
- MRI: 3 months after surgery, then annually for 5 years.
- Step 1.1 – Assessment:
-
Q. How common is secondary adrenal insufficiency in patients with pituitary apoplexy?
- It is very common, found in about 70% of cases.
-
Q. What are the signs of secondary adrenal insufficiency?
- Hyponatremia.
- Hypoglycemia.
- Hypotension.
-
Q. When surgery is considered, how are the outcomes of various complications?
- Endocrine abnormalities: Recover in 2 weeks.
- Visual field defect: 8 weeks.
- Cranial nerve abnormality: 2 months.
-
Q. What is the importance of preoperative prolactin levels in predicting recovery of endocrine function?
- Preoperative prolactin levels >8.8 ng/ml predict a higher likelihood of recovery of endocrine function postoperatively.
-
Q. Give the difference in outcome in early surgery versus late surgery.
- Improvement in Visual Deficits:
- Early Surgery: 57% to 95% improvement.
- Late Surgery: No significant difference in visual outcomes.
- Recovery of Cranial Nerve Palsies:
- Early Surgery: 63% to 100% improvement.
- Late Surgery: No significant difference.
- Pituitary Function Recovery:
- Early Surgery: 19% to 57% improvement.
- Late Surgery: No significant difference.
- Recovery of Visual Acuity:
- Early Surgery: Improvement in visual acuity.
- Late Surgery: No clear association with timing.
- Timing of Surgery and Visual Field Deficits:
- Early Surgery: Higher rate of improvement within 7 days.
- Late Surgery: Lower rate of improvement beyond 7 days.
- General Considerations:
- Early Surgery: Considered for substantial visual deficits after addressing electrolyte and hemodynamic abnormalities.
- Late Surgery: Selection bias in treatment decisions; outcomes must be interpreted with caution.
- Improvement in Visual Deficits:
-
Q. Give the summary of data on surgery versus conservative management.
- Surgical Decompression:
- Historically recommended for rapid relief of symptoms.
- Improves visual deficits and cranial nerve palsies.
- Pituitary function recovery varies.
- Conservative Management:
- Similar outcomes in selected cases.
- Involves stabilization, hormonal replacement, and electrolyte correction.
- Comparative Outcomes:
- No definitive superiority of one approach over the other.
- Factors Influencing Decision:
- Severity of symptoms and complications.
- Limitations in Data:
- Further studies needed for better stratification.
- Surgical Decompression:
-
Q. What percentage of patients have complete regression after conservative management?
- Complete regression is seen in 28% of cases, with a mean time of regression of 18 months.
-
Q. What percentage of patients have progression or recurrence?
- 20%.
-
Q. Does the recurrence or progression depend on whether surgery was done or conservative management was done?
- No.
References:
- Revisiting Pituitary Apoplexy: Donegan D, Erickson D. Revisiting pituitary apoplexy. Journal of the Endocrine Society. 2022 Sep 1;6(9):bvac113.
Multiple-Choice Questions
-
Question: What is the most common subtype of pituitary adenoma associated with pituitary apoplexy?
A. Prolactinomas
B. Non-functioning pituitary adenomas
C. Growth hormone-secreting adenomas
D. ACTH-secreting adenomas
Correct Answer: B
Explanation: Pituitary apoplexy is most commonly reported in non-functioning pituitary adenomas. Among functional tumors, prolactinomas are the most common, but non-functioning adenomas are the overall most frequent subtype associated with apoplexy. -
Question: Which imaging modality is preferred when a patient presents with symptoms of pituitary apoplexy within 6 hours of onset?
A. MRI
B. CT scan
C. Ultrasound
D. X-ray
Correct Answer: B
Explanation: A CT scan is preferred for diagnosing pituitary apoplexy within the first 6 hours of symptom onset because MRI cannot reliably detect fresh blood at this early stage. -
Question: What is the typical nature of the headache experienced by patients with pituitary apoplexy?
A. Mild and dull
B. Frontal and retroorbital, often described as "thunderclap" or "worst ever"
C. Occipital and throbbing
D. Band-like pressure around the head
Correct Answer: B
Explanation: The headache in pituitary apoplexy is typically frontal and retroorbital, severe, and often described as "thunderclap" or "worst ever," frequently accompanied by nausea and vomiting.
Real life case
A 22-year-old girl presented to the gastroenterologist with incessant vomiting. On evaluation, she was found to have pituitary apoplexy. The patient was started on glucocorticoids and had significant improvement following the treatment. There was no optic chiasma involvement.
!CleanShot 2025-01-24 at 15.36.46@2x.png
!CleanShot 2025-01-24 at 15.36.02@2x.png
!CleanShot 2025-01-24 at 15.35.30@2x.png
Updates
- 27-January-25: Experience with Pituitary Apoplexy from India