-
- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
- Credits
-
Q. What is the definition of delayed puberty?
- Absent or incomplete development of secondary sexual characteristics by the age when 95% of children of the same sex and culture have initiated sexual maturation
-
Q. What is the definition of delayed puberty in boys?
- Testicular volume <4 ml in boys >14 years of age
-
Q. What is the definition of delayed puberty in girls?
- Absent breast bud by 13 years
- No menarche five years after the development of breast bud
- No menarche by 15 years of age
-
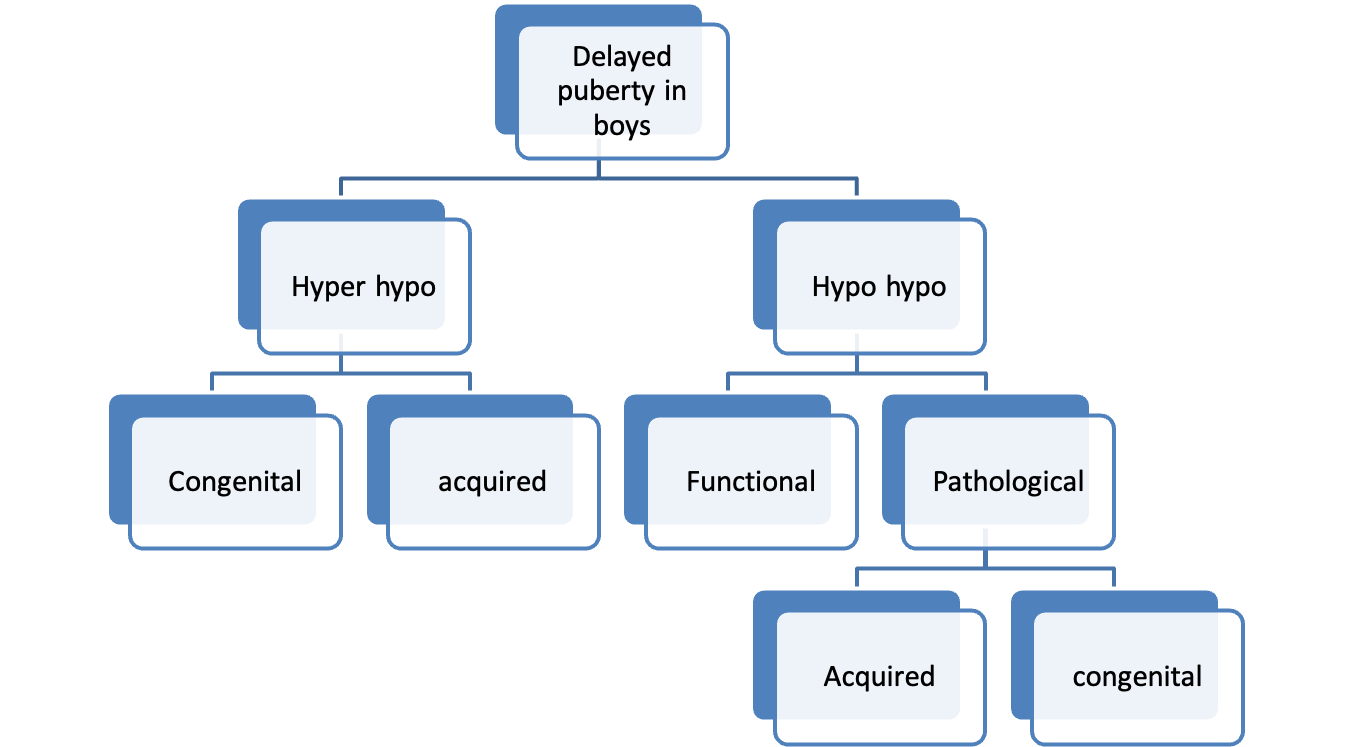
Q. Classify and enlist the causes of delayed puberty in boys?
-
-
Hypergonadotropic hypogonadism
- Congenital
- Klinefelter's
- Gonadal dysgenesis
- Anorchia-
- Vanishing testis syndrome
- Acquired
- Chemotherapy
- Radiation
- Surgery
- Mumps orchitis
- Trauma to testis
- Congenital
-
Hypogonadotropic hypogonadism
-
Congenital
- Isolated GnRH deficiency – IHH
- Without anosmia
- With anosmia- Kallman
- With obesity
- Lawrence Bidel Moon
- Prader Willi
- Part of MPHD (Multiple pituitary hormone deficiencies)
- Isolated GnRH deficiency – IHH
-
Acquired
- Tumors
- Head trauma
- Pituitary apoplexy
- Infiltrative
- Hemochromatosis
- Tuberculosis
- Sarcoidosis
- Granulomatous disease
- Drugs – Marijuana
-
-
Q. What FSH value suggests hyper hypo vs. hypo hypo in boys?
- FSH < 2 – Hypo hypo
- FSH – 2-8 – intermediate
- FSH >8- Hyper hypo
-
Q. What is the most common cause of Hypo hypo in boys?
- CDGP is most common – in 60% of cases
- Functional hypo hypo- 20%
- Hypergonadotropic hypodonadism- 13%
- Idiopathic hypogonadotropic hypogonadism- 12 %
-
Q. What are pointers to Constitutional delay in growth and puberty (CDGP), and what are pointers to a pathological cause?
- Pointers to CDGP
- No pubic hair
- Delayed bone age
- Short stature
- Pointers to a pathological cause
- Presence of pubic hair
- Normal stature
- Normal bone age
- Pointers to CDGP
-
Q. What is the typical pubertal development in Klinefelter syndrome?
- They have stalled puberty (Arrested puberty)
- Pubertal development takes place generally at first
- They have pubic hair development
- At around testicular volume of 8-10 ml- the puberty does not progress further – testis are small and sotty
- They also start having gynecomastia
-
Q. CDGP is more in boys or girls?
- More in boys
-
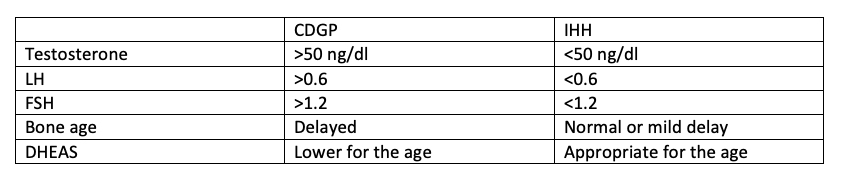
Q. How will you differentiate Constitutional delay of growth and puberty (CDGP) from Idiopathic hypogonadotropic hypogonadism in boys?
- Step 1: History and Examination
- Points towards CDGP
-
- Family history of CDGP
- o Age of menarche of Mother- >15 years is delayed (After 10th grade)
- o Continued growth of father after completing school
- o Growth spurt after 11th grade in father
- o Started shaving after 11th grade
-
- Points towards IHH
-
- Anosmia
-
- Testicular volume 1-2 ml with a bone age of >12 years
-
- Micropenis at birth
-
- Cryptorchidism at birth
-
- Midline defect
-
- Cleft lip / cleft palate
-
- Points towards CDGP
- Step 2: Basic Investigations
- Tests to order
-
- Total Testosterone
-
- LH
-
- FSH
-
- Bone age
-
- Tests to order
- Step 3- Advanced Tests and Stimulation tests
-
- Inhibin B
-
- GnRH Agonist testing
-
- Inhibin B
- • Value < 35 pg/ml- IHH for sure
- • 35-100 pg/ml- Either way-more in favor of CDGP
- • >100 pg/ml- CDGP for Sure
- Inhibin B
-
-
- LUPEROLIDE PROTOCOL (Lakhani protocol developed from Street et al.)
-
- Baseline LH
-
- Inj LUPRIDE 1 mg vial (0.5ml) in Insulin – 100 IU syringe order
- a. 0.25 ml (0.5 mg) – 25 units in Insulin syringe
- b. Inject Subcutaneously
-
- Repeat LH after 2 hr and 4 hr
- Interpretation
-
- Peak LH > 6.1 - Suggestive of CDGP
-
- Peak LH <2.8 IHH
-
- 2.8-6.1- either way – Favour CDGP
-
-
- TRIPTORELIN PROTOCOL
-
- Baseline LH
-
- Inj DECAPEPTYL (Triptorelin) 1 ml subcutaneous (100 ug)- 100 IU in insulin syringe
-
- Check LH and FSH after 2 hrs and 4 hrs
-
- If Peak LH >5 – suggestive of CDGP
- a. Dergos et al. say 14 IU/l is more discriminatory
-
- HCG stimulation test
-
- Baseline testosterone
-
- In HCG (FERTIGYN), 1500 IU IM on alternate days for 3 days
-
- Day 7 – Repeat testosterone
- a. >230 ng/dl – CDGP
-
- ALTERNATE SINGLE DOSE HCG PROTOCOL (DERGOS et al.)
-
- Baseline Testosterone
-
- Inj HCG (FERTIGYN) – 5000 IU im
-
- Repeat testosterone after 72 hrs
- a. Tetosterone >260 ng/dl- CDGP
- b. <86 ng/dl- IHH
- Step 4- Follow Up
-
- Inj TESTOVIRON 50 mg monthly for 3 months
-
- Recheck Testosterone 1 month after the last injection
- a. Testosterone > 300 ng/ml- Suggestive of CDGP
- b. <300 ng/ml- IHH
-
- LUPEROLIDE PROTOCOL (Lakhani protocol developed from Street et al.)
- Step 1: History and Examination
-
#Clinicalpearl Gold standard is GnRH stimulation test
-
Q. Which is more important for assessment in a child with delayed puberty- FSH or LH?
- FSH- more important for a child with delayed puberty
- LH-more important for a child with precocious puberty
-
Q. Give an outline for Constitutional delay of growth and puberty (CDGP) management?
- inj Testosterone (Testoviron)- 100 mg – monthly injection – 3 times
- After the third injection- they generally have a push of puberty
- If no push- then wait for a few months and give a second course
-
Q. What is the importance of bilateral inguinal hernia in boys with delayed puberty?
- It could be testis which is inguinal. Suggests Undescended testis.
-
Q. What is cryptorchidism ?
- It is testis that is not present in the scrotum by 4 months of age. It could be either absent testis or undescended testis.
-
Q. What is anorchia ?
- 46 XY DSD with both testis absent at birth
-
Q. How will you interpret the past history of undescended testis in a child presenting with delayed puberty at 15 years? What are the clinical conditions associated with bilateral cryptorchidism?
-
Genetic disorders are more common in children with bilateral cryptorchidism than those without it
- Hypogonadism and Cryptorchidism
- 46 XY DSD- Ovotesticular syndrome, mixed gonadal dysgenesis – esp if associated with hypospadias
- Defects in testosterone secretion- Kallman, Klinefelter syndrome
- Defects in testosterone action- Androgen insensitivity syndrome
- Bilateral cryptorchidism is more associated with other conditions than unilateral
-
-
Q. What is the most common location for undescended testis?
- Just outside the external ring
-
Q. By what age do undescended testis generally descend?
- Generally, by 6 months of age
- If they don’t descend by that time- unlikely to descend further
-
Q. What pubertal development sign in boys is considered equivalent to menarche?
- Presence of nocturnal sperm emissions or sperm in urine
-
Q. What time before the development of pubic hair does testis tend to develop?
- About 6 months
- Testis development starts about 6 months before pubic hair development
-
Q. How will you ask for a history of Delayed puberty in parents?
- Mother- the onset of menses after 15 years of age
- Father
- Growth spurt after 16 years of age
- Continued to grow in height after graduating from school
- When did they start to shave
-
Q. What age do facial hair develop in children?
- About 2.5 years after growth of testis or about 2 years after growth of pubic hair
- Generally, boys develop facial hair at about 15 years of age
- However, facial hair is not a reliable sign because it depends on ethnicity
-
Q. Should DSD be considered in a case of bilateral cryptorchidism?
- Yes
-
Q. What will you suspect if the patient has tall stature and Hypogonadism?
-
Q. What about obesity and hypogonadism?
- Prader Willi syndrome
- Leptin deficiency
-
Q. What other physical examination findings would you look for?
- Upper segment: Lower segment ratio – would suggest eunuchoid proportion going in favor of Kleinfelter’s
- Whether testis appears atrophic or not
-
Q. What is Tanner Stage 3 pubic hair?
- Hair is dark, coarse, and curly
- Extends to the mid pubis
-
Q. What is DD of Clinodactyly with Hypogonadism?
- Klinefelter syndrome
- 46 XXYY
-
Q. What happens to bone age in Kleinfelter’s?
- Mild delay
-
Q. What are the facial dysmorphisms in 48, XXYY ?
- Asymmetry
- Upslating palpebrel fissures
- Hypertelorism