Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
-
Support you by Becoming a YouTube member (Click here).
- Premium Membership- Download PDF version of Notes, Get ad free video and more
- Consultant Membership- Above plus Download Powerpoint presentation of the notes
-
Support us by purchasing our book - Click here for more details:
-
For more such updates follow our WhatsApp Channel: https://whatsapp.com/channel/0029VaFyQnfHbFUz0LVdBO3h
- Q. What are the current terminology to replace the word NAFLD ?
- It is MASLD - Metabolic dysfunction steatotic liver disease
- or MetALD- for those who consume moderate amounts of alcohol
- Q. Is liver an Endocrine organ ?
- Yes
- Q. Which hormones are produced or modified by the liver ?
- Hormone Production
- Insulin-like Growth Factor- I
- Angiotensinogen
- Thrombopotetin
- Hepcidin
- 25-hydroxyvitamin D
- Hormone Receptors
- Insulin
- Glucagon
- Growth hormone
- T3
- Estrogen
- Androgens
- Cortisol
- Progesterone
- Leptin
- Ghrelin
- Melatonin
- prolactin
- Adiponectin
- Gastrin
- PTHrP
- FGF-21
- Hepatokine Production*
- Fetuin-A
- Fetuin-B
- FGF-21
- Angiopoietin-like proteins
- Selenoprotein P
- Follistatin
- Binding proteins
- Thyroid Binding Globulin
- Sex-Hormone Binding Globulin
- Cortisol Binding Globulin
- IGF-1 binding proteins
- Transthyretin
- Prealbumin
- Albumin
- Lipoproteins
- Metabolic Process
- Glucose Homeostasis
- Lipid Homeostasis
- Hormone Production
- Q. What is the role of hepcidin ?
- Hepcidin controls iron absorption in the intestine.
- High levels reduce iron absorption by binding to and inducing the degradation of ferroportin, the protein that allows iron to enter the bloodstream from the intestinal epithelium and from macrophages.
- it Contributes to the anemia of chronic disease (or anemia of inflammation) by limiting iron availability for erythropoiesis (red blood cell production), due to its upregulation by inflammatory cytokines.
- hepcidin levels are often elevated in patients with Chronic liver disease and hence it contributes to anemia in these patients in the same way
- Q. What is the role of Thrombopoietin ?
- Stimulates Platelet Production: Primary regulator of megakaryocyte and platelet production. TPO encourages the proliferation and differentiation of megakaryocytes, the bone marrow cells responsible for producing platelets
- Q. What is Fetuin-A and what it's relationship with metabolic disorders ?
- Fetuin-A is a protein that acts as an endogenous ligand of TLR4 (Toll-like receptor 4).
- It promotes lipid-induced insulin resistance.
- Fetuin-A has been shown to be involved in the development of non-alcoholic fatty liver disease (NAFLD) and its associated cardiometabolic consequences.
- It is considered as one of the hepatokines, which are proteins secreted by the liver that affect metabolism and insulin sensitivity.
- Q. What about Fetuin-B ?
- Preliminary research indicates that Fetuin-B might also be involved in glucose homeostasis and insulin sensitivity, suggesting a possible link to diabetes, though its role is less clear and direct compared to Fetuin-A.
- Fetuin-B is crucial for female fertility, particularly in protecting against premature zona pellucida hardening in the ovary, thus ensuring normal fertilization.
- Q. What about FGF21 ?
- See the image below

- Q. What is the importance of hormone binding proteins ?
- A lot of hormone binding proteins as listed above are produced by the liver (eg: Thyroxine binding globulin) etc
- Chronic liver disease is associated with reduced levels of these globulins
- Hence the interpretation of these hormones have to be made in the context of the underlying liver disease
- Q. What is Resmetirom ?
- It is an
- Oral
- Liver-directed
- Thyroid hormone receptor beta-selective agonist
- It is an
- Q. If you had to choose one word to define the key driver for the progression of NASH/NAFLD , what is it ?
- lipotoxicity
- Q. Which carbohydrate has a lot of contribution to this pathway ?
- Fructose
- Q. What is still the most common cause of death in patients with NASH/NAFLD ?
- Cardiovascular disease
- Q. Where are the TSH receptors- alpha and beta mainly present ?
- TSH receptor alpha- Heart and Bone
- TSH receptor beta- Liver
- Q. True or false- Subclinical and overt hypothyroidism are associated with higher prevelance of NAFLD ?
- True
- Q. True or false- higher the TSH - more the chances of NAFLD and progression of NAFLD ?
- True
- Q. Considering this fact, would euthyroid patients treated with T4 or T3 would have any benefit in NAFLD ?
- Yes
- This was proven back in 2018 by a study done by Eveline Bruinstroop
- The study investigated the effect of thyroid hormone (TH) treatment on nonalcoholic fatty liver disease (NAFLD) in euthyroid patients with type 2 diabetes mellitus (T2DM) and steatosis.
- Patients were treated with levothyroxine to maintain thyroid-stimulating hormone levels within a specific range, followed by a 16-week maintenance phase.
- The primary outcome measured was the change in intrahepatic lipid content (IHLC), which showed a decrease after treatment.
- Secondary outcomes included small decreases in body mass index (BMI), visceral adipose tissue volume, and subcutaneous adipose tissue volume, but no significant changes in glucose regulation or lipid profile.
- The study concluded that low-dose thyroid hormone therapy was effective and safe for treating NAFLD in men, suggesting that TH or TH analogs could benefit patients with this condition.
- Therefore, considering the findings, euthyroid patients treated with T4 (levothyroxine) or potentially T3 (if studied) might have benefits in managing NAFLD, especially in reducing IHLC and possibly affecting body composition
- Q. What was the TSH level targeted in above study ?
- The target was TSH of 0.34-1.7
- Q. What is stopping us from using the above approach ?
- We do not know the long term cardiac effects of the above which are mediated via TSH alpha
- Q. Explain in simple words how does T3 regulate lipid metabolism in the liver ?
- T3 (triiodothyronine) is a thyroid hormone that plays a crucial role in regulating metabolism, including lipid metabolism in the liver. Here's how it works in simple terms:
- Increases Fatty Acid Oxidation: T3 stimulates the process by which fatty acids are broken down in the liver. This process produces energy.
- Promotes Lipophagy: It encourages the liver cells to clean up and break down lipid droplets, a process known as lipophagy, which helps reduce fatty buildup.
- Enhances Mitochondrial Activity: T3 boosts the activity and creation of mitochondria, the powerhouse of the cell, which plays a key role in energy production and metabolism, including the burning of fats.
- Regulates Gene Expression: It influences the expression of genes involved in lipid metabolism, leading to increased breakdown and reduced storage of fats in the liver.
- Improves LDL Uptake: T3 can also help in reducing bad cholesterol (LDL) levels by promoting its uptake from the blood into the liver, where it's processed and removed from the body.
- T3 (triiodothyronine) is a thyroid hormone that plays a crucial role in regulating metabolism, including lipid metabolism in the liver. Here's how it works in simple terms:
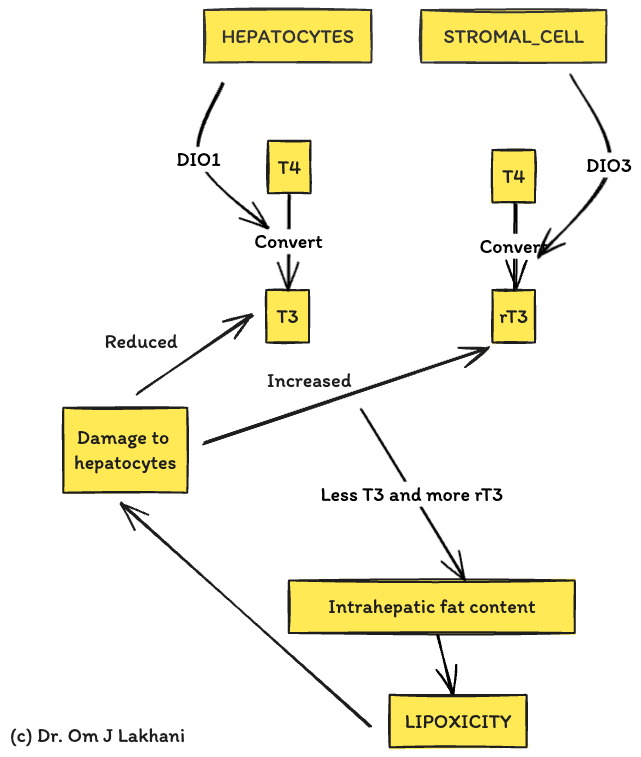
- Q. What is intrahepatic hypothyroidism ?
- Intrahepatic hypothyroidism refers to a condition characterized by reduced activity or levels of thyroid hormones specifically within the liver, despite normal thyroid hormone levels in the bloodstream.
- It is thought to contribute to the development and progression of non-alcoholic steatohepatitis (NASH) and other liver diseases by disrupting normal liver metabolism and increasing lipotoxicity.
- This condition occurs when there's a decrease in the activity of deiodinase type 1 (DIO1), which converts the thyroid prohormone T4 to the active hormone T3 within the liver, and an increase in deiodinase type 3 (DIO3) activity, which converts T4 to inactive reverse T3 (rT3).
- The resulting imbalance leads to a reduction in active thyroid hormone (T3) levels within the liver, contributing to accumulation of lipotoxic species and promoting a cycle of liver injury.
- Intrahepatic hypothyroidism disrupts the liver's ability to regulate lipid metabolism effectively, contributing to the development of fatty liver disease and its progression to more severe forms like NASH.
- The following diagram explains this well
- Q. What is the "Thyroid-liver" axis ?
- The thyroid and liver are connected at multiple levels
- This is called the thyroid-liver axis
- This is how they are connected :
-
- Hepatocytes have type 1 deiodinase which help convert T4 to T3
-
- There are TR-beta receptor beta present in the liver
-
- Thyroxine binding globulin is produced by the liver
-
- Q. What is the pattern of thyroid function in patients with advanced cirrhosis of liver ?
- The pattern is of sick euthyroid syndrome like picture
- Initially low T4- then low TSH and then low T3
- Increased of reverse T3 levels
- The total T3 and total T4 levels may be low because of lower TBG levels
- The pattern is of sick euthyroid syndrome like picture
- Q. What are the thyroid function test patterns in other liver diseases ?
- In acute hepatitits- the TBG may be elevated and hence the Total T3 and Total T4 levels may be high
- In hepatic encephalopathy - there might be central hypothyroidism like picture
- In autoimmune hepatitis - associated Hypothyroidism and Graves' disease are common
- Q. Can overt hypothyroidism mimic a liver disease ?
- Yes
-
- Overt hypothyroidism may be associated with elevated AST and ALT levels which are corrected with giving thyroid hormone replacement
-
- Overt hypothyroidism may be associated with ascites and anasarca
-
- It may be associated with myopathy which may resemble that of liver disease with elevated AST
-
- Overt hypothyroidism can lead to cholestatitc jaundice
-
- The base symptoms of overt hypothyroidism- weight gain, ascities, edema, fatigue, jaundice- may resemble liver disease
-
- Hence it is important to rule out hypothyroidism in all patients with suspected chronic liver disease
- Yes
- Q. What kind of liver dysfunction is seen with hyperthyroidism ?
-
- Hyperthyroidism may be associated with transaminitis
-
- It may be associated with cholestatic jaundice
-
- ATD can lead to liver injury
- Methimazole / Carbimazole may produce cholestatic hepatitits
- PTU can lead to idiosyncratic liver toxicity
-
- Q. Before Resmetirom which other TSH receptor beta agonist were developed and why was the development halted for the same ?
- Sobetirome (GC-1) and eprotirome (KB2115) were the first THR-β agonists shown to reduce intrahepatic lipid content in preclinical models.
- Eprotirome's development was halted in phase III due to cartilage damage observed in dogs after chronic treatment, as well as liver toxicity noted in patients with familial hypercholesterolemia treated for only 6 weeks.
- Sobetirome had favorable effects on lipid profiles by upregulating low-density lipoprotein (LDL) receptors on hepatocytes and reducing hepatic steatosis in a rat model of NAFLD. However, its advancement to phase I was limited by funding issues and some experimental observations of hyperglycemia and insulin resistance.
- Q. Explain this diagram to me which is showing the mechanism of action of Resmetirom
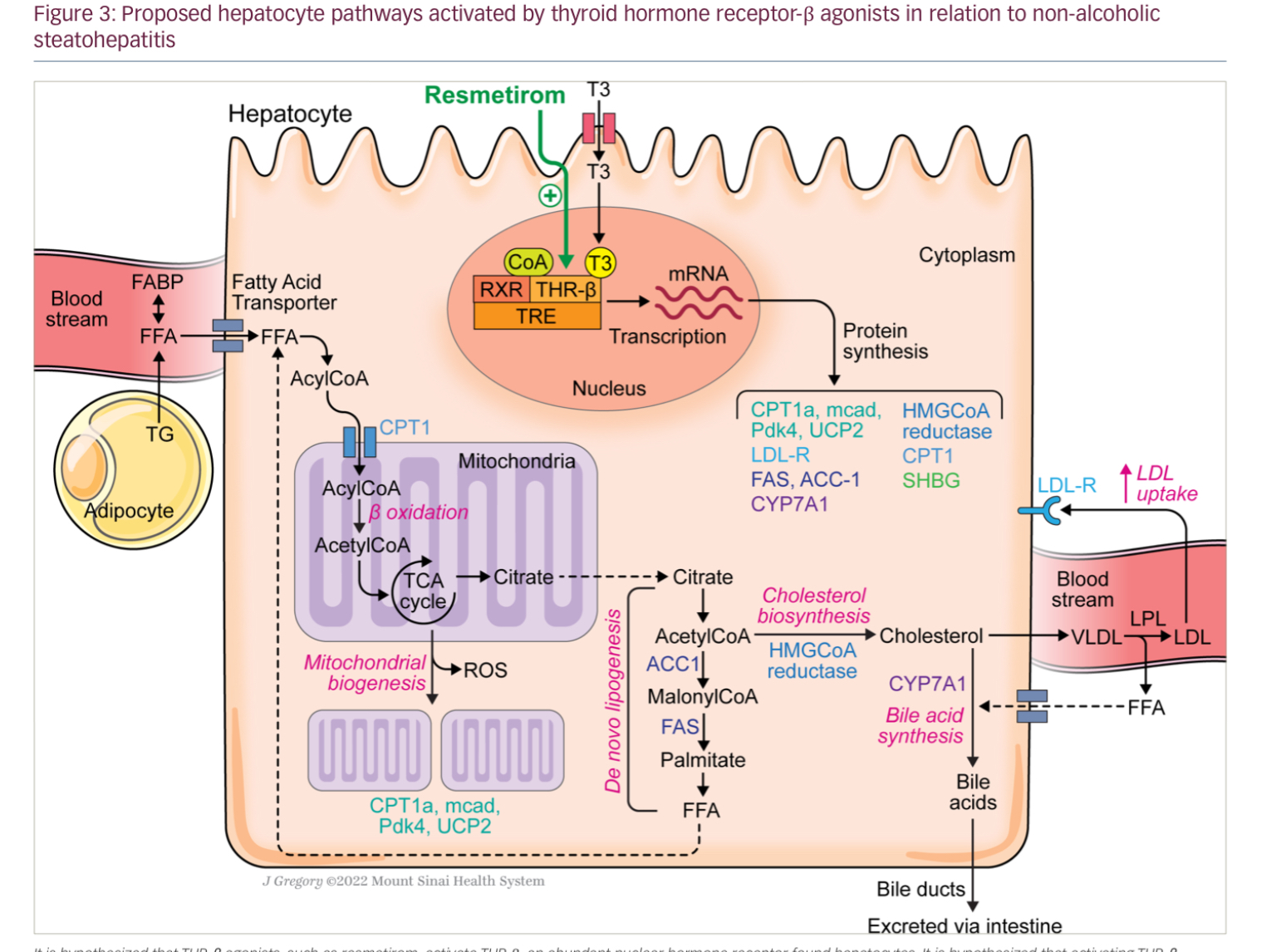
- This diagram outlines the effects of thyroid hormone (T3) and a T3 receptor-β agonist, Resmetirom, on lipid metabolism pathways in liver cells (hepatocytes). Here’s a simplified breakdown:
- T3 and Resmetirom: These substances activate the T3 receptor in the nucleus of liver cells.
- Receptor Activation: When activated, this receptor stimulates the transcription of various genes, leading to the production of proteins that control lipid metabolism.
- Proteins and Their Functions:
- CPT1a, mcad, Pdk4, UCP2: Increase the breakdown of fatty acids in the mitochondria.
- LDL-R: Enhances the removal of LDL ("bad cholesterol") from the bloodstream.
- FAS, ACC-1: Involved in the production of fatty acids.
- CYP7A1: Important for converting cholesterol to bile acids.
- HMGCoA reductase, CPT1, SHBG: Involved in cholesterol synthesis and transport.
- Lipid Metabolism in the Liver:
- Fatty Acids from Blood: Fatty acids are transported from the bloodstream into the liver.
- Beta-oxidation: Fatty acids are broken down in the mitochondria, which may lead to the production of reactive oxygen species (ROS).
- Cholesterol and Bile Acid Synthesis: Cholesterol is produced and converted into bile acids, which help digest fats.
- Triglycerides and VLDL: Triglycerides (type of fat) are formed and released as very-low-density lipoproteins (VLDL), eventually becoming LDL after losing some fat content.
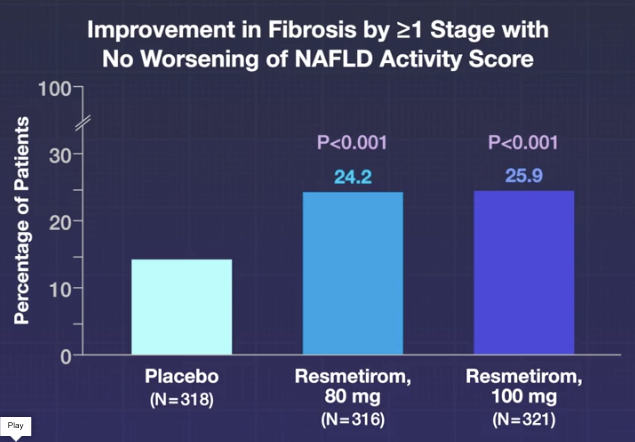
- Q. Is it true that Resmetirom is the first drug approved by the US-FDA for NASH ?
- Yes
- Evidence for Resmetirom in NASH / NAFLD
- Q. What was the name of the phase 3 study published in the NEJM ?
- MAESTRO-NASH trial
- Q. What patients were included in the study ?
- Adult patients with NASH and Fibrosis
- Q. Give the full details of inclusion criteria ?
- Age 18 years or older.
- Presence of at least three of five metabolic risk factors according to a modified version of the International Diabetes Foundation criteria for the metabolic syndrome.
- A controlled attenuation parameter (CAP) of 280 dB per meter or more and a liver-stiffness measurement of 8.5 kPa or more as measured by vibration-controlled transient elastography (VCTE; FibroScan) within the past 3 months, or alternatively, a liver biopsy performed within 6 months before randomization confirmed to be eligible as a baseline biopsy by the central pathologist of the trial.
- Histologic evidence of NASH and a nonalcoholic fatty liver disease (NAFLD) activity score of 4 or more, with a score of 1 or more for each component (steatosis, lobular inflammation, and hepatocellular ballooning).
- At least 50% of the total enrollment was required to have a fibrosis stage of F3, with no more than 15% having a fibrosis stage of F1 (primarily F1B) and no more than 3% having a fibrosis stage of F1A or F1C (only if the N-terminal type III collagen propeptide level was ≥14 ng per milliliter).
- Weight stability (less than 5% change in 3 months) and stable doses of glucagon-like peptide-1 agonists for at least 6 months before biopsy.
- Q. What were the exclusion criteria ?
- Key exclusion criteria included alcohol consumption above specified limits, a glycated hemoglobin level of more than 9.0% at screening, and causes of chronic liver disease other than noncirrhotic NASH
- Q. What Fibrosis stages were included ?
- F1B, F2 and F3
- Q. Enlist the F stages of fibrosis ?
- This is the Metavir scoring system
- F0: No fibrosis
- F1: Portal fibrosis
- F2: Periportal fibrosis
- F3: Bridging fibrosis
- F4: Cirrhosis

- This is the Metavir scoring system
- Q. What is F1B ?
- F1: Portal fibrosis without septa. Within F1, subcategories (such as F1A, F1B, and F1C) can provide more detail about the fibrosis pattern or extent, though these subcategories might not be universally applied or recognized in all scoring systems or studies.
- F1A typically indicates mild fibrosis.
- F1B is often used to denote moderate fibrosis, specifically mentioning fibrosis that is more pronounced in the pericentral (central vein or zone 3) area of the liver lobule.
- F1C might be used in some contexts to describe more specific characteristics or locations of fibrosis within the F1 stage but is less commonly referenced.
- F1: Portal fibrosis without septa. Within F1, subcategories (such as F1A, F1B, and F1C) can provide more detail about the fibrosis pattern or extent, though these subcategories might not be universally applied or recognized in all scoring systems or studies.
- Q. Did all patients undergo liver biopsy ?
- Yes, all eligible patients in the study underwent liver biopsy.
- The study involved adults with biopsy-confirmed nonalcoholic steatohepatitis (NASH) and a fibrosis stage of F1B, F2, or F3.
- The inclusion criteria required histologic evidence of NASH and specific fibrosis stages, which necessitated that participants had liver biopsies to confirm their diagnosis and the extent of their liver fibrosis.
- At the beginning of the study, patients were required to have undergone a liver biopsy within a certain timeframe before randomization, which was used as a baseline biopsy.
- This biopsy confirmed the presence of NASH and the stage of liver fibrosis according to the study's inclusion criteria.
- Additionally, a second liver biopsy was performed at week 52 to assess the primary endpoints, which were NASH resolution (including a reduction in the NAFLD activity score by ≥2 points) with no worsening of fibrosis and an improvement (reduction) in fibrosis by at least one stage with no worsening of the NAFLD activity score
- Q. What does of Resmetirom was given ?
- Two doses- 80 and 100 mg orally
- Q. What were the primary end points ?
-
- NASH resolution with no worsening of fibrosis
-
- Improvement in fibrosis by atleast one grade without worsening of NAFLD activity score
-
- Q. What were the results of the first primary end points ?
- Both doses were effective in significantly reducing the NASH without fibrosis progression

- Q. What about the second primary end point ?
- Also in favour of both doses of Resmetirom
- Q. What were the major side effects ?
- Diarrhea and Nausea
- Q. What were the secondary and other end points ?
- The key secondary endpoint at week 24 was the percent change from baseline in the low-density lipoprotein (LDL) cholesterol level. Other secondary endpoints included changes in various clinical and biochemical parameters indicative of NASH and liver fibrosis improvement, such as:
- Apolipoprotein B level at week 24
- Triglyceride level at week 24 for patients with a baseline triglyceride level of more than 150 mg per deciliter
- Lipoprotein(a) level at week 24 for patients with a baseline lipoprotein(a) level of more than 10 nmol per liter
- MRI-PDFF at week 52
- Alanine aminotransferase level at week 48 for patients with a baseline alanine aminotransferase level of 30 U per liter or more
- Aspartate aminotransferase level at week 48 for patients with a baseline aspartate aminotransferase level of 30 U per liter or more
- γ-Glutamyltransferase level at week 48 for patients with a baseline γ-glutamyltransferase level of 30 U per liter or more
- The key secondary endpoint at week 24 was the percent change from baseline in the low-density lipoprotein (LDL) cholesterol level. Other secondary endpoints included changes in various clinical and biochemical parameters indicative of NASH and liver fibrosis improvement, such as:
- Q. What were the results of the secondary end points ?
- The results for the key secondary and other secondary endpoints in the study were as follows:
- LDL cholesterol levels at week 24 decreased by 13.6% in the 80 mg resmetirom group and by 16.3% in the 100 mg resmetirom group, compared with a 0.1% change in the placebo group. Both reductions were statistically significant compared to placebo (P<0.001 for both comparisons).
- Apolipoprotein B levels at week 24 decreased significantly in both the 80 mg and 100 mg resmetirom groups compared to placebo.
- Triglyceride levels at week 24 showed significant reductions in the resmetirom groups for patients with baseline triglyceride levels of more than 150 mg per deciliter.
- Lipoprotein(a) levels at week 24 also decreased significantly in the resmetirom groups for patients with a baseline lipoprotein(a) level of more than 10 nmol per liter.
- MRI-PDFF at week 52 indicated improvements consistent with the treatment effects of resmetirom.
- Alanine aminotransferase, aspartate aminotransferase, and γ-glutamyltransferase levels at week 48 showed more substantial reductions from baseline in the resmetirom groups than in the placebo group.
- These results suggest that resmetirom treatment not only impacts the primary measures of NASH resolution and fibrosis improvement but also positively affects several metabolic and liver-related biomarkers. The significant reductions in LDL cholesterol, apolipoprotein B, triglycerides, and lipoprotein(a) levels, alongside improvements in liver enzymes, underscore resmetirom's potential to address both liver pathology and cardiovascular risk factors associated with NASH
- The results for the key secondary and other secondary endpoints in the study were as follows:
- Q. What is the impact of Resmetirom on sex hormones ?
- Increase estradiol and total testosterone
- But also increases SHBG so no change in free testosterone
- Other points
- Q. What is the importance of MASLD in pediatric population ?
-
- it is the most common cause of Chronic liver disease in the youth
-
- It is more aggressive
-
- Those youth with MASLD have higher risk of developing CVD early in life
-
- They have more inflammation and fibrosis but no hepatocyte ballooning
-
- Q. Is MASLD associated with hypopituitarism ?
- Yes
- MASLD is associated with hypopituitarism - especially GH deficiency
- Administration of GH is found to be associated with reduction in steatosis
- Q. What is the impact of T3 on Lipid profile as mediated by the liver ?
- T3 reduces the LDL level
- Upgregulates LDL receptors and hence clears LDL from circulation
- T3 reduces triglyceride levels
- By activating lipoprotein lipase
- T3 reduces the LDL level
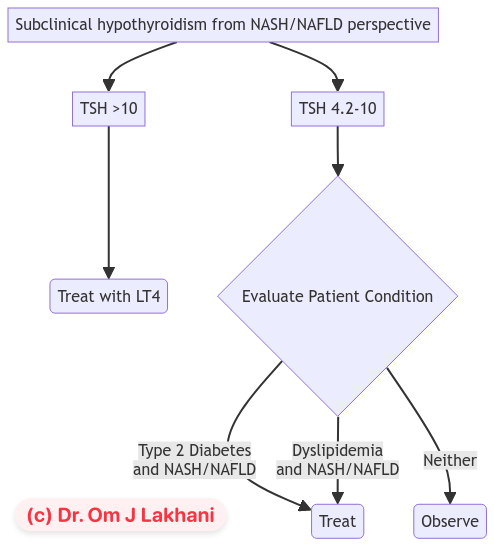
- Q. Is there any study to show the benefits of T4 supplementation in patients with subclinical hypothyroidism with NASH/NAFLD ?
- A study done by Liu et al in about 300 patients showed the following:
-
- T4 supplementation in patients with significant SCH - showed reduction of NAFLD / NASH
-
- T4 supplementation in mild SCH with dyslipidemia showed improvement in NAFLD/NASH
-
- T4 supplementation in mild SCH without dyslipidemia did not show improvement
-
- A study done by Liu et al in about 300 patients showed the following:
- Q. What was the definition of Significant Subclinical hypothyroidism in the study above ?
- TSH >10 was considered significant
- Mild was TSH between 4.2-10
- Q. What was the definition of Dyslipidemia in the study above ?
- Dyslipidemia was defined as abnormalities in the serum levels of lipids, including
- Triglyceride ≥ 150 mg/dl
- Total cholesterol ≥240 mg/dl
- LDL-C ≥ 160 mg/dl
- HDL-C < 40 mg/dl for men and <50 mg/dl for women
- Dyslipidemia was defined as abnormalities in the serum levels of lipids, including
- Q. Is there any study in euthyroid subjects ?
- Yes
- In a small study by Bruinstroop et al measure hepatic fat with MR spectroscopy in euthyroid male patients with NAFLD and and Type 2 diabetes and treated them with low dose of LT4 to achieve a TSH of 0.34-1.7
- After treatment, fat content was decreased 12% (±SEM, 26%) relative to baseline (absolute change, -2%; 95% CI, -3 to 0; P = 0.046)
- Q. What is your personal take on this ?
- The use of LT4 supplementation for patients with NAFLD with subclinical hypothyroidism needs to be explored in more detail.
- NAFLD/NASH itself should eventually be an indication for using LT4 in patients with subclinical hypothyroidism.
- Considering LT4 being cheap and widely available therapy, its potential role in NASH/NAFLD, especially for a resource-limited setting like India, needs to be explored further.
- Q. Based on the above study, please give a flow chart for management of Subclinical hypothyroidism from a NASH/NAFLD perspective
- Q. What is the role of measuring Free T3 to Free T4 ratio in patients with NASH ?
- According to the study done by Turker , the Free T3 to Free T4 ratio is predictive of progression of NASH to cirrhosis and correlates well with FIb-4 score
- This is the conclusion from the study :
- "In this single-center study, we aimed to evaluate the FT3-to-FT4 ratio, which is a new simple marker to assess liver fibrosis in patients with NAFLD. When the APRI, NAFLD fibrosis score, ALBI, AST-to-ALT ratio, FT3-to-FT4 ratio, and FIB-4 were evaluated together, we found that the FT3-to-FT4 ratio was the best predictor for developing NAFLD and NASH cirrhosis"
- Q. What happens to the ratio in the advancement of the disease ?
- The ratio reduces as shown in the table below

- The units used were mIU/L for both
- Q. What is the explanation for this ratio ?
- We know TBG levels decline in advancement of Cirrhosis
- Hence Free T4 levels are a little higher
- Also we saw earlier- that free t3 levels decline with cirrhosis
- Hence the ratio- increase of Free T4 because of less TBG and reducing Free T3 due to the liver disease- make this ratio attractive
- Similar finding is also seen from an Indian study by Punekar et al
References:
- Karim G, Bansal MB. Resmetirom: An Orally Administered, Smallmolecule, Liver-directed, β-selective THR Agonist for the Treatment of Non-alcoholic Fatty Liver Disease and Non-alcoholic Steatohepatitis. touchREV Endocrinol. 2023 May;19(1):60-70. doi: 10.17925/EE.2023.19.1.60. Epub 2023 May 1. PMID: 37313239; PMCID: PMC10258622.
- Bruinstroop E, Dalan R, Cao Y, Bee YM, Chandran K, Cho LW, Soh SB, Teo EK, Toh SA, Leow MKS, Sinha RA, Sadananthan SA, Michael N, Stapleton HM, Leung C, Angus PW, Patel SK, Burrell LM, Lim SC, Sum CF, Velan SS, Yen PM. Low-Dose Levothyroxine Reduces Intrahepatic Lipid Content in Patients With Type 2 Diabetes Mellitus and NAFLD. J Clin Endocrinol Metab. 2018 Jul 1;103(7):2698-2706. doi: 10.1210/jc.2018-00475. PMID: 29718334.
- Harrison SA, Bedossa P, Guy CD, Schattenberg JM, Loomba R, Taub R, Labriola D, Moussa SE, Neff GW, Rinella ME, Anstee QM. A Randomized Controlled Phase 3 Trial of Resmetirom in NASH with Liver Fibrosis. New England Journal of Medicine. 2024.
- Hepatology TL. Resmetirom for NASH: balancing promise and prudence. The lancet. Gastroenterology & hepatology. 2024 Apr;9(4):273.
- Isaacs S, Isaacs A. Endocrinology for the Hepatologist. Current Hepatology Reports. 2024 Jan 18:1-1.
- Sinha RA, Bruinstroop E, Singh BK, Yen PM. Nonalcoholic fatty liver disease and hypercholesterolemia: roles of thyroid hormones, metabolites, and agonists. Thyroid. 2019 Sep 1;29(9):1173-91.
- Liu L, Yu Y, Zhao M, Zheng D, Zhang X, Guan Q, Xu C, Gao L, Zhao J, Zhang H. Benefits of levothyroxine replacement therapy on nonalcoholic fatty liver disease in subclinical hypothyroidism patients. International Journal of Endocrinology. 2017 Apr 4;2017.
- Bruinstroop E, Dalan R, Cao Y, Bee YM, Chandran K, Cho LW, Soh SB, Teo EK, Toh SA, Leow MK, Sinha RA. Low-dose levothyroxine reduces intrahepatic lipid content in patients with type 2 diabetes mellitus and NAFLD. The Journal of Clinical Endocrinology & Metabolism. 2018 Jul;103(7):2698-706.
- Türker F, Oral A, Şahin T, Türker BÇ, Kocak E, Ataoğlu HE, Ahbab S. Does the FT3-to-FT4 ratio easily predict the progression of NAFLD and NASH cirrhosis?. Journal of International Medical Research. 2021 Nov;49(11):03000605211056841.
- Punekar P, Sharma AK, Jain A. A study of thyroid dysfunction in cirrhosis of liver and correlation with severity of liver disease. Indian journal of endocrinology and metabolism. 2018 Sep 1;22(5):645-50.