-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Q. Give a broad outline of the terms NAFLD, NAFL, NASH
-
Q. What is NAFLD?
- (1) Evidence of hepatic steatosis (HS), either by imaging or histology
- (2) lack of secondary causes of hepatic fat accumulation such as significant alcohol consumption, long-term use of a steatogenic medication, or monogenic hereditary disorders.
- (3) no significant alcohol consumption (defined as ongoing or recent alcohol consumption of >21 drinks/week for men and >14 drinks/week for women)
-
Q. What is NASH?
- NAFLD is subdivided into the nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH).
- NAFL, hepatic steatosis is present without evidence of significant inflammation
- NASH, hepatic steatosis is associated with hepatic inflammation that may be histologically indistinguishable from alcoholic steatohepatitis
-
Q. How do you differentiate NASH from NAFL?
- Liver biopsy is the only method to differentiate NAFL from NASH #ClinicalPearl
-
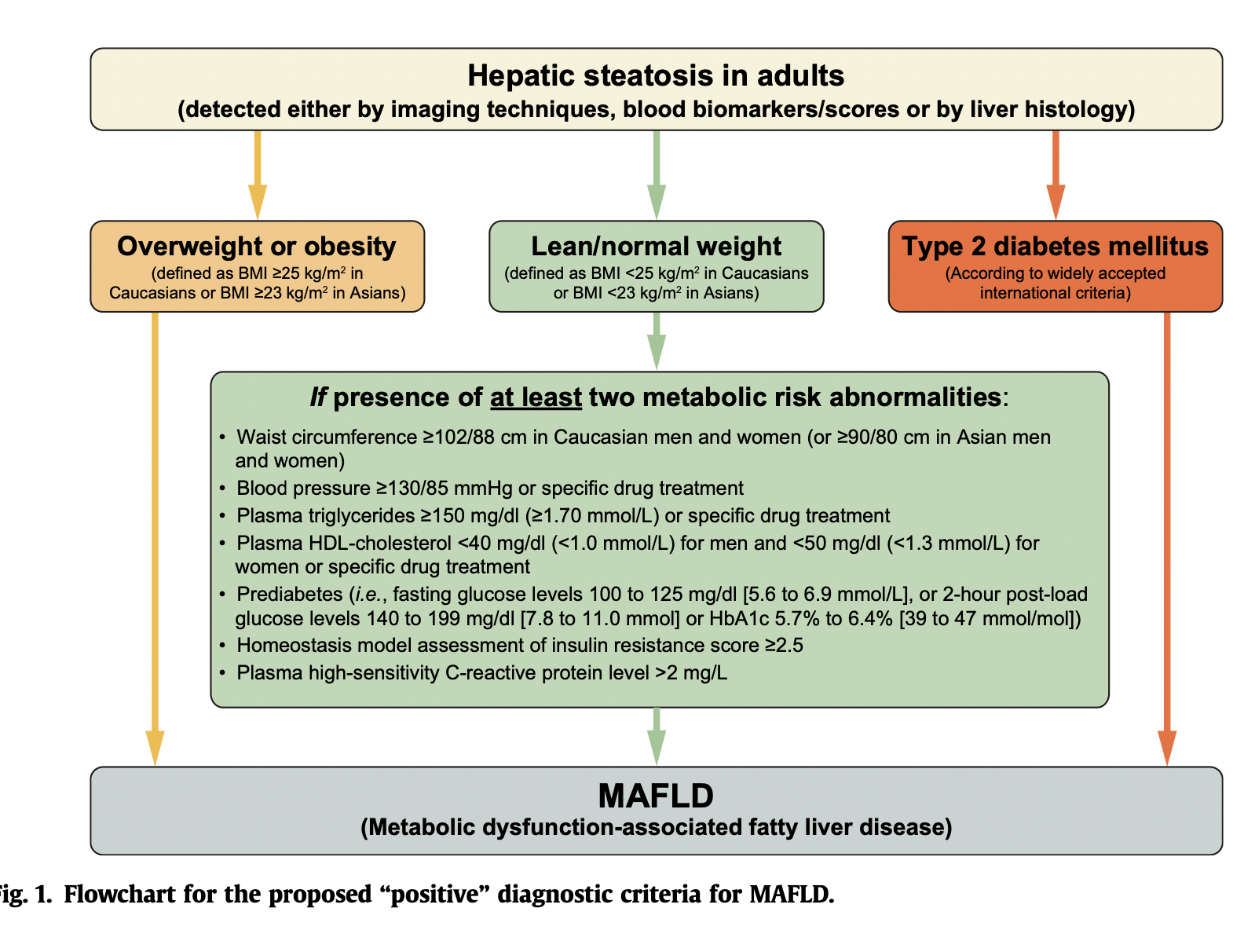
Q. What is MAFLD?
- Metabolic dysfunction-associated fatty liver disease (MAFLD)
- Recently, based on insights gained from the past two decades, an international panel of experts from 22 countries has taken the initiative to propose a new name and definition for NAFLD in adult individuals - that is, metabolic dysfunction-associated fatty liver disease .
- Idea is to make it a diagnosis of inclusion rather than the diagnosis of exclusion
-
Q. Give the direction in which the etiology for transplant is moving.
-
Applying Wilson and Junger criteria for nash/NAFLD screening
-
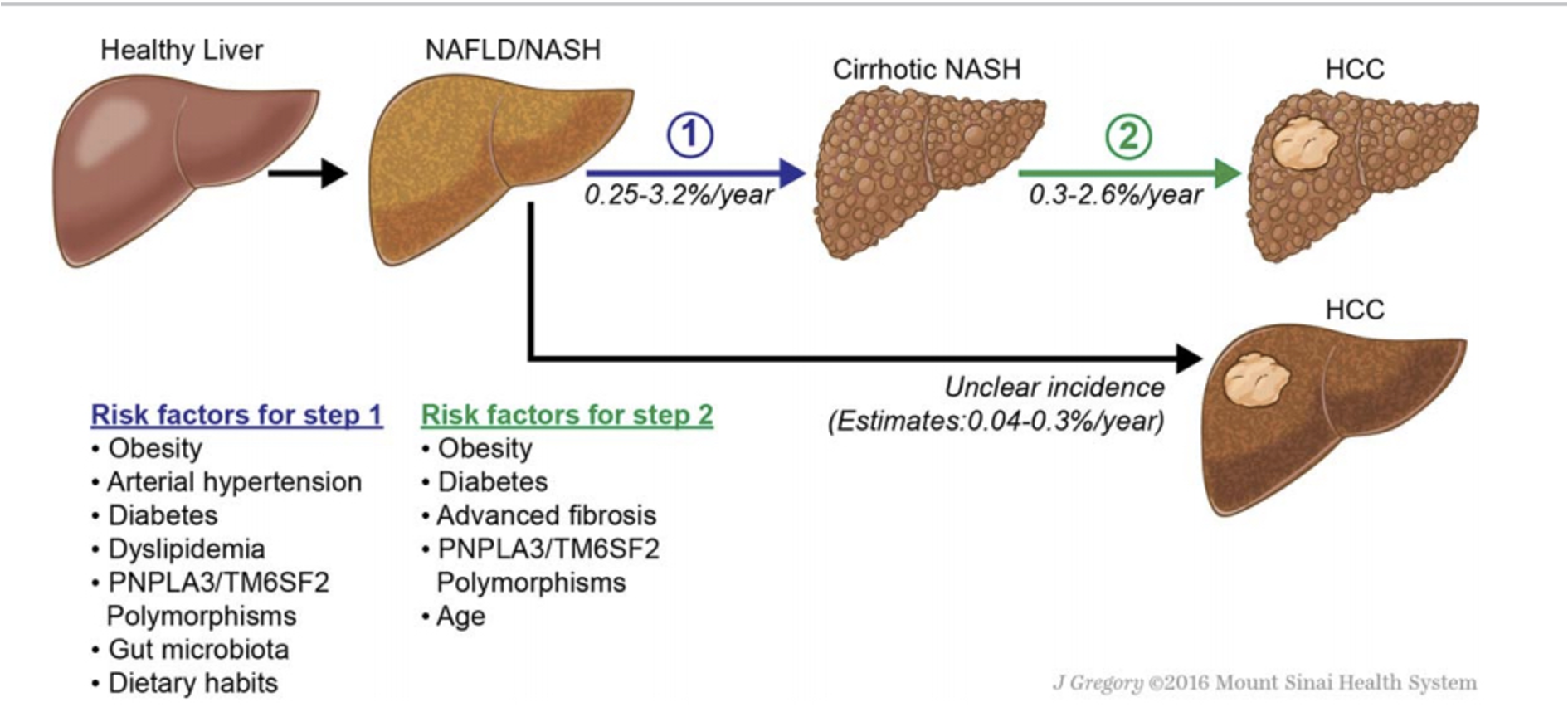
Q. The condition sought should be an important health problem. Is NAFLD an important health problem?
- Yes
- NASH is 2nd most common etiology for Liver transplant and will be number one soon.
- Risk of Liver cancer is increased 2 folds in patients with NAFLD
-
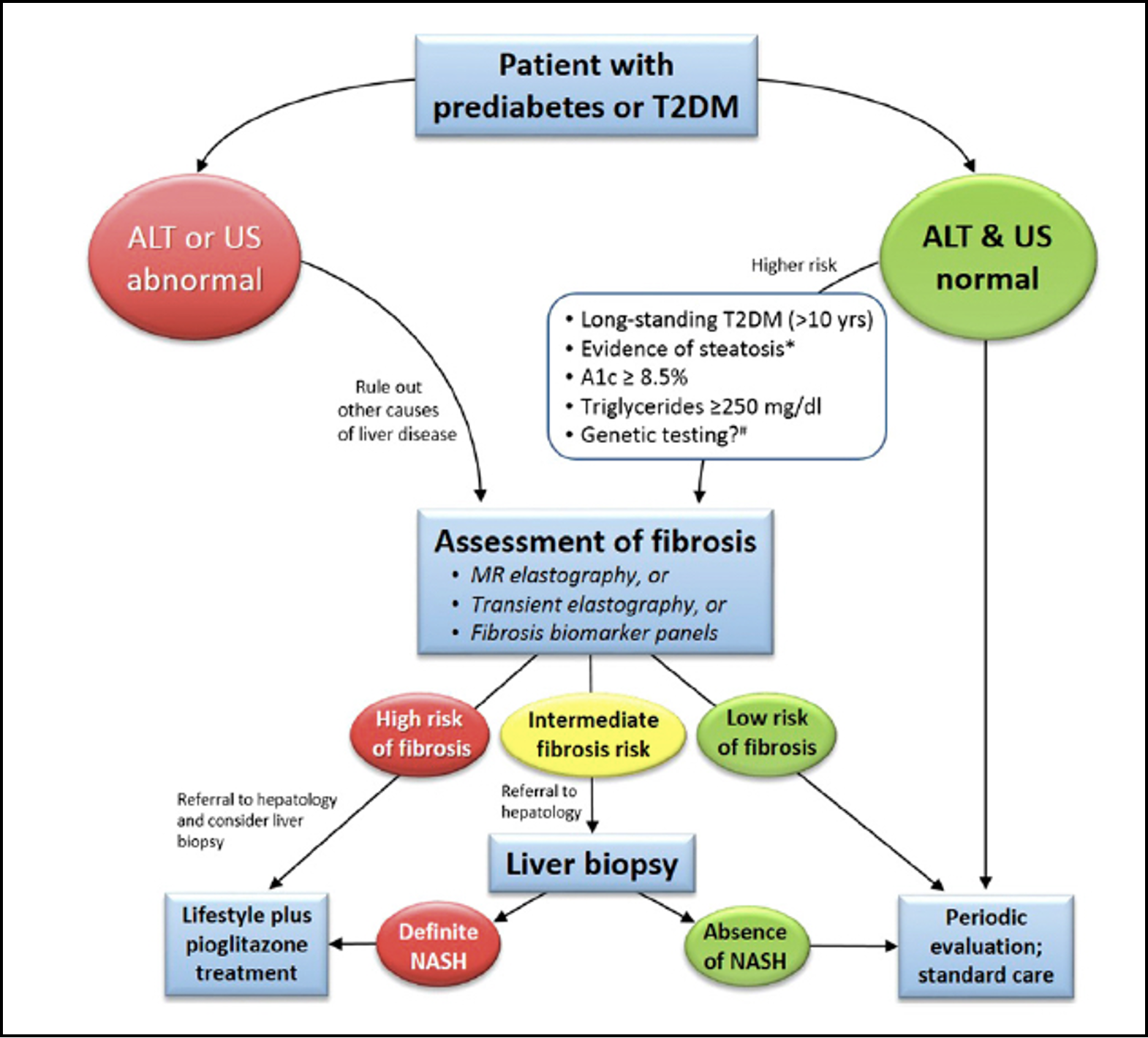
Q. What is the prevalence of NAFLD in patients with type 2 diabetes?
- Depending on the screening methodology used, as much as 65-70% of patients with Type 2 Diabetes have NAFLD
-
Q. There should be an accepted treatment for patients with recognized diseases. Can we prevent the progression of Fibrosis in patients with NASH?
- Yes
- Drugs like Pioglitazone, Empagliflozin, and Liraglutide have been shown to prevent the progression of fibrosis in NASH

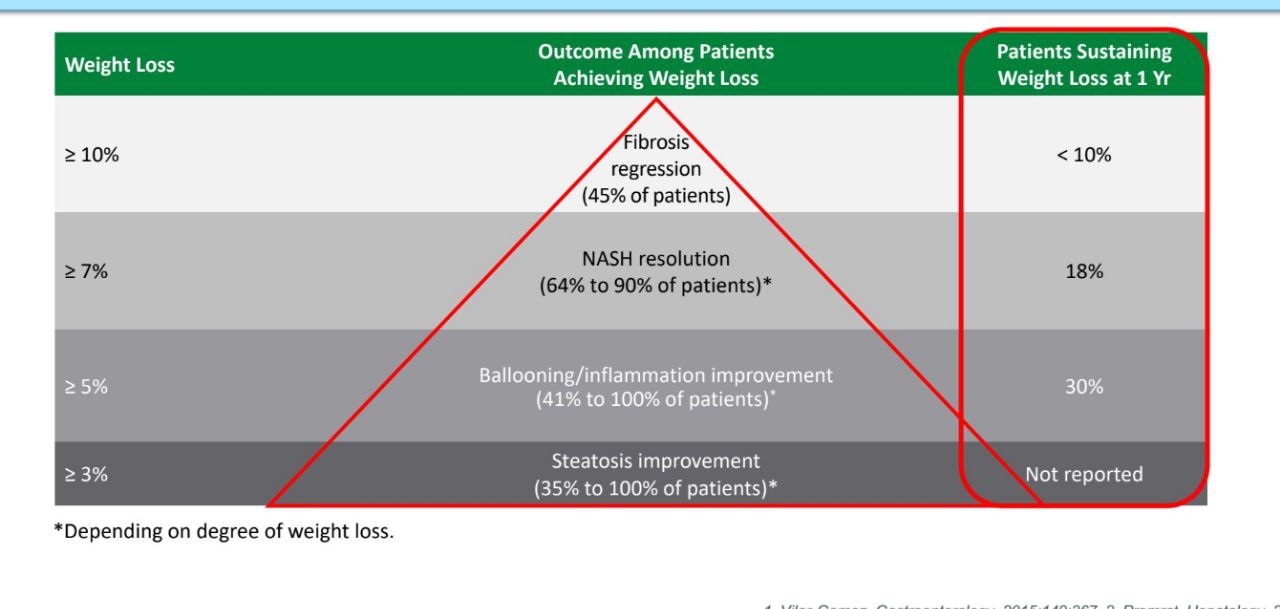
- Weight loss is an effective option for preventing progress in patients with NASH.
-
Q. How do we screen for NAFLD/NASH?
- 2/3rd of patients with NAFLD/NASH have normal liver enzymes
- Typically ALT >AST
- Newer Cut-offs are 30 in males and 19 in females
- USG shows increased echogenicity
- A meta-analysis found that the sensitivity and specificity for ultrasound were 85 and 94 percent, respectively, when using liver biopsy as the gold standard
- The fatty liver index (FLI), is an algorithm based on waist circumference, body mass index (BMI), triglyceride, and gamma-glutamyl-transferase (GGT) used for recognizing fatty liver
- Cutoff of 30 has a sensitivity of 87%
- Cutoff of 60 has a specificity of 86%
- Other tests like Transient elastography, MR spectroscopy, MR elastography, and liver biopsy are more useful for the assessment of fibrosis rather than mere screening
- 2/3rd of patients with NAFLD/NASH have normal liver enzymes
-
Q. Does the AST/ALT (SGOT/SGPT) ratio help in the diagnosis of NASH?
- AST/ALT ratio in NASH/NAFLD is <1 (SGOT/SGPT) while in Alcoholic liver disease, it is more than 2
-
Q. Does the degree of ALT elevation correlate with the severity of the disease?
- the degree of AST/ALT elevation does not correlate with the severity of the disease
-
Q What happens to the ALP levels?
- ALP may be elevated 2-3 times the ULN
-
Q. What is the importance of serum ferritin levels in this disease?
- Serum ferritin has an important role in NASH/NAFLD #ClinicalPearl
- Value >1.5 times the ULN is likely to be associated with greater progression of the liver disease
- Serum ferritin has an important role in NASH/NAFLD #ClinicalPearl
-
Q. What are the diagnostic criteria for MAFLD ?
-
Q. Do we have an early stage here?
- Yes. NASH is an early precursor of Cirrhosis or End stage liver disease which is what we are trying to prevent.
- There should be a suitable test or examination and the test should be acceptable to the population
- Liver enzymes and ultrasound are acceptable tests for the population
-
Q. Upto what stage can the disease be reversed?
- Upto the Fibrosis stage
-
Q. The natural history of the condition, including development from latent to declared disease, should be adequately understood. Do we understand the natural history of NAFLD/NASH?
-
Q. There should be an agreed policy on whom to treat as patients. What to do once NAFLD is recognized?
-
FIBROSIS BIOMARKERS AND SCORES
-
Q. Is screening for NAFLD cost-effective?
- NAFLD is a reversible condition, particularly in the early stages.
- Failing to detect the disease at an early stage can have detrimental clinical effects for some high-risk patients who are in danger of developing liver cirrhosis and related complications such as jaundice, ascites, variceal bleeding, hepatic encephalopathy, and hepatocellular carcinoma.
- NAFLD was considered cost-effective at a cost-effectiveness threshold of £20,000 per QALY gained.
- Fatty liver index is the most cost-effective screening test
-
Q. Give a broad outline of the treatment of NASH/NAFLD.
- Vaccination
- Hepatitis A
- Hepatitis B
- Pneumococcal vaccine
- Weight loss - 0.5-1 kg/week
- Biopsy proven NASH and fibrosis with stage ≥2 and not having diabetes - Vitamin E - 800 IU/day (C. EVION- 400 IU - twice a day)
- Diabetes patients
- Metformin
- Pioglitazone
- Liraglutide
- If after weight loss - repeat ALT/AST after 3 months
- if it has not come to normal - look for other causes
- Vaccination
-
Q. Give some important notes on weight loss and NASH/NAFLD.
- Weight loss to be done to the tune of 0.5- 1 kg/week
- weight loss can reverse all stages except cirrhosis
- Liver function test can be normal in 30% of patients with NASH/NAFLD #ClinicalPearl
-
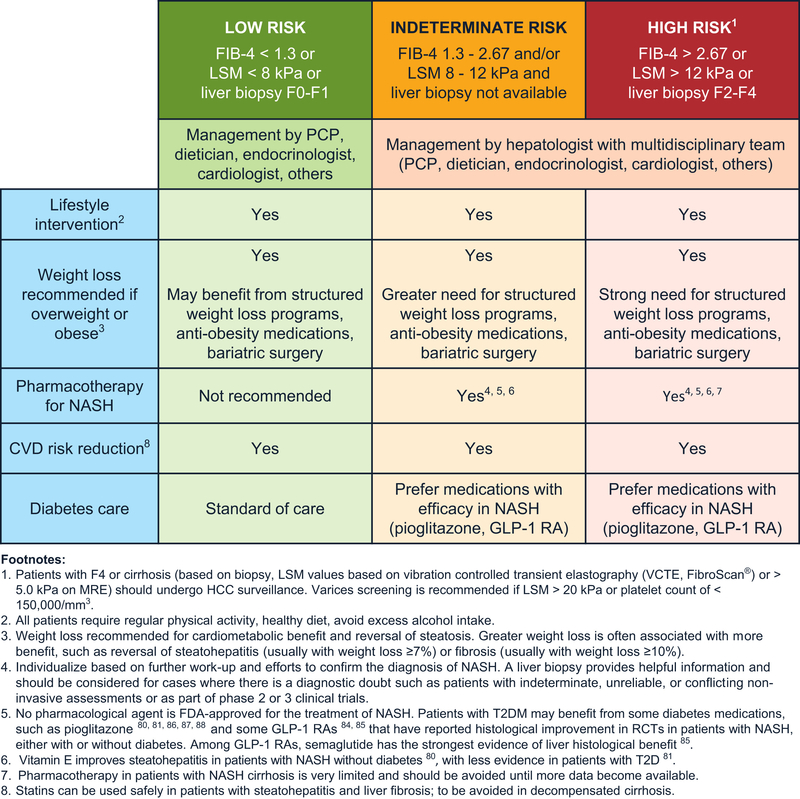
Q. In which cases is Pharmacotherapy used?
- Early stage NASH at high risk for disease progression (age > 50 years, metabolic syndrome, diabetes mellitus, or increased ALT)
- Active NASH with high necroinflammatory activities
- Progressive NASH (bridging fibrosis and cirrhosis)
-
Q. What is the main purpose of any medication used?
- It should be able to prevent the fibrosis stage
- This can be gauged by a reduction of the NAS score (NAFLD Activity score)
-
Q. Give an outline of various legacy drugs and their use in NASH/NAFLD.
-
Q. Is Saroglitazar approved in India for use in NASH/NAFLD?
- Yes
-
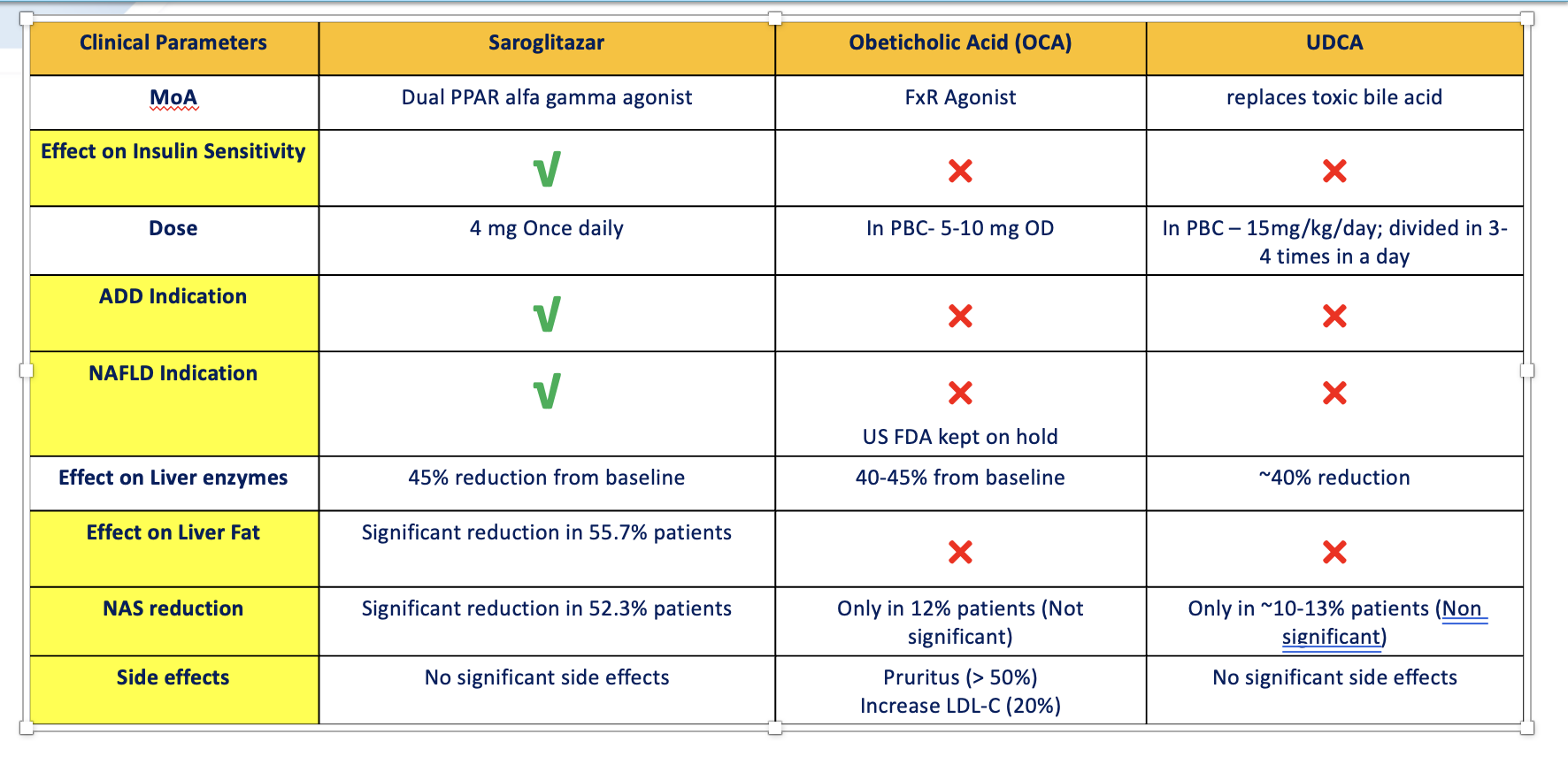
Q. What is the mechanism of action of Saroglitazar?
- Saroglitazar is a dual PPAR α and γ agonist and through activation of these transcriptional factors PPAR α & γ :
- Reduces TG (predominantly through PPAR α agonism)
- Reduces Insulin resistance and controls blood sugar level (predominantly through PPAR γ agonism)
- Saroglitazar is a dual PPAR α and γ agonist and through activation of these transcriptional factors PPAR α & γ :
-
Q. How does Saroglitazar compare with other drugs like OCA and UDCA?
-
Q. Does Saroglitazar reduce (NAFLD Activity score)?
- Yes
-
Q. What is the role of Semaglutide in NASH/NAFLD?
- This is from a trial published in the NEJM
- Nonalcoholic steatohepatitis (NASH) is a common disease that is associated with increased morbidity and mortality, but treatment options are limited. The efficacy and safety of the glucagon-like peptide-1 receptor agonist semaglutide in patients with NASH are not known
- This phase 2 trial involving patients with NASH showed that treatment with semaglutide resulted in a significantly higher percentage of patients with NASH resolution than placebo.
- However, the trial did not show a significant between-group difference in the percentage of patients with an improvement in fibrosis stage
- This is from a trial published in the NEJM
-
Q. What is the most common cause of death in patients with NASH/NAFLD?
- The most common cause of death in patients with NASH/NAFLD is heart disease - need to screen and monitor for the same
-
Q. What is MAFLD?
- Metabolic dysfunction-associated fatty liver disease (MAFLD)
- "Nonalcoholic fatty liver disease (NAFLD) has become the most common cause of liver disease in many parts of the world, causing considerable liver-related (steatohepatitis, cirrhosis, liver failure, and hepatocellular carcinoma) and extra-hepatic morbidity and mortality (mainly cardiovascular disease, chronic kidney disease or certain types of extra-hepatic cancers).
- Recently, based on insights gained from the past two decades, an international panel of experts from 22 countries has taken the initiative to propose a new name and definition for NAFLD in adult individuals - that is, metabolic dysfunction-associated fatty liver disease .
- This proposed change in nomenclature is not simply a semantic revision, but may facilitate improved diagnosis of this common liver disease for health promotion, case identification, patient awareness, ongoing clinical trials, and health services delivery"
- Until now the exclusion of other chronic liver diseases, including “excess” alcohol intake, was necessary for the diagnosis of MAFLD.
- As the pathogenic process leading to MAFLD is now better understood and is seen to originate from an underlying state of systemic metabolic dysfunction, MAFLD is perceived as a standalone disease that warrants a positive diagnosis, rather than a “none”-disease rubric.
- Moreover, the rising prevalence of MAFLD makes its coexistence with other chronic liver diseases quite possible, further negating a diagnosis based on the exclusion of concomitant diseases.
- It is therefore our belief that this disease needs to be defined by its own set of positive criteria, rather than by exclusion criteria.
-
Idea is to make it a diagnosis of inclusion rather than the diagnosis of exclusion
-
Q. What are the diagnostic criteria for MAFLD ?
-
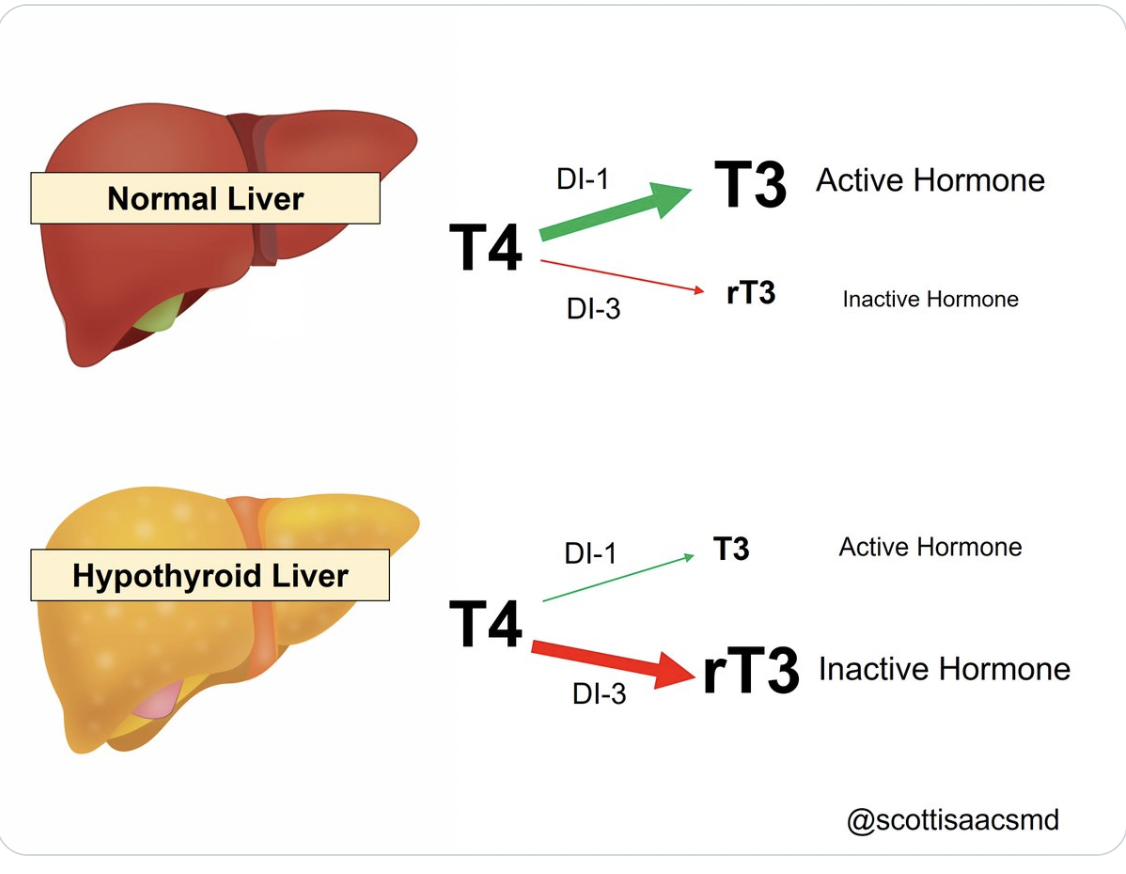
Q. What is Hepatic hypothyroidism?
- Effects of Resmetirom on Noninvasive Endpoints in a 36‐Week Phase 2 Active Treatment Extension Study in Patients With NASH - PMC
- Evidence suggests that NASH may be, in part, a condition of diminished liver thyroid hormone levels or hepatic hypothyroidism and that the incidence of clinical and subclinical hypothyroidism is higher in patients with NAFLD/NASH relative to age‐matched controls. Tag: NASH/NAFLD; NASH
- Effects of Resmetirom on Noninvasive Endpoints in a 36‐Week Phase 2 Active Treatment Extension Study in Patients With NASH - PMC
-
December 14th, 2022 - Updates from ADA 2023 Guidelines
-
Q. What is the grading for hepatic fibrosis?
-
- F0- No fibrosis
-
- F1- Mild
-
- F2- Moderate
-
- F3- Severe
-
- F4- Cirrhosis
-
-
Q. Patients with type 2 diabetes generally have what level of fibrosis?
- 20% of patients with type 2 diabetes have ≥F2 level of fibrosis
-
Q. What is the link between NAFLD and CKD?
- Patients with NAFLD have an increased risk of developing CKD
-
Q. Should Type 1 diabetes patients be screened for NAFLD?
- The prevalence of NAFLD/NASH is lower in type 1 diabetes
- Hence routine screening for type 1 diabetes is not recommended
-
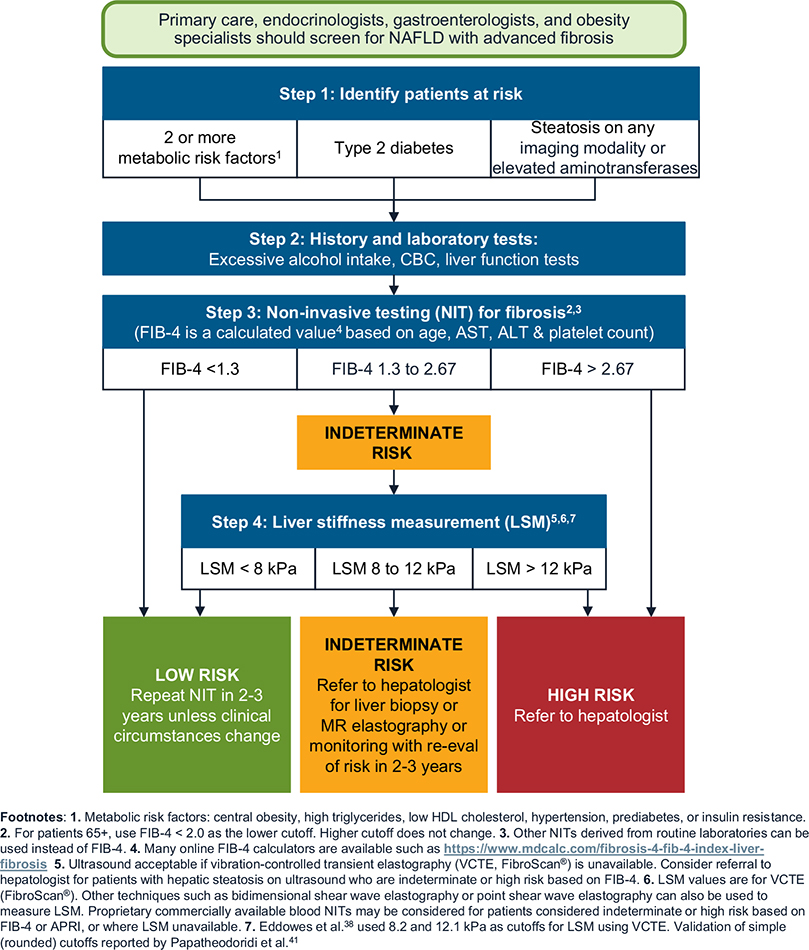
Q. Which is the most effective screening tool for screening for NASH/NAFLD in patients with type 2 diabetes and prediabetes?
- FIB-4 score is the most effective screening tool for screening for patients
-
Q. Is it okay to screen patients having ALT >40?
- No
- Significant patients have ≥F2 by the time they have ALT >40
-
Q. What are the ALT cut-off's given by the American college of Gastroenterology?
- More than 29-33 male
- More than 19-25 female
-
Q. What FIB-4 score is suggestive of high risk?
- <1.3- lower risk
- 1.3-2.67- moderate risk
- More than 2.67- high risk of fibrosis

-
Q. What is the problem with FIB-4 score?
-
- It has good specificity but low sensitivity
- A lot of type 2 diabetes fall in intermediate-risk and hence may be missed out
- hence a confirmation test is often required
-
- It is not recommended for pediatric patients
-
- It is less reliable for ages <35 years
-
- For ages > 65 years- a higher cutoff of 1.9-2.0 is suggested in place of 1.3
-
-
Q. Which is a good confirmatory test?
- Transient elastography
-
Q. What are the cut-off used in transient elastography?
- <8.0 kPA- has good negative predictive value to rule out advanced fibrosis- ≥ F3/F4 levels
- More than 12 KPA - must be referred to a hepatologist
-
Q. Which test has good use in early fibrosis?
- MR elastography
-
Q. Give the clinical care pathway for NASH/NAFLD as suggested by several guidelines.
-
Q. What type of diet has the best evidence for improving outcomes in NASH?
- Mediterranean diet
-
Q. Is obesity surgery helpful?
- Yes
- It is known to reduce all parameters in NASH including fibrosis
-
Q. Can obesity surgery lead to decompensation in patients with compensated cirrhosis?
- The risk is no greater compared to other surgeries
- However in patients already having decompensated cirrhosis, it is not recommended
-
Q. Can Pioglitazone reduce fibrosis in NASH?
- Yes
-
Q. Does GLP-1 receptor agonist reduce fibrosis ?
- It delays fibrosis as observed in two trials involving liver biopsies
- The evidence is for liraglutide and semaglutide
-
Q. What about SGLT2i?
- It is known to reduce steatosis
- But the impact on steatohepatitis and fibrosis is unknown
-
Q. Is currently any drug FDA-approved for NASH?
- No
-
Q. What about Vitamin E?
- Vitamin E is useful in non-diabetic patients with NASH
- No clear evidence of benefit in patients with diabetes
-
Q. Summarize the treatment option for NASH based on the new guidelines.
Some notes from UptoDate
- Most cases are diagnosed in the 40-the 50s
- Some reports suggest that NASH/NAFLD may be more common after cholecystectomy (but not in patients having gallstones) #ClinicalPearl
- AST/ALT ratio in NASH/NAFLD is <1 (SGOT/SGPT) while in Alcoholic liver disease it is more than 2 #ClinicalPearl
- the degree of AST/ALT elevation does not correlate with the severity of the disease #ClinicalPearl
- ALP may be elevated 2-3 times the ULN
- Serum ferritin has important role in NASH/NAFLD #ClinicalPearl
- Value >1.5 times the ULN is likely to be associated with greater progression of the liver disease
-
- Treatment of NASH/NAFLD
- Vaccination
- Hepatitis A
- Hepatitis B
- Pneumococcal vaccine
- Weight loss - 0.5-1 kg/week
- Biopsy proven NASH and fibrosis with stage ≥2 and not having diabetes - Vitamin E - 800 IU/day (C. EVION- 400 IU - twice a day)
- Diabetes patients
- Metformin
- Pioglitazone
- Liraglutide
- If after weight loss - repeat ALT/AST after 3 months
- if it has not come to normal - look for other causes
-