-
Credits:
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani -
MIND DIET
-
Q. What is the MIND diet ?
- The MIND diet is a dietary pattern that combines elements of the Mediterranean diet and the DASH (Dietary Approaches to Stop Hypertension) diet.
- It is specifically designed to promote brain health and reduce the risk of cognitive decline and dementia.
- The MIND diet emphasizes the consumption of foods such as green leafy vegetables, nuts and berries, fish, and olive oil, which are believed to be beneficial for brain health.
- It also limits the intake of foods high in saturated fat and sugar, such as red meat, butter, pastries, and fried foods. The MIND diet has been associated with a decreased risk of dementia and Alzheimer's disease.
-
Q. Give me the history of MIND Diet
- he Mediterranean-DASH Diet Intervention for Neurodegenerative Delay (MIND) was introduced in 2015 by Dr. Martha Clare Morris and colleagues.
- The study identified 15 dietary components as either "brain-healthy" or unhealthy.
- Participants with the highest MIND diet scores had a significantly slower rate of cognitive decline compared to those with the lowest scores.
- The MIND diet showed greater cognitive effects than either the Mediterranean or the DASH diet alone.
-
Q. What are the dietary components to avoid according to the MIND Diet ?
- Recommended limitations in the MIND diet include:
- Less than 5 servings a week of pastries and sweets
- Less than 4 servings a week of red meat
- Less than one serving a week of cheese and fried foods
- Less than 1 tablespoon a day of butter or stick margarine
- Recommended limitations in the MIND diet include:
-
Q. What were the results of the MIND diet published recently in the NEJM ?
- The study investigated the effects of the MIND diet on cognitive decline.
- The MIND diet is a combination of the Mediterranean and DASH diets, designed to promote brain health.
- Participants were randomly assigned to either the MIND diet or a control diet with mild caloric restriction.
- MIND diet that was designed to improve brain health, cognitive function and brain imaging outcomes at 3 years did not differ significantly between participants who followed the MIND diet and those who followed a control diet with a mild caloric restriction (Ref 2)
-
Q. What were the limitation of this study ?
- The 3-year duration of the 2023 study may have been too short to show significant improvement in cognitive function.
-
Mediterranean diet
-
Q. What is the definition of a Mediterranean diet ?
- A Mediterranean diet is typically high in fruits, vegetables, whole grains, beans, nuts, and seeds.
- It includes olive oil as an important source of monounsaturated fat.
- It allows low to moderate wine consumption.
- It generally includes low to moderate amounts of fish, poultry, and dairy products.
- It includes little red meat.
-
Q. What are the proven health benefits of a Mediterranean diet and trials showing those benefits ?
- Health Benefits:
- Associated with several health benefits, but unclear if benefits come from a single component or a combination.
- PREDIMED Trial:
- Study involving persons at high cardiovascular risk, the incidence of major cardiovascular events was lower among those assigned to a Mediterranean diet supplemented with extra-virgin olive oil or nuts than among those assigned to a reduced-fat diet.
- CARDIOPREV Trial (2022):
- Fewer major cardiovascular events compared to a low-fat diet after seven years.
- Network Meta-Analysis:
- Lower risk of all-cause mortality, cardiovascular mortality, stroke, and nonfatal myocardial infarction compared to minimal intervention.
- Observational Studies:
- Lower overall and cardiovascular mortality.
- Reduced incidence of Parkinson's, Alzheimer's, and various cancers.
- Type 2 Diabetes:
- See below
- Health Benefits:
-
Q. What are the benefits of Mediterranean diet in Type 2 Diabetes mellitus ?
- Glycemic Control:
- Mediterranean diet improves glycemic control compared to various control diets.
- Four-Year Trial:
- 215 overweight patients with newly-diagnosed type 2 diabetes.
- Mediterranean diet led to less need for antihyperglycemic drugs (44% vs 70%).
- Greater weight loss after one year, but no difference at years 3 and 4.
- Increase in HDL and decrease in triglycerides were significantly better in the Mediterranean diet group.
- Post-Trial Monitoring:
- Delayed time to initiation of glucose-lowering medication (median 4.8 vs 2.8 years with low-fat diet).
- Cardiovascular Benefits:
- Reduces incidence of major cardiovascular events in high-risk patients, including those with diabetes.
- Glycemic Control:
-
Q. What kind of fat is present in Mediterranean diet ?
- The Mediterranean diet is rich in healthy fats.
- The primary source of fat in the Mediterranean diet is olive oil.
- The diet also includes monounsaturated and polyunsaturated fats from sources such as seeds and nuts.
-
Q. What is the difference between MUFA and PUFA ?
- MUFA stands for monounsaturated fatty acids, while PUFA stands for polyunsaturated fatty acids.
- MUFA has one double bond in its chemical structure, while PUFA has multiple double bonds.
- MUFA is found in foods like olive oil, avocados, and nuts, while PUFA is found in foods like fatty fish, vegetable oils, and seeds.
- MUFA is considered a healthier type of fat compared to saturated fats, as it can help improve cholesterol levels and reduce the risk of heart disease.
- PUFA is divided into two main types: omega-3 fatty acids and omega-6 fatty acids. Omega-3 fatty acids are known for their anti-inflammatory properties and are found in fatty fish, flaxseeds, and walnuts. Omega-6 fatty acids are essential for the body but should be consumed in moderation, as excessive intake can promote inflammation.
- Both MUFA and PUFA are important components of a healthy diet and should be included in moderation as part of a balanced eating plan.
-
Q. Which is better MUFA or PUFA ?
- MUFA (Monounsaturated Fatty Acids):
- Pros:
- Improves heart health by lowering LDL cholesterol.
- May help control blood sugar levels.
- Found in olive oil, avocados, and nuts.
- Cons:
- Less effective than PUFA in reducing inflammation.
- Pros:
- PUFA (Polyunsaturated Fatty Acids):
- Pros:
- Reduces inflammation.
- Lowers bad cholesterol, thus reducing heart disease risk.
- Contains essential fatty acids like omega-3 and omega-6.
- Cons:
- Omega-6 fatty acids, if consumed in excess, may promote inflammation.
- Pros:
- Comparison:
- Heart Health: Both are good but PUFA is generally considered more effective in reducing heart disease risk.
- Inflammation: PUFA is more effective in reducing inflammation.
- Blood Sugar: MUFA may have a slight edge in blood sugar control.
- Conclusion:
- Neither is definitively "better"; both have unique benefits and drawbacks.
- A balanced intake of both is generally recommended for a well-rounded, healthy diet.
- MUFA (Monounsaturated Fatty Acids):
-
Key point- MUFA reduces LDL , while PUFA reduces inflammation
-
Q. Does Mediterranean diet reduce weight ?
- Short-Term Effects:
- Some studies show greater weight loss in the first year when following a Mediterranean diet compared to low-fat diets.
- Long-Term Effects:
- Weight loss tends to equalize with other diets like low-fat diets in the long term (e.g., after 3-4 years).
- Quality Over Quantity:
- Focuses on nutrient-dense foods rather than calorie restriction, making it more sustainable.
- Additional Benefits:
- While weight loss may not be the primary focus, the diet is associated with improvements in metabolic health, which can indirectly support weight management.
- Variable Results:
- Individual results can vary based on adherence to the diet and other lifestyle factors like exercise.
- Conclusion:
- The Mediterranean diet may offer moderate weight loss benefits, especially in the short term, but its primary strengths lie in overall health improvement.
- Short-Term Effects:
-
Q. Give me the pyramid for Mediterranean diet ?
-
Q. What are the suggestions for Indian version of Mediterranean diet ?
-
Proteins
- Lean Meat: Opt for skinless chicken and turkey.
- Fish: Include oily fish like mackerel, sardines, or local varieties rich in Omega-3s.
- Plant-Based Proteins: Lentils, chickpeas, and other pulses can replace meat in many dishes.
- Dairy: Use low-fat or skimmed milk, yogurt, and paneer as alternatives to full-fat versions.
-
Fruits and Vegetables
- Local Produce: Incorporate a variety of seasonal fruits and vegetables.
- Leafy Greens: Include Indian greens like spinach (palak), fenugreek (methi), and mustard leaves (sarson).
-
Grains
- Whole Grains: Opt for whole-wheat roti, brown rice, or millets like ragi and jowar over white rice and bread.
- Legumes: Add a variety of lentils and pulses such as mung, toor, and chana dal.
-
Fats
- Cooking Oils: Use olive oil or canola oil for cooking, and mustard oil for pickling.
- Nuts and Seeds: Incorporate almonds, walnuts, and flaxseeds for snacks or as additions to meals.
-
Herbs and Spices
- Fresh Herbs: Use cilantro, mint, and basil generously.
- Spices: Incorporate spices like turmeric, cumin, and coriander that have health benefits.
-
Beverages
- Water: Make it the primary beverage; avoid sugary drinks and excessive amounts of caffeine.
- Tea: Opt for green tea or herbal teas like chamomile.
-
Snacks
- Healthy Options: Choose fruits, nuts, or whole-grain crackers over processed snacks.
- Fried Foods: Limit or avoid fried snacks like samosas or pakoras.
-
Other Tips
- Portion Control: Pay attention to serving sizes.
- Meal Timing: Stick to regular meal timings, including breakfast.
- Exercise: Complement the diet with regular physical activity.
-
-
Q. Are the benefits of Mediterranean diet mainly because of olive oil ?
- Olive oil is the main source of fat in the Mediterranean diet.
- Olive oil has direct effects on the immune system and inflammatory responses due to its content of tocopherols, polyphenols, and mono-unsaturated fatty acids.
- Olive oil also has indirect effects on the immune system and inflammation by providing lower saturated fats and a balanced ratio of linoleic and alpha-linolenic acid.
- The health benefits attributed to olive oil are specifically related to extra virgin olive oil (EVOO) intake, which has high nutritional quality and multiple positive effects on health.
- However, the overall benefits of the Mediterranean diet are not solely due to olive oil. The dietary pattern as a whole, including the consumption of fruits, vegetables, whole grains, legumes, nuts, and seeds, contributes to the favorable health effects of the Mediterranean diet.
-
DASH diet
-
Q. What is the DASH diet ?
- The DASH (Dietary Approaches to Stop Hypertension) diet is a dietary pattern.
- It includes four to five servings of fruit and vegetables per day.
- It also includes two to three servings of low-fat dairy per day.
- The DASH diet recommends consuming less than 25 percent of daily caloric intake from fat.
- It has been found to lower systolic and diastolic blood pressure more than a diet rich in fruits and vegetables alone.
- Combining the DASH diet with low-sodium intake further decreases blood pressure.
- The DASH diet has been associated with a lower risk of colorectal cancer, cardiovascular disease, premature mortality, and gout in men
-
Q. What is the history of DASH diet ?
- This was mainly introduced by the NIH in 1990s
- It has strong fundamental research basis with several RCT conducted with regards to the diet
- The DASH (Dietary Approaches to Stop Hypertension) diet was introduced in 1996 and published in the New England Journal of Medicine in 1997.
-
Q. What is the sodium intake in the DASH diet ?
- All versions of the DASH diet studied provided about 3000 mg of sodium, which is above the recommended amount but below the average American intake.
- Greater reductions in blood pressure can be achieved by restricting sodium to less than 2300 mg/day, and even more so with a 1500 mg/day restriction.
-
Q. What are the proven clinical benefits of the DASH diet ?
- Research consistently shows that DASH lowers blood pressure in people with both high and normal blood pressure, even without sodium restriction.
- DASH also lowers serum uric acid levels, reducing the risk of gout in people with hyperuricemia.
- An 8-week controlled trial found that the DASH diet lowered cardiovascular risk compared to other diets, including a fruit and vegetable-rich diet.
- A recent meta-analysis and the Atherosclerosis Risk in Communities (ARIC) cohort study suggest that adherence to the DASH diet may help prevent diabetes and kidney disease.
-
Anti-inflammatory diet
-
Q. What is the anti-inflammatory diet ?
- An anti-inflammatory diet is a eating plan that aims to reduce inflammation in the body
- It includes foods that are rich in nutrients, fiber, and phytochemicals.
- The diet limits foods commonly found in a Western diet that can contribute to inflammation.
- It emphasizes fresh fruits, vegetables, legumes, nuts, seafood, and olive oil.
- The Mediterranean diet and DASH diet are examples of anti-inflammatory diets.
- Research suggests that an anti-inflammatory diet can decrease markers of inflammation and improve symptoms in certain conditions like cardiovascular disease and rheumatoid arthritis.
- The diet may also support a diverse and beneficial gut microbiome, which can help prevent inflammation-related conditions.
-
Q. What food substances are known to increase and which are known to reduce inflammation ?
- Foods that may increase inflammation:
- Sweetened beverages like soda, juice drinks, iced tea
- Excess of refined carbohydrate foods like white bread, pasta, rice
- Fried foods
- Processed high-fat meats like bacon, sausage, hot dogs
- Saturated fats like full-fat dairy from cream and butter, partially hydrogenated oils, fatty cuts of meat and poultry
- Excess alcohol
- Foods that may reduce inflammation:
- Dark chocolate with at least 70% or higher cocoa solids
- Herbs, spices (turmeric, ginger)
- Moderate amounts of alcohol (wine, beer)
- Fruits
- Vegetables
- High-fiber whole grains
- Legumes
- Monounsaturated fats (avocados, olive oil, nuts, nut butters, seeds)
- Polyunsaturated omega-3 fats (walnuts, flaxseeds, chia seeds, and aquatic foods including salmon, herring, sardines, mackerel)
- Tea
- Coffee
- Foods that may increase inflammation:
-
Q. Is there any clinical evidence for this concept of anti-inflammatory diet ?
- A study called the Anti-Inflammatory Diet In Rheumatoid Arthritis randomized controlled crossover trial found that patients with rheumatoid arthritis who followed an anti-inflammatory diet had a significant decrease in disease activity score.
- Following a vegetarian diet for at least 2 years has been associated with lower levels of C-reactive protein, a pro-inflammatory marker, compared to omnivores with no dietary restrictions.
- A randomized trial on participants at risk for cardiovascular disease showed that a Mediterranean diet, which includes anti-inflammatory foods, significantly decreased markers of inflammation compared to a low-fat diet.
- There is emerging research on the effects of high-fiber plant-rich diets in preventing low-grade inflammation associated with metabolic diseases like cardiovascular disease and type 2 diabetes.
- Some studies suggest that a vegan diet, Mediterranean diet, and elimination diet (avoiding certain food allergens) can suppress pro-inflammatory cells and improve symptoms in patients with rheumatoid arthritis.
-
Q. What is the concept of 'leaky gut' ?
- Leaky gut refers to increased intestinal permeability, allowing bacteria, viruses, toxins, and allergens to escape from the gut into the bloodstream and the rest of the body.
- It is observed in inflammatory conditions like rheumatoid arthritis, Hashimoto thyroiditis, celiac disease, Crohn's disease, multiple sclerosis, obesity, non-alcoholic fatty liver disease, and major depression.
- The small and large intestines are lined with a layer of epithelial cells that create a barrier of tight junctions to prevent bacterial translocation.
- Abnormal changes in the gut microbiota, caused by factors like chronic stress, medications (antibiotics, non-steroidal anti-inflammatory drugs), or food toxins, can disrupt the intestinal barrier and increase the risk of disease.
- The initial trigger for dysbiosis (imbalanced gut microbiota) and leaky gut is not yet clear.
- Certain nutrients like glutamine and tryptophan have been shown to improve intestinal permeability by strengthening tight junctions.
- Fiber in the diet can improve gut bacteria diversity and strengthen the intestinal barrier.
- The relationship between dysbiosis, leaky gut, and inflammatory conditions requires more research to understand and develop potential treatments.
-
** intermittent fasting **
-
Q. What is intermittent fasting ?
- Intermittent fasting is a diet regimen that involves cycling between periods of fasting and periods of unrestricted eating.
- It can be done in different ways, such as fasting on alternate days, fasting for whole days with a specific frequency per week, or following a designated time frame for fasting each day.
- The goal of intermittent fasting is to change body composition by reducing fat mass and weight, and to improve markers of health like blood pressure and cholesterol levels.
- It is rooted in traditional fasting practices that have been used for health and spiritual benefits.
- Prolonged very low calorie diets can cause the body to adapt and prevent further weight loss, but intermittent fasting aims to address this issue by cycling between low calorie periods and normal eating.
-
Q. What are the three main types of intermittent fasting ?
- Alternate-day fasting- one day eating and the other day very low calorie or no eating
- Whole-day fasting- here two days of the week you fast- and rest of the day you eat normall
- This is called 5:2 fast - where 5 days you eat and 2 days you fast or just take 400-500 calorie
- Time-restricted feeding- fasting for a particular length of time everyday. eg: meals only eaten between 8 am to 3 pm- then fast. 16:8 eating (16 hrs fast and 8 hrs of feeding period is an example of the same)
-
Q. Which are the three most studied intermittent fasting regimens ?
-
- Alternate day feeding
-
- 5:2 weekly cycles- 5 days eating and 2 days fasting
-
- 16:8 time restricted feeding
-
-
Q. What is the result of systemic review on intermittent fasting done for weight loss ?
- A systemic review of 40 studies found that intermittent fasting was better compared to standard over a period of 10-12 weeks with additional 4-5 kg weight loss
- However there were a lot of inconsistencies in the studies included in the review
- In an RCT of about 100 obese subjects- intermittent fasting had no benefit over daily calorie restriction
- Another trial of 16:8 time restricted feeding also found no benefit beyond similar calorie restriction. Though weight loss was slightly higher in the fasting group the difference was not statistically significant (this was the trial published in NEJM)
-
Q. Do you have increased appetite on the days that you don't fast ?
- No
- this is not the case
-
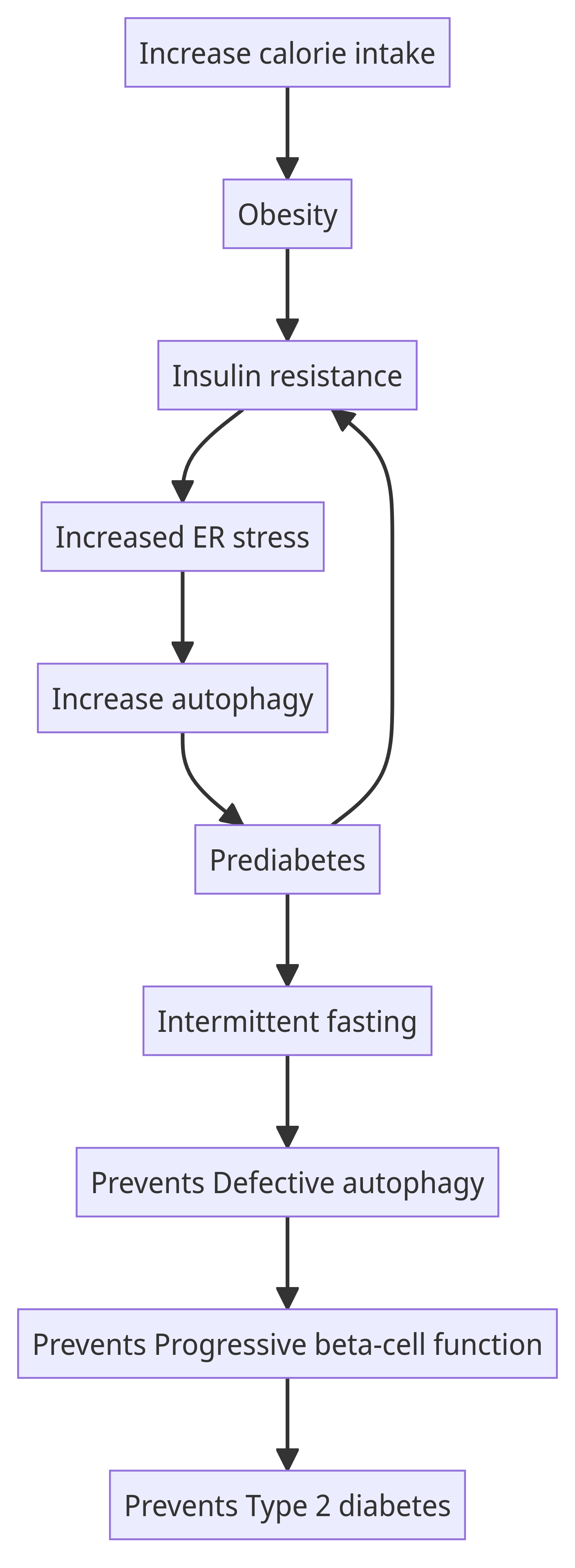
Q. How does intermittent fasting help in diabetes from pathophysiological perspective ?
-
Q. Explain the concept of Autophagy in simple words
- Autophagy is like the recycling system inside your cells. Imagine your cell is a house, and over time, it accumulates waste, broken furniture, and old toys. Autophagy is the process where the cell cleans up this mess by breaking down the old or damaged parts and using the materials to build new, functional parts. This helps the cell stay healthy and efficient. Just like recycling in real life helps the environment, autophagy helps keep cells in good shape.
-
Q. What is the result from a meta-analysis on intermittent fasting published in JCEM in 2021
- Current evidence suggests that IF is associated with greater weight loss in patients with T2DM compared with a standard diet, but with a similar impact on glycemic control.
- This is based on the study: Borgundvaag E, Mak J, Kramer CK. Metabolic impact of intermittent fasting in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of interventional studies. The Journal of Clinical Endocrinology & Metabolism. 2021 Mar 1;106(3):902-11.
-
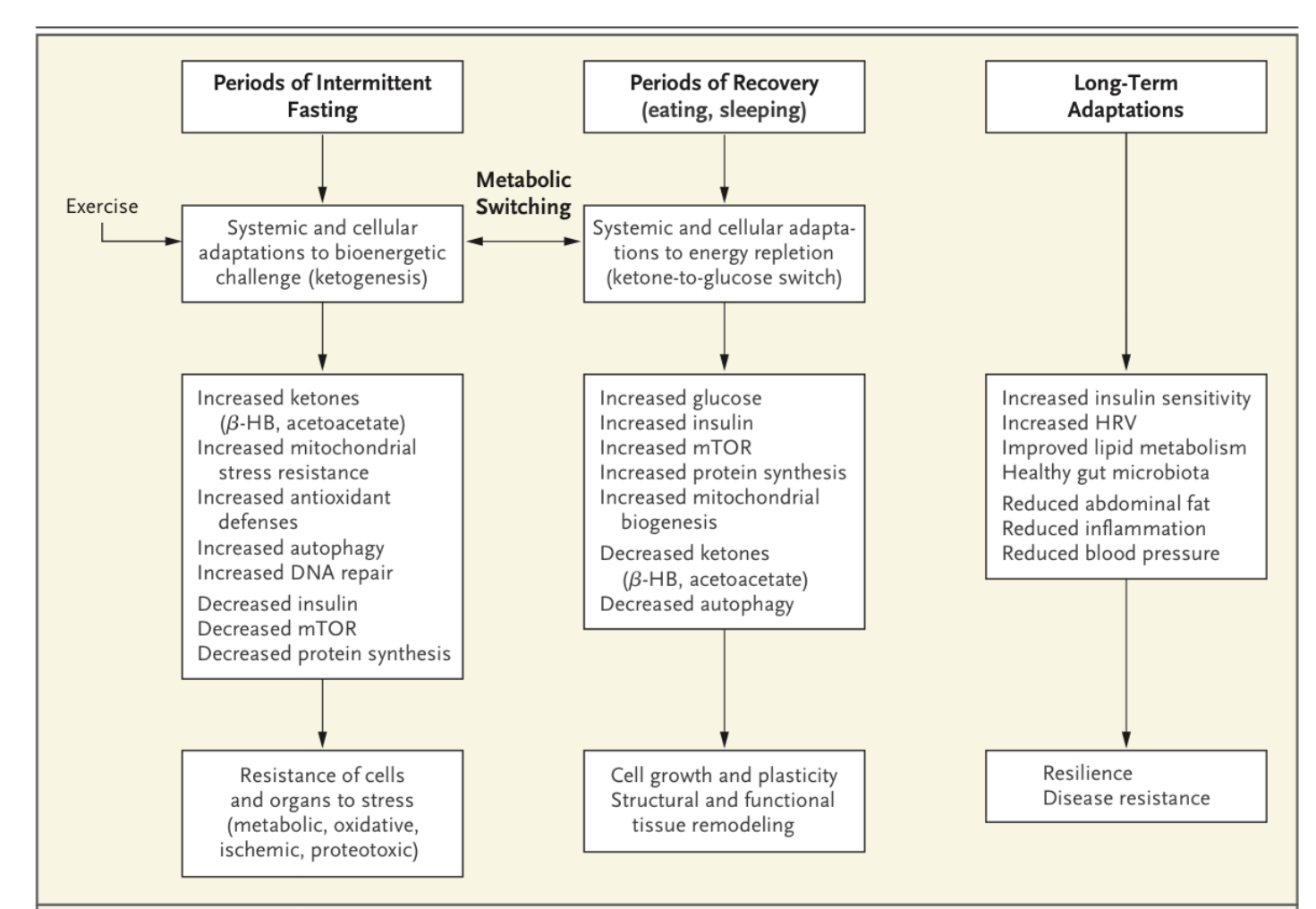
Q. What were the key points from review on intermittent fasting published in NEJM in 2019 ?
- Intermittent fasting has shown broad-spectrum benefits for various health conditions, including obesity, diabetes, cardiovascular disease, cancers, and neurologic disorders.
- Animal models suggest that intermittent fasting improves health throughout the lifespan, while clinical studies have mainly focused on short-term interventions.
- The molecular mechanisms behind the health benefits of intermittent fasting include proteostasis and autophagy, stress resistance, mitochondrial biogenesis, cell survival, and neuroendocrine signaling.
- Intermittent fasting may have potential applications in the prevention and treatment of cancer, as well as in neurodegenerative diseases.
- Implementing intermittent fasting requires adequate information, ongoing communication, support, and regular positive reinforcement from physicians.
-
Q. What kind of fuel switch occurs when we are fasting ?
- With intermittent fasting the fuel switches from liver generated glucose to adipose cell generated ketones
-
Q. What are the three important bioenergetic sensors ratios that you need to be aware about ?
- NAD+ to NADH
- ATP to AMP
- acetyl CoA to CoA
-
Q. What happens to the three ratio NAD+ to NADH, ATP to AMP, acetyl CoA to CoA during fasting and feeding ?
- NAD+ to NADH Ratio:
- Fasting: Generally increases, favoring oxidative pathways and activating proteins like sirtuins that promote stress resistance and repair mechanisms.
- Feeding: Typically decreases as more NADH is produced during nutrient metabolism, which can slow down catabolic pathways and encourage anabolic processes like growth and storage.
- ATP to AMP Ratio:
- Fasting: Decreases, leading to an increase in AMP levels that activate AMPK, a kinase that promotes catabolic processes like fatty acid oxidation and inhibits anabolic processes like protein synthesis.
- Feeding: Increases as ATP is generated through nutrient metabolism, leading to decreased AMPK activity and the promotion of growth and storage processes.
- Acetyl CoA to CoA Ratio:
- Fasting: Decreases as acetyl CoA is used in catabolic pathways like the Krebs cycle and fatty acid oxidation.
- Feeding: Increases as acetyl CoA accumulates from carbohydrate and fatty acid metabolism, often leading to the initiation of anabolic processes like lipid synthesis.
- In summary, fasting generally pushes these ratios in a direction that promotes catabolic processes, stress resistance, and repair. Feeding does the opposite, encouraging anabolic processes like growth and storage.
- NAD+ to NADH Ratio:
-
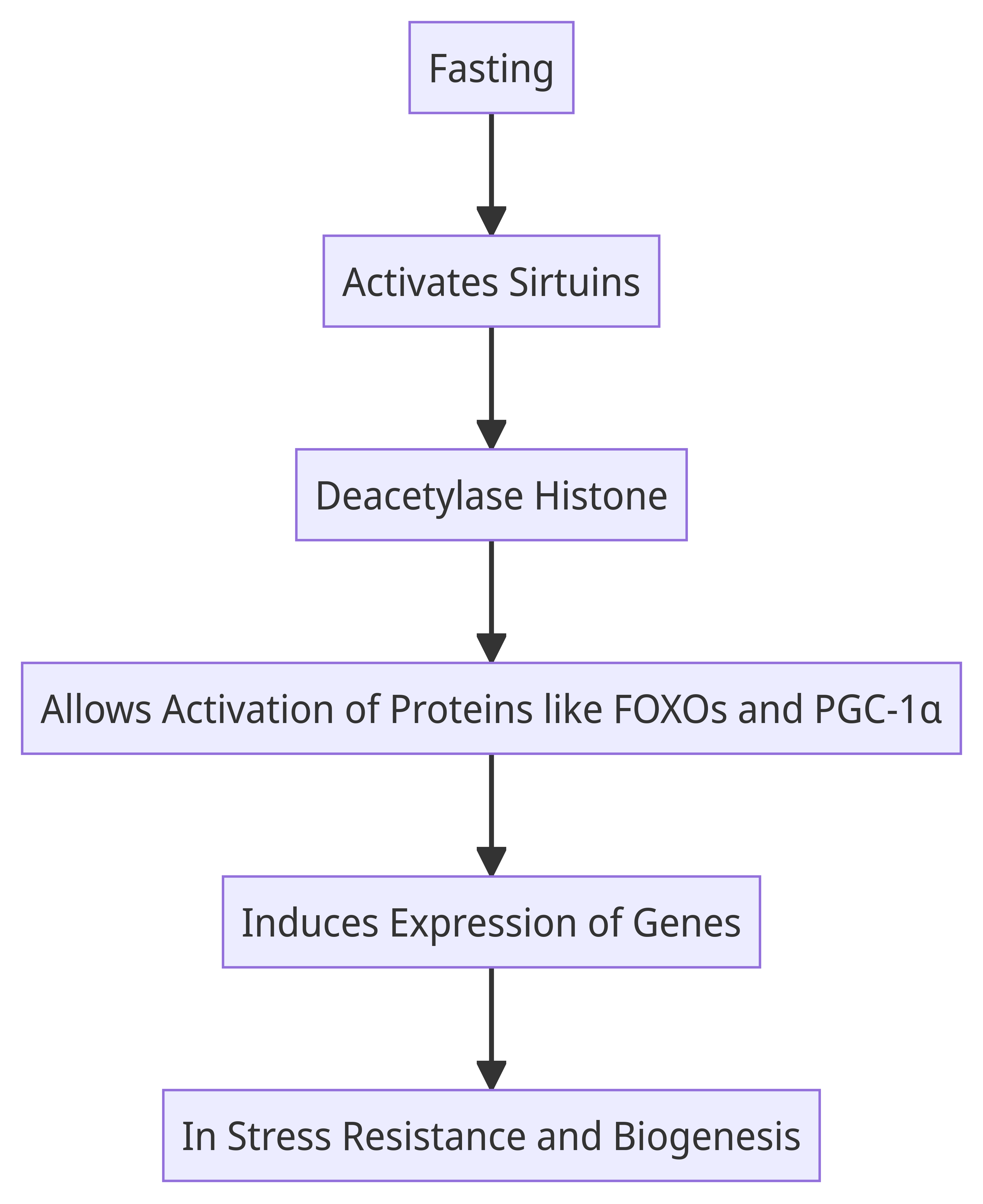
Q. What are Siruitins ?
- https://www.loom.com/share/865c7f1558134923b4d5e5052203285e
- They are enyzymes
- There are 7 of them SIRT1 to SIRT7
- They are stress adaptors and nutrient sensors
- they are histone deacetylases
- Histone deacetylases (EC 3.5.1.98, HDAC) are a class of enzymes that remove acetyl groups (O=C-CH3) from an ε-N-acetyl lysine amino acid on a histone, allowing the histones to wrap the DNA more tightly. 2 (https://en.wikipedia.org/wiki/Histone_deacetylase#cite_note-Milazzo_2020-2) This is important because DNA is wrapped around histones, and DNA expression is regulated by acetylation and de-acetylation. Its action is opposite to that of histone acetyltransferase. HDAC proteins are now also called lysine deacetylases (KDAC), to describe their function rather than their target, which also includes non-histone proteins
-
Q. What is SIRT1 ?
- It is a member of Sirtuins
- It is basically an antioxidant
- It works like nutrient restriction
- In case of increase ROS , the SIRT1 prevents the effect of ROS on the DNA
- This prevents DNA breakdown and works as anti-agining
-
Q. What is the role of SIRT1 in Cardiology ?
- SIRT1 increases Nitrous oxide #important
-
Q. What is the role of SIRT1 in Diabetes ?
- SIRT1 prevents the endothelial dysfunction and microvascular complications produced by hyperglycemia
- ^^SIRT1 improves insulin sensitivity^^
- SIRT6 also does this.
- If a mice has SIRT6 overexpression and given high caloric diet, he is protected from the effects of calorie excess
- SIRT6 also works in the liver to prevent NASH/NAFLD
- There is a correlation between SIRT6 and Hypertriglyceridemia
- both SIRT1 and SIRT6 increase the beta-cell induced insulin secreation
-
Q. What role to Sirtuins play in intermittent fasting ?
- Sirtuins are a type of deacetylase enzymes that play a role in intermittent fasting.
- Intermittent fasting activates sirtuins, specifically SIRT1, which is involved in regulating cellular responses to energy restriction.
- Sirtuins, including SIRT1, deacetylate proteins such as FOXOs and PGC-1α, leading to the expression of genes involved in stress resistance and mitochondrial biogenesis.
- Activation of sirtuins by intermittent fasting promotes cell survival, enhances stress resistance, and supports improvements in health and disease resistance.
-
Q. Explain the entire concept of fasting in simple words ?
- The human body has two states- fasting and post-absorptive state
- during the fasting state- the body uses the state for mainly clean-up and maintaince
- It clears off the reactive oxygen species (ROS)
- ROS are are little sparks formed during the various metabolic process in the human body
- the post-absorptive state is the state for building and storage
- this is the state when a lot of ROS are actually formed
- So the longer the fasting state- the more the time the body gets for the cleaning and maintenance process
- Sirutins are the switches which convert the body to the various states
-
Q. What happens to fuel switches during fasting and post-absorptive state ?
- In the post-absorptive state the body breaksdown the carbohydrates to glucose which is either immediatley used for energy or stored in the liver in form of glycogen
- The body stores the fat in the diet in form of triglyceride in the adipose tissue
- In the fasting state the body uses first the glycogen and then further fasting it starts breaking down the triglycerides to fatty acid and glycerol
- The fatty acid is then used by the liver to be converted to ketones which are used as an alternative fuel for the human body
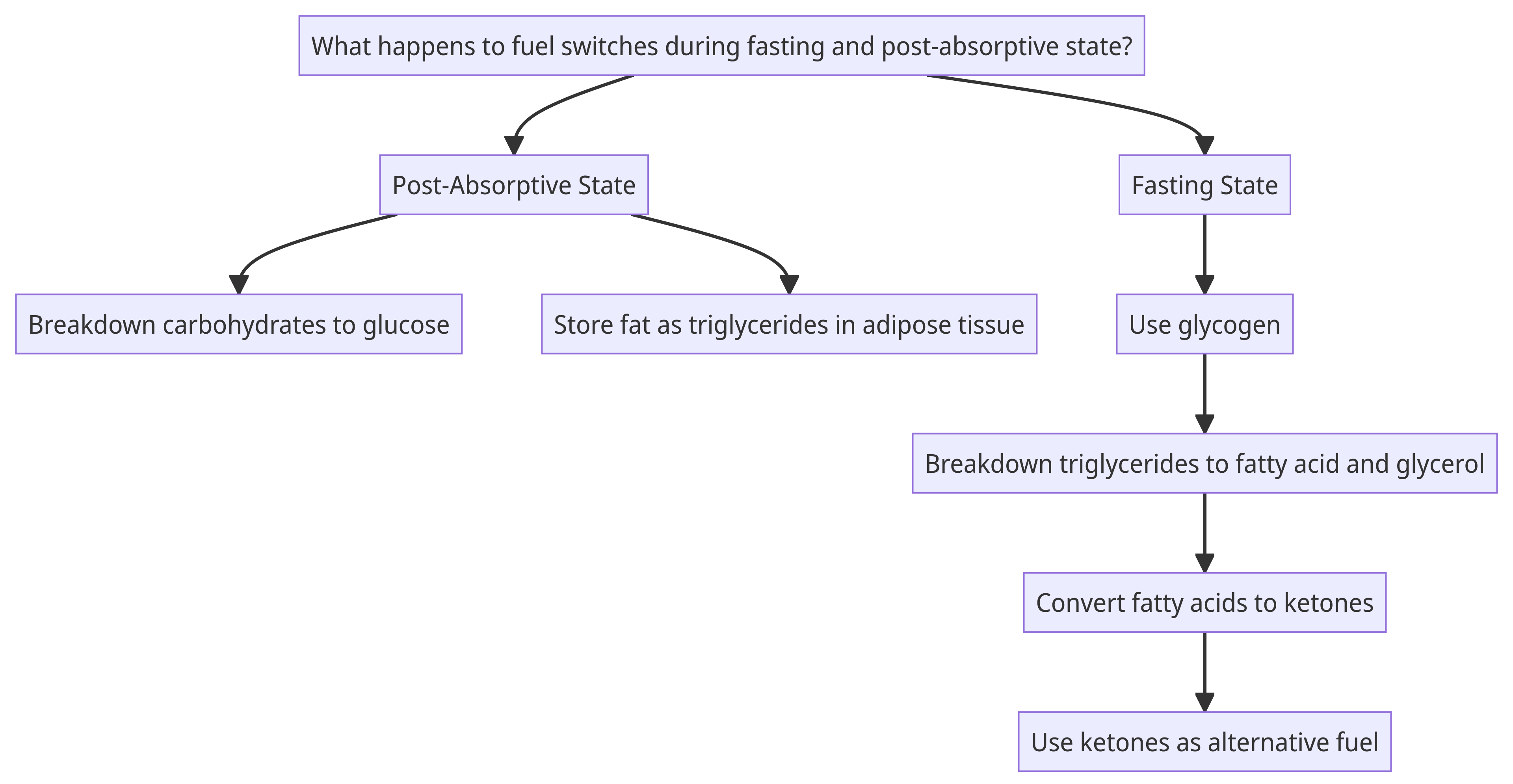
-
Q. What is the importance of measuring blood ketone levels with regards to fasting state ?
- The time when the body starts converting the fatty acid to ketone is a period of adequate fasting period for the human body
- Hence measuring of the ketones in the blood may be a useful marker for intermittent fasting
-
Q. Are ketones just an alternative fuel ?
- No
- ketones are also signals to the body that the switch has occurred and influence the deep fasting protocols in the body which we talked about earlier
-
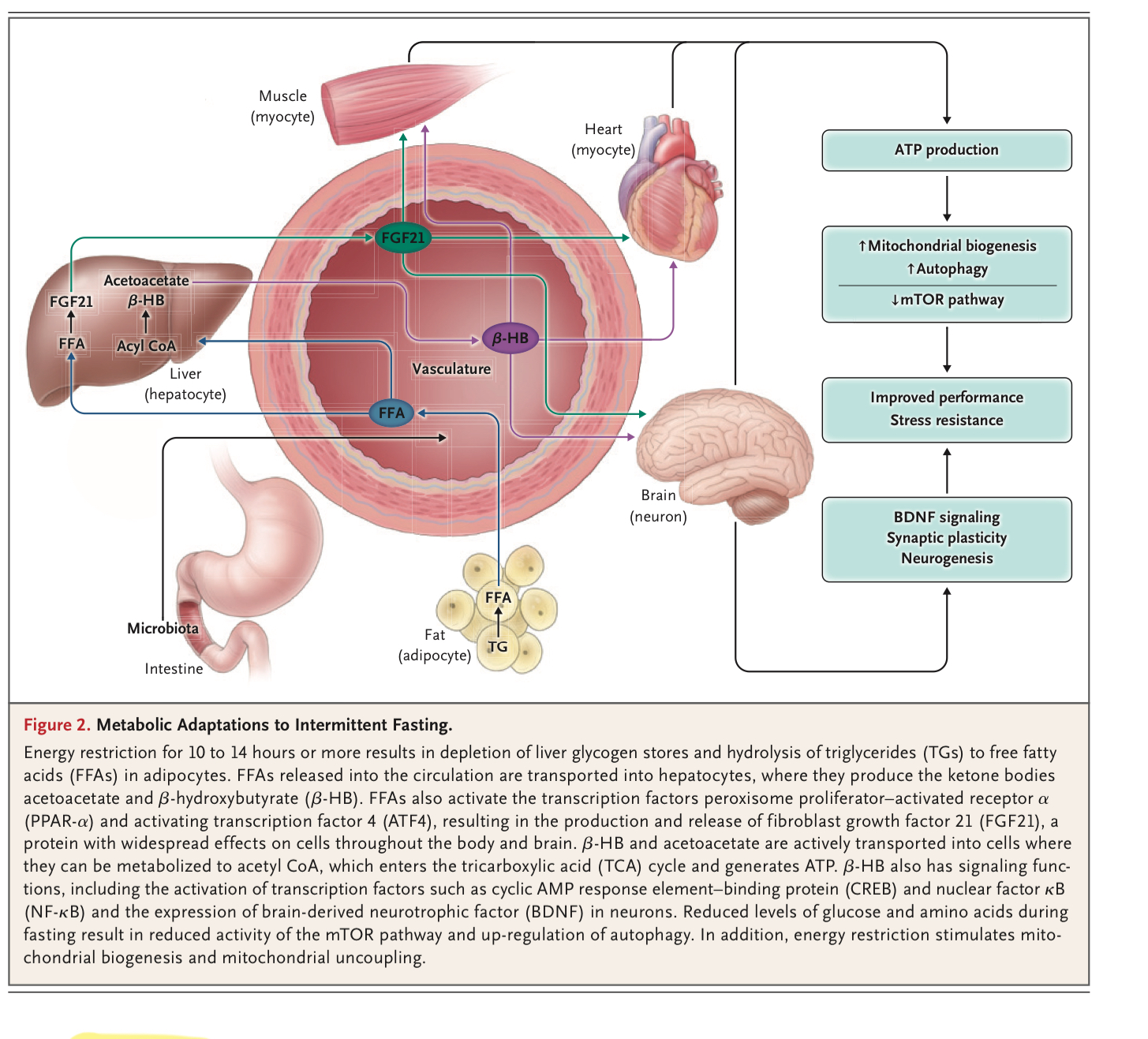
Q. Summarize the metabolic adaptations to fasting based on the NEJM article ?
- Energy restriction for 10-14 hours depletes liver glycogen and breaks down triglycerides to free fatty acids (FFAs).
- FFAs are transported to liver cells, where they produce ketone bodies like acetoacetate and B-HB.
- FFAs activate transcription factors PPAR-a and ATF4, leading to the release of FGF21, a protein affecting cells globally.
- Ketone bodies are used by cells to generate ATP through the TCA cycle.
- Beta-hydroxybutyrate (BOHB) has signaling functions, activating transcription factors like CREB and NF-B, and increasing BDNF expression in neurons.
- Reduced glucose and amino acids during fasting lower mTOR activity and increase autophagy.
- Energy restriction also stimulates mitochondrial biogenesis and uncoupling.
-
Q. Explain the above in simple words ?
- When you don't eat for 10-14 hours, your liver uses up its sugar stores and starts breaking down fat into something called free fatty acids (FFAs).
- These FFAs go to the liver, where they help make something called ketone bodies, which can be used for energy.
- FFAs also trigger some special proteins that have effects all over the body.
- The ketone bodies are used by your cells to make energy.
- One of the ketone bodies, called B-HB, also helps send signals in the body, including in the brain, to keep things running smoothly.
- Not eating for a while also makes your body clean up old cell parts and be more efficient, a process called autophagy.
- Finally, not eating for some time helps your cells make more energy factories (mitochondria) and work more efficiently.
-
Q. What is the importance of Ketones on the brain ?
- Ketones stimulate the production of BDNF. BDNF stands for Brain-Derived Neurotrophic Factor
-
Q. What is the importance of BDNF ?
- BDNF stands for Brain-Derived Neurotrophic Factor.
- It's a protein that plays a crucial role in the health and growth of neurons (nerve cells) in the brain.
- BDNF is often referred to as a "fertilizer" for the brain because it helps neurons grow, survive, and form new connections.
- This protein is particularly important for memory, learning, and higher-level thinking.
- In simple terms, BDNF is like "brain food" that helps your brain cells stay healthy and work better.
- It's especially important for things like learning new things and remembering them later.
-
Q. Explain the correlation between fasting and Autophagy in simple words
- Autophagy is a natural process in our cells that helps to remove damaged or unnecessary components and recycle them for energy. Fasting, or periods of not eating, can actually stimulate autophagy. When we fast, our cells experience a mild stress, and in response, they activate autophagy to help clean up and repair themselves. This can have many benefits for our health, including improved cellular function, increased stress resistance, and protection against certain diseases. So, fasting can be a way to promote autophagy and support the overall health of our cells.
-
Q. What is the bottom line with regards to intermittent fasting ?
- There is no significant difference in weight loss amounts or body composition changes between intermittent fasting and continuous calorie restriction.
- Intermittent fasting does not lead to an overall increase in appetite, despite significant weight loss and decreases in appetite-suppressing hormone levels.
- Intermittent fasting is not more effective than daily calorie restriction for weight loss.
- There are no significant differences in blood pressure, heart rate, fasting glucose, and fasting insulin between intermittent fasting and daily calorie restriction.
- The dropout rate is higher in the intermittent fasting group compared to the daily calorie restriction group.
- Intermittent fasting may be more beneficial for individuals who typically eat one or two meals a day or do not eat for long stretches of time.
- More high-quality studies are needed to determine the direct effects and possible benefits of intermittent fasting.
-
Q. Explain this entire thing in simple words ?
- When you fast or go without food:
- Your body creates a balance that helps repair cells and fight stress.
- Your body also breaks down fats and other nutrients for energy instead of building up new stuff like fats and proteins.
- When you eat:
- Your body is more focused on using the food to grow and store energy for later.
- So basically, fasting helps your body focus on cleaning and repairing, while eating directs your body to grow and store energy.
- When you fast or go without food:
-
Q. Give some practical ideas how physicians and prescribe intermittent fasting to their patients ?
- Physicians can incorporate intermittent fasting prescriptions for early intervention in patients with chronic conditions or at risk for such conditions.
- Patients can choose either a daily time-restricted feeding regimen (an 18-hour fasting period and a 6-hour eating period) or the 5:2 intermittent fasting regimen (fasting 2 days per week with an intake of 500 calories).
- There should be a 4-month transition period to accomplish the fasting goal.
- Physicians' staff should be in frequent contact with the patient during the 4-month period and closely monitor body weight, glucose, and ketone levels.
- Inpatient and outpatient facilities staffed by experts in diet, nutrition, exercise, and psychology can help patients make the transition to sustainable intermittent fasting and exercise regimens.
- Dietitians or nutritionists should be consulted to ensure nutritional needs are being met and to provide continued counseling and education

-
Clean eating
-
Q. What is Orthorexia nervosa ?
- Term Origin: Coined in 1997 by physician Steven Bratman, Orthorexia Nervosa (ON) describes an extreme preoccupation with "healthy" eating.
- Not Officially Recognized: It's not currently a diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
- Focus on Purity: The condition is characterized by an obsession with achieving dietary "purity," rather than weight loss.
-
Q. What is the suggested clinical criteria for Orthorexia nervosa ?
- Suggested criteria in defining ON include:
- Obsessional or pathological preoccupation with healthy nutrition
- Emotional consequences (e.g., distress, anxiety) of non-adherence to self-imposed nutritional rules
- Psychosocial impairments in relevant areas of life as well as malnutrition and weight loss
- Suggested criteria in defining ON include:
-
Q. What is the concept of 'clean eating' ?
- "Clean eating" is a popular but unregulated term generally interpreted as eating foods close to their natural state. It's especially popular among younger consumers and social media influencers.
- Surveys show a majority of people associate "clean eating" with unprocessed foods, organic produce, and simple ingredient lists.
- While many view it as a healthy lifestyle, a minority find it restrictive and even unhealthy.
- "Clean eating" can mask eating disorders like orthorexia nervosa (ON), a term describing an unhealthy obsession with "pure" foods.
- The Instagram effect: Frequent use of Instagram, popular among 18-34-year-olds, correlates with tendencies toward ON.
-
Gluten free diet for weight loss
-
Q. Is there any evidence for benefit of gluten free diet in people not having celiac disease ?
- There is no evidence to support that a gluten-free diet is effective for weight loss or offers general health benefits for those without celiac disease or gluten sensitivity.
- Key points:
- Popularity for Weight Loss: A gluten-free diet has gained attention for weight loss, despite being primarily for those with celiac disease or gluten sensitivity.
- Initial Weight Loss: Eliminating gluten-containing processed foods may lead to initial weight loss and a shift towards consuming naturally gluten-free whole foods.
- Lack of Research: There is no scientific evidence to support the effectiveness of a gluten-free diet for weight loss in people without celiac disease.
- Nutrient Deficiencies: A strict gluten-free diet can lead to inadequate intakes of essential nutrients like fiber, iron, and calcium.
- Potential Risks: Following a gluten-free diet may increase the risk of chronic diseases like heart disease and could actually lead to weight gain in some cases.
-
Ketogenic diet
-
Q. Which are the various named low carbohydrate diet ?
-
- Atkins diet
-
- Ketogenic diet
-
- Paleo diet
-
- South Beach diet
-
- Dunkan diet
-
-
Q. What is the difference between ketogenic diet and many of the other diets in the list ?
- Ketogenic diet has more fat content while the other diets tend to have more protein content
-
Q. How does a ketogenic diet work ?
- The ketogenic diet is a low-carbohydrate, high-fat eating plan.
- It aims to deprive the body of glucose, the main source of energy, and instead use ketones, which are produced from stored fat, as fuel.
- When carbohydrate intake is limited, the body first uses stored glucose from the liver and then breaks down muscle to release glucose.
- After a few days of low carbohydrate intake, blood levels of insulin decrease, and the body starts using fat as its primary fuel.
- The liver produces ketone bodies from fat, which can be used as an alternative to glucose.
- Ketosis occurs when ketone bodies accumulate in the blood.
- Ketosis is a natural state that can happen during fasting or intense exercise.
- The ketogenic diet aims to maintain a state of mild ketosis to promote weight loss and other health benefits.
- The diet typically consists of high-fat foods, moderate protein intake, and very low carbohydrate intake.
-
Q. What is the typical nutrient composition of a ketogenic diet ?
- The typical nutrient composition of a ketogenic diet is high in fat, moderate in protein, and low in carbohydrates.
- The diet typically reduces total carbohydrate intake to less than 50 grams a day, and can be as low as 20 grams a day.
- Popular ketogenic resources suggest an average of 70-80% fat from total daily calories, 5-10% carbohydrate, and 10-20% protein.
- For a 2000-calorie diet, this translates to about 165 grams fat, 40 grams carbohydrate, and 75 grams protein
-
Q. Why is the protein restricted in ketogenic diet ?
- Protein is restricted in the ketogenic diet to prevent excessive production of glucose.
- Consuming too much protein can prevent the body from entering ketosis.
- The amino acids in protein can be converted to glucose, which can hinder the process of using fat as the primary fuel source.
- Restricting protein helps to maintain a state of ketosis, where the body relies on ketones for energy instead of glucose.
-
Q. Do ketogenic diet have a high amount of saturated fat ?
- Yes
-
Q. Summarize the results of clinical studies done for ketogenic diet ?
-
Meta-Analysis of 13 Randomized Controlled Trials:
- Ketogenic diet led to small but significant reductions in weight, triglycerides, and blood pressure compared to low-fat diets.
- Greater increase in HDL and LDL cholesterol on the ketogenic diet.
- Compliance declined over time.
-
Systematic Review of 26 Short-Term Trials:
- Significant weight loss on both very low-calorie and ketogenic diets.
- Reduced hunger and desire to eat compared to baseline.
- Suggested further studies to explore the threshold of ketone levels needed to suppress appetite.
-
8-Week Study on 39 Obese Adults:
- Mean loss of 13% of starting weight.
- Significant reductions in fat mass, insulin levels, blood pressure, and waist and hip circumferences.
- Ghrelin levels did not increase, leading to decreased appetite.
-
12-Month Study on 89 Obese Adults:
- 10% weight loss with no weight regain at one year.
- 88% of participants were compliant with the diet regimen.
- The ketogenic diet used was lower in fat and slightly higher in carbs and protein than the average ketogenic diet.
- These studies generally show that the ketogenic diet has benefits for weight loss and metabolic health, but compliance and long-term effects need further study.
-
-
Q. What types of food are allowed and what are not allowed in ketogenic diet ?
-
Allowed Foods:
- High-Fat Focus: Cocoa butter, lard, poultry fat, plant fats (olive, palm, coconut oil), avocado, certain nuts and seeds.
- Limited Dairy: Butter and hard cheeses are allowed due to lower lactose content; cream, ice cream, and full-fat milk are restricted.
- Moderate Protein: Grass-fed beef, free-range poultry, pork, bacon, wild-caught fish, organ meats, eggs, tofu, certain nuts and seeds.
- Non-Starchy Vegetables: Leafy greens, cauliflower, broccoli, Brussels sprouts, asparagus, bell peppers, onions, garlic, mushrooms, cucumber, celery, summer squashes.
- Certain Fruits: Small portions of berries allowed due to lower "net carbs."
- Other: Dark chocolate (90% or higher cocoa), unsweetened coffee and tea, unsweetened vinegars and mustards, herbs, and spices.
-
Not Allowed Foods:
- Grains and Sugars: All whole and refined grains, added and natural sugars.
- Starchy Vegetables: Potatoes, corn, winter squash.
- Restricted Fruits: All fruits other than those on the allowed list; all fruit juices.
- Legumes: Beans, lentils, peanuts.
- Certain Alcohols: Most full carbohydrate wines and beers, drinks with added sweeteners are restricted; some programs allow small amounts of hard liquor or low-carb wines and beers.
-
-
Q. What are net carbs ?
-
Definition and Origin:
- Unregulated Terms: "Net carbs" and "impact carbs" are unregulated, interchangeable terms.
- Marketing Strategy: Invented by food manufacturers to claim lower "usable" carbs on labels.
-
Calculation:
- Directly Absorbed Carbs: Net carbs are carbs directly absorbed by the body and contribute calories.
- Subtraction Method: Calculated by subtracting indigestible carbs from total carbs.
- Indigestible Carbs: Include insoluble fibers and sugar alcohols like mannitol, sorbitol, and xylitol.
-
Controversies and Limitations:
- Inexact Science: Effect of sugar alcohols on absorption and blood sugar can vary.
- Caloric Impact: Some sugar alcohols may still contribute calories and affect blood sugar.
- Calorie Level: Total calorie count remains the same regardless of net carbs.
- Community Debate: Even within the ketogenic community, the value of using net carbs is debated.
-
-
Q. What are the potential side effects of ketogenic diet ?
- Hunger
- Fatigue
- Low mood
- Irritability
- Constipation
- Headaches
- Brain "fog"
- Increased risk of kidney stones
- Increased risk of osteoporosis
- Increased blood levels of uric acid (risk factor for gout)
- Possible nutrient deficiencies if a variety of recommended foods are not included
-
Q. What is the role of ketogenic diet in epilepsy ?
- Effective treatment for epilepsy: 38-60% of patients have a greater than 50% seizure reduction, and up to 30% achieve a greater than 90% seizure reduction.
- Valid treatment option for patients who have failed at least two antiseizure medications.
- May be particularly effective for patients with certain types of epilepsy, such as Doose syndrome, Dravet syndrome, glucose transporter 1 (GLUT-1) deficiency, infantile spasms, pyruvate dehydrogenase deficiency, and tuberous sclerosis complex.
- Should be supervised by a trained dietitian and neurologist in an epilepsy center with expertise in this form of therapy.
- Important adverse effects of KDT include gastrointestinal symptoms, dyslipidemia, hypoglycemia, constipation, growth failure, bone disease, and kidney stones.
- Efficacy of the diet is usually apparent in the first one to three months.
- KDT is generally recommended for a minimum of three months and maximum of two years; however, longer periods of effective use have been described.
-
Q. What is the role of ketogenic diet in epilepsy ?
- Efficacy of KDT in Epilepsy: Ketogenic Dietary Therapy (KDT) is effective in treating epilepsy, with 38-60% of patients experiencing over a 50% seizure reduction.
- Indications for KDT: It is a valid treatment especially for those who have failed at least two antiseizure medications and is particularly effective for specific syndromes and drug-resistant epilepsy.
- Pre-treatment Counseling: Patients and caregivers should be educated about the diet's implications on seizure control, medication use, and psychosocial factors. Screening for contraindications is important.
- Types of KDT: Multiple diets available, such as classic ketogenic, medium-chain triglyceride, modified Atkins, and low glycemic index treatment. Diet choice should be individualized. Supplements are often necessary.
- Supervision: Diet should be managed by a trained dietitian and neurologist. Initial diet often started in a hospital setting; outpatient approaches also available.
- Monitoring and Follow-Up: Regular clinical and laboratory assessments are required to adjust KDT and/or medications and to monitor for adverse effects like gastrointestinal issues and kidney stones.
- Timeline for Efficacy: Positive results usually seen in the first one to three months. If effective, antiseizure medications may be tapered.
- Duration and Discontinuation: Typically recommended for 3 months to 2 years, but can be extended. Tapering is advised unless severe adverse effects occur.
-
Q. What does the American diabetes association say with regards to ketogenic diet ?
- Ketogenic Diet for Type 2 Diabetes: The ADA says it may be an option for those not meeting glycemic targets or wanting to reduce glucose-lowering drugs but should be supervised by healthcare professionals.
- Caution for Type 1 Diabetes: People with type 1 diabetes should consult their doctor before trying a ketogenic diet due to the risk of diabetic ketoacidosis (DKA).
- Not Suitable for All: Ketogenic diets are not recommended for pregnant or breastfeeding women, those with kidney disease, eating disorders, or taking specific medications like SGLT2 inhibitors.
- Consult Healthcare Professional: The ADA emphasizes the need to consult with a qualified healthcare professional before starting a ketogenic diet, especially for those with underlying health conditions.
- Evolving Research: The ADA's guidelines are based on current scientific evidence, which is still evolving, and may change in the future as more research becomes available
-
Q. What is the bottom line with regards to ketogenic diet ?
- The ketogenic diet is a low-carbohydrate, high-fat eating plan.
- It has been used for centuries to treat specific medical conditions.
- It has been found to have benefits on a short term, but long term issues are not well known
- The diet promotes weight loss and can improve health parameters associated with excess weight.
- Compliance may be difficult due to the elimination of certain food groups and potential side effects.
- The diet may have adverse effects on blood LDL cholesterol due to its emphasis on saturated fat.
- It is important to consult with a physician and dietitian before starting a ketogenic diet.
- The exact ratio of fat, carbohydrate, and protein needed for health benefits may vary among individuals.
- A modified carbohydrate diet following the Healthy Eating Plate model may also produce health benefits and weight reduction.
- Long-term effects and safety issues of the ketogenic diet are still not well understood.
-
Other points
-
Q. What is the relationship between dairy consumption and cardiovascular health ?
- According to a recent meta-analysis published in Advances in nutrition dairy consumption is generally associated with a lower risk of cardiovascular issues like hypertension (HTN), coronary heart disease (CHD), and stroke.
- Specific Findings:
- Lower risk of HTN with higher dairy intake (RR: 0.91 for highest vs lowest intake).
- Lower risk of CHD with higher dairy intake (RR: 0.96 for highest vs lowest intake).
- Lower risk of stroke with higher dairy intake (RR: 0.90 for highest vs lowest intake).
- Quality of Evidence:
- Moderate quality for the relationship with HTN and CHD.
- Low quality for the relationship with stroke.
- Variability:
- Moderate to considerable heterogeneity in study estimates.
- Types of Dairy:
- Low-fat dairy associated with lower risk of HTN and stroke.
- High-fat dairy associated with lower risk of stroke.
- Conclusion: Dairy consumption, especially low-fat dairy, is associated with a modestly lower risk of cardiovascular issues, although the quality of evidence varies
-
Paleo diet
-
Q. What is the concept of a paleo diet ?
- Origins: Based on the eating habits of humans during the Paleolithic era, which dates back over 2 million years ago.
- Genetic Rationale: Proponents believe that since our genetics and anatomy have changed little since the Stone Age, we should consume foods available during that time for optimal health.
- Food Sources: Early humans relied on hunting, fishing, and gathering wild plants for sustenance, as they lacked advanced tools for farming.
- Diet Composition: Emphasizes lean meats, fish, fruits, vegetables, nuts, and seeds.
- Exclusions: Avoids processed foods, whole grains, dairy products, legumes, and refined sugars.
- Low-Glycemic Focus: Encourages the consumption of low-glycemic fruits and vegetables.
- Debate: There's ongoing debate about the exact foods available during the Paleolithic era and thus what should be included or excluded in the diet.
- Health Claims: Believed to reduce the risk of modern-day diseases like diabetes, cancer, and heart disease due to its natural and unprocessed food focus.
-
Q. What foods are allowed or not allowed in paleo diet ?
- Allowed Foods:
- Lean Meats: Such as chicken, turkey, and beef.
- Fish and Shellfish: Especially those rich in omega-3 fatty acids like salmon and mackerel.
- Eggs: Preferably from free-range or pasture-raised chickens.
- Fruits: All kinds, but low-glycemic fruits are emphasized.
- Vegetables: Almost all, with a focus on non-starchy varieties.
- Nuts and Seeds: Such as almonds, walnuts, and flaxseeds.
- Healthy Oils: Derived from fruits and nuts like olive oil and coconut oil.
- Certain Root Vegetables: Sweet potatoes and cassava may be allowed in moderation due to their nutrient content.
- Natural Sweeteners: Limited amounts of honey.
- Not Allowed Foods:
- Whole Grains: Such as wheat, oats, and barley.
- Cereals: Both refined and whole grain varieties.
- Refined Grains and Sugars: Like white bread and table sugar.
- Dairy Products: Including milk, cheese, and yogurt.
- White Potatoes: Due to their high glycemic index.
- Legumes: Such as peanuts, beans, and lentils.
- Alcohol: Especially in processed forms.
- Coffee: Some versions of the Paleo diet exclude it.
- Salt: Especially in high amounts.
- Refined Vegetable Oils: Such as canola oil.
- Most Processed Foods: Anything with artificial additives, preservatives, or other chemicals.
- Allowed Foods:
-
Q. Which natural food has highest amount of omega 3 fatty acid ?
- Salmon fish
- It has 1000-2000 mg of EPA/DHA per 3 ounce portion
-
Q. What is the typical nutrition breakdown of paleo diet ?
- Protein: High intake, primarily from lean meats, fish, and eggs.
- Fats: Moderate intake, mainly from:
- Unsaturated Fats: Including monounsaturated and polyunsaturated fats.
- Omega-3 Fats: Especially EPA and DHA, sourced from marine fish, nuts, seeds, and certain oils.
- Grass-Fed Beef: Highlighted for its slightly higher omega-3 content compared to grain-fed beef.
- Carbohydrates: Low to moderate intake, with a focus on:
- Low-Glycemic Index: Emphasizing fruits and vegetables that have a slower impact on blood sugar levels.
- Restriction: High glycemic index carbohydrates are typically restricted.
- Fiber: High intake, sourced mainly from fruits, vegetables, nuts, and seeds.
- Sodium: Low intake, as processed foods and added salts are generally avoided.
- Refined Sugars: Minimal to none, as the diet emphasizes natural foods and sweeteners.
- Overall Nutrient Focus: The diet aims for nutrient-dense whole fresh foods and avoids highly processed foods containing added salt, sugar, and unhealthy fats.
-
Q. What is the clinical evidence with regards to paleo diet ?
- Short-Term Benefits: Some randomized controlled trials have shown that the Paleo diet can offer short-term benefits over diets based on national nutrition guidelines. These benefits include:
- Greater weight loss.
- Reduced waist circumference.
- Decreased blood pressure.
- Increased insulin sensitivity.
- Improved cholesterol levels.
- Study Duration and Size: The aforementioned studies were typically of short duration (6 months or less) and involved a small number of participants (less than 40).
- Long-Term Study: One larger randomized controlled trial followed 70 post-menopausal Swedish women with obesity for two years. They were placed on either a Paleo diet or a Nordic Nutrition Recommendations (NNR) diet. Results showed:
- Both groups saw significant decreases in fat mass and waist circumference at 6 and 24 months.
- The Paleo diet resulted in greater fat loss at 6 months but not at 24 months.
- Triglyceride levels decreased more with the Paleo diet at both 6 and 24 months compared to the NNR diet.
- Potential Pitfalls: The restrictive nature of the Paleo diet and the exclusion of certain food groups might lead to nutrient deficiencies and other health concerns, especially when followed long-term.
- Need for More Research: While some studies show benefits of the Paleo diet, more high-quality, long-term research is needed to determine its direct health benefits and potential risks.
- Conclusion: Strong recommendations for the Paleo diet for weight loss cannot be made at this time based on the available evidence.
- Short-Term Benefits: Some randomized controlled trials have shown that the Paleo diet can offer short-term benefits over diets based on national nutrition guidelines. These benefits include:
-
Q. What are important pitfalls with this diet ?
- Higher red meat consumption may be problematic
- All micronutrients may not be adequatley supplemented
- this is especially a problem with dietary calcium requirement
-
Mindful eating
-
Q. What is mindfulness ?
- Origin: Mindfulness has roots in many religions and has been practiced for centuries.
- Definition: It is an intentional focus on one's thoughts, emotions, and physical sensations in the present moment.
- Purpose: Mindfulness aims to increase awareness rather than reacting impulsively to one's situation and choices.
- Application: It can be applied in various aspects of life, including eating, meditation, and daily activities.
- Benefits: Mindfulness promotes a deeper understanding of oneself, enhances the overall experience of activities, and can improve mental well-being.
- Non-Judgmental: One of the key principles of mindfulness is to observe thoughts and feelings without judgment, allowing for a more objective understanding of oneself.
-
Q. What is mindful eating ?
- Origin: Derives from the broader philosophy of mindfulness, emphasizing presence and awareness.
- Definition: Eating mindfully involves using all physical and emotional senses to experience, savor, and enjoy food choices.
- Intentional Focus: Emphasizes heightened awareness of eating experiences, body-related sensations, and thoughts and feelings about food.
- Non-Judgmental: Encourages satisfying and nourishing food choices without "judging" or criticizing one's eating behaviors.
- Holistic Experience: Considers the broader spectrum of the meal, including its origin, preparation, and the people involved in its creation.
- Sensory Engagement: Engages all senses, noting the appearance, smell, texture, and taste of food.
- Pace: Encourages eating slowly, savoring each bite, and chewing thoroughly to enhance digestion and satisfaction.
- Cues: Involves noticing internal cues (like hunger and fullness) and external cues that might affect consumption.
- Gratitude: Expressing appreciation for the meal, acknowledging its source, and reflecting on its impact on health and the environment.
- Benefits: Can lead to better diet quality, reduced overeating, improved psychological well-being, and increased eating pleasure.
- Application: Can be practiced by anyone, regardless of dietary preferences or restrictions, and complements any eating pattern.
-
Q. What are the 4 principles of mindful eating ?
- What we eat ?
- Why we eat, what we eat ?
- How much to eat ?
- How to eat ?
-
Q. What are the seven principles of mindful eating ?
- Honor the Food: Acknowledge its source and the effort involved in its preparation.
- Engage All Senses: Experience the food with sight, smell, touch, taste, and hearing.
- Serve in Modest Portions: Be mindful of portion sizes to avoid overconsumption.
- Savor Small Bites: Take time to chew thoroughly and truly taste the food.
- Eat Slowly: This helps in recognizing fullness cues and enhances the enjoyment of the meal.
- Don't Skip Meals: Ensure regular and balanced food intake.
- Prioritize a Plant-Based Diet: Emphasize plant foods for health and environmental reasons.
-
Q. What are the clinical benefits with regards to mindful eating ?
- Mindless Eating Issues: Mindless or distracted eating has been linked to anxiety, overeating, and weight gain.
- Strategy for Improved Eating: Mindful eating has been explored as a potential strategy to address and improve eating behaviors.
- Emotional and Binge Eating: Studies have shown that mindfulness practices can help reduce emotional and binge eating tendencies.
- Weight Loss: While mindful eating has shown benefits in eating behaviors, consistent weight loss isn't always a direct outcome.
- Diet Quality: Mindful eating practices can lead to better diet quality, such as making healthier food choices like opting for fruits over sweets.
- Research Limitations: More research is needed to standardize the approach of mindful eating and to determine its long-term impact on health and well-being.?
-
Q. What is the bottom line with regards to mindful eating ?
- Mindful eating can complement any eating pattern and has shown benefits like psychological well-being, increased eating pleasure, and body satisfaction.
- Combining mindfulness with nutrition knowledge can lead to healthier food choices and a better body image.
-
References:
-
- Mazzocchi, A., Leone, L., Agostoni, C., & Pali-Schöll, I. (2019). The Secrets of the Mediterranean Diet. Does [Only] Olive Oil Matter? Nutrients, 11(12). https://doi.org/10.3390/nu11122941
-
- Barnes LL, Dhana K, Liu X, Carey VJ, Ventrelle J, Johnson K, Hollings CS, Bishop L, Laranjo N, Stubbs BJ, Reilly X. Trial of the MIND Diet for Prevention of Cognitive Decline in Older Persons. New England Journal of Medicine. 2023 Aug 17;389(7):602-11.
-
- Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, Lamuela-Raventos RM. Primary prevention of cardiovascular disease with a Mediterranean diet. New England Journal of Medicine. 2013 Apr 4;368(14):1279-90.
-
- Diet reviews : Harvard School of public health - https://www.hsph.harvard.edu/nutritionsource/healthy-weight/diet-reviews/
-
- Borgundvaag E, Mak J, Kramer CK. Metabolic impact of intermittent fasting in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of interventional studies. The Journal of Clinical Endocrinology & Metabolism. 2021 Mar 1;106(3):902-11.
-
- Liu D, Huang Y, Huang C, Yang S, Wei X, Zhang P, Guo D, Lin J, Xu B, Li C, He H. Calorie restriction with or without time-restricted eating in weight loss. New England Journal of Medicine. 2022 Apr 21;386(16):1495-504.
-
- Chen Z, Ahmed M, Ha V, Jefferson K, Malik V, Ribeiro PA, Zuchinali P, Drouin-Chartier JP. Dairy product consumption and cardiovascular health: a systematic review and meta-analysis of prospective cohort studies. Advances in Nutrition. 2022 Mar;13(2):439-54.
-