Credits
Section Writer: Dr. Om J Lakhani
Section Editor: Dr. Om J Lakhani
Support us:
-
Premium Membership- Download PDF version of Notes, Get ad free video and more
-
Consultant Membership- Above plus Download Powerpoint presentation of the notes
- Support us by purchasing our book - Click here for more details:
- Q. Broadly what are the two causes of hypokalemia?
-
- Entry of potassium into the cells- redistributive hypokalemia
-
- Loss of potassium from the body - GI or renal loss
-
- Q. True or false- potassium replacement in redistributive hypokalemia is done cautiously?
- Yes
- Because it is often transient and can lead to rebound hyperkalemia
- Q. When do symptoms of hypokalemia generally appear?
- When the potassium level is <3.0 meq/l
- Q. When does muscle weakness start appearing?
- Muscle weakness appears when the potassium is <2.5 meq/l
- Q. How does hypokalemia produce muscle weakness?
- Impaired muscle contraction: A decrease in extracellular potassium concentration hyperpolarizes muscle cell membranes, making them more negatively charged and impairing their ability to depolarize and contract, leading to weakness.
- Potassium's role in blood flow: Normally, potassium release from muscle cells during exercise aids in vasodilation and increases muscle blood flow. Profound hypokalemia reduces this potassium release, diminishing blood flow to muscles during exertion, which can contribute to muscle weakness and even ischemic rhabdomyolysis.
- Q. Is the impact of the above reversible?
- Yes
- It reverses with potassium correction
- Q. What is the impact of hypokalemia on the GI tract?]
- It can similarly impact GI muscles leading to paralytic ileus
- Q. What is Ogilves's syndrome?
- Ogilvie's syndrome, also known as acute colonic pseudo-obstruction, is associated with hypokalemia due to the following factors:
- Involvement of gastrointestinal muscles: Hypokalemia can cause muscle dysfunction, including in the gastrointestinal tract, leading to symptoms like ileus.
- Distension, anorexia, nausea, and vomiting: These symptoms are associated with gastrointestinal muscle involvement due to hypokalemia.
- Association with secretory diarrhea: Some patients with Ogilvie's syndrome and hypokalemia experience secretory diarrhea, characterized by an abnormally high fecal potassium content. This can exacerbate the condition and contribute to the complexity of managing electrolyte imbalances.
- Ogilvie's syndrome, also known as acute colonic pseudo-obstruction, is associated with hypokalemia due to the following factors:
- Q. What are the ECG changes that we expect in patients with hypokalemia?
- The ECG changes observed in patients with hypokalemia include:
- Flattening of the T wave: This is often the earliest electrocardiographic sign of hypokalemia.
- Prominent U waves: As hypokalemia progresses, U waves become more prominent, particularly in the precordial leads.
- ST-segment depression: This may be observed as potassium levels continue to decrease.
- Appearance of a U wave that is taller than the T wave: In severe cases of hypokalemia, the U wave can become taller than the T wave, which is a more pronounced sign of the condition.
- Prolongation of the PR interval and widening of the QRS complex: These changes are less common but can occur with severe hypokalemia.
- The ECG changes observed in patients with hypokalemia include:
- Q. What kind of arrhythmias can be precipitated by hypokalemia]]?
- Hypokalemia can precipitate several types of arrhythmias, including:
- Ventricular fibrillation: A severe form of cardiac rhythm disturbance that can be fatal if not immediately treated.
- Ventricular tachycardia: A fast, abnormal heart rate that originates in the lower chambers of the heart (the ventricles).
- Atrial fibrillation: A common type of arrhythmia that causes an irregular and often rapid heart rate.
- Atrial tachycardia: A type of heart rhythm problem characterized by a faster-than-normal heart rate originating in the atria.
- Premature ventricular contractions (PVCs): Extra, abnormal heartbeats that begin in the ventricles.
- Torsades de pointes: A specific type of ventricular tachycardia that can lead to sudden cardiac death if not promptly treated.
- Hypokalemia can precipitate several types of arrhythmias, including:
- Q. At what potassium levels do arrhythmia typically occur?
- Potassium <3.0 meq/l
- Q. Which are the factors that increase the risk of arrhythmia due to hypokalemia?
- The factors that increase the risk of arrhythmia due to hypokalemia include:
- Concomitant use of digitalis: The use of digitalis drugs increases the risk of arrhythmias in the setting of hypokalemia.
- Presence of heart disease: Patients with underlying heart disease like coronary ischemia are at higher risk for developing arrhythmias when they have hypokalemia.
- Concurrent hypomagnesemia: Low magnesium levels, along with low potassium levels, can exacerbate the risk of arrhythmias.
- Use of diuretics: Diuretics that increase potassium loss through urine can significantly increase the risk of hypokalemia-induced arrhythmias.
- The factors that increase the risk of arrhythmia due to hypokalemia include:
- Q. What are the renal abnormalities that can be seen with hypokalemia?
- Impaired urine concentration: Hypokalemia can lead to difficulties in the kidney's ability to concentrate urine, potentially causing polyuria and contributing to dehydration.
- Increased ammonia production: The kidney may produce more ammonia in response to hypokalemia, which can contribute to metabolic alkalosis by enhancing the reabsorption of bicarbonate.
- Interference with renal blood flow: Hypokalemia can affect kidney function by altering renal blood flow, potentially leading to reduced glomerular filtration rate (GFR).
- Structural damage to the kidneys: Chronic hypokalemia can cause histological changes in the kidneys, including vacuolization of the tubular epithelium, which may lead to chronic kidney disease if not addressed. This is also called Hypokalemic nephropathy
- Q. What are the endocrine abnormalities seen with hypokalemia?
-
- Reduced insulin secretion:
- This is an important etiology of thiazide-induced glucose intolerance
-
- Nephrogenic Diabetes insipidus]]
-
- Q. Which patients of hypokalemia require continuous ECG monitoring?'
- Significantly low potassium levels: Individuals presenting with markedly low serum potassium levels (<2.5) are at increased risk for cardiac arrhythmias, making continuous ECG monitoring essential to detect and manage potential life-threatening cardiac events promptly.
- Symptoms of cardiac involvement: Patients exhibiting symptoms such as palpitations, chest pain, or syncope should be closely monitored with continuous ECG to promptly identify arrhythmias or other cardiac abnormalities that may arise due to hypokalemia.
- Existing heart disease: Those with underlying heart conditions, such as coronary artery disease, heart failure, or a history of arrhythmias, are more susceptible to the cardiac effects of hypokalemia. Continuous ECG monitoring in these patients helps in the early detection and management of arrhythmias that hypokalemia may exacerbate.
- Concomitant use of medications that affect cardiac rhythm: Patients on medications known to influence cardiac rhythm or predispose to arrhythmias, such as digoxin or certain diuretics, benefit from continuous ECG monitoring due to an increased risk of arrhythmias under the influence of hypokalemia.
- Undergoing aggressive potassium repletion: Continuous ECG monitoring is also warranted in patients receiving aggressive treatment for hypokalemia, especially if intravenous potassium is administered. This is because rapid changes in potassium levels can precipitate cardiac arrhythmias, necessitating close monitoring of the heart's electrical activity to ensure patient safety.
- Q. Can hypokalemia be corrected with potassium replacement for a few hours?
- No
- Remember potassium is mainly intracellular
- Hence hypokalemia reflects a mere reduction in extracellular potassium
- But patients with hypokalemia will have total body potassium deficit which needs to be corrected
- This correction may require replacement for often days
- Q. Why is hypomagnesemia important in patients with hypokalemia?
-
- Hypomagnesemia is caused by the same process as often as hypokalemia and both often coexist
-
- The existence of both together increases the Arrhythmogenic potential
-
- Correction of Hypokalemia is refractory without correction of Hypomagnesemia
-
- Q. Why is it important to closely monitor the potassium and ECG monitoring is a must in case of redistributive hypokalemia?
- Redistributive hypokalemia is because of potassium moving inside the cells
- Once this is corrected- it can lead to rebound hyperkalemia which can even cause arrhythmia
- The rebound hyperkalemia is NOT uncommon and occurs in 40-60% of cases
- This is especially common in patients with hypokalemic and thyrotoxic periodic paralysis
- Q. What are the causes of redistributive hypokalemia?
- The causes of redistributive hypokalemia include:
- Increased beta-adrenergic activity: Conditions that lead to elevated levels of catecholamines can cause potassium to move from the extracellular to the intracellular space, lowering serum potassium levels without actual total body potassium loss.
- Insulin administration: Insulin promotes the cellular uptake of glucose and potassium, which can lead to a transient decrease in serum potassium levels as potassium shifts into cells.
- Alkalosis: Both respiratory and metabolic alkalosis can cause potassium to move intracellularly in exchange for hydrogen ions, leading to a decrease in serum potassium levels.
- Hypothermia: Reduced body temperature can lead to a redistribution of potassium into cells, lowering serum potassium levels.
- Familial periodic paralysis: This rare genetic disorder can cause episodes of muscle weakness associated with shifts of potassium into cells, leading to hypokalemia during attacks.
- The causes of redistributive hypokalemia include:
- Q. If Increased beta-adrenergic activity or theophylline toxicity is thought to be the cause of redistributive hypokalemia, what is the best course of treatment?
- The best course of treatment in such cases is using a non-specific beta-blocker
- This corrects the problem without causing rebound hyperkalemia
- Q. Based on this concept, 1 meq/l of drop in serum potassium is equal to what total body potassium loss?
- 1 meq/l of potassium is associated with 200-400 meq/l of total body potassium loss
- Q. Give a ballpark figure of total body potassium deficit based on the serum potassium levels.
-
- Serum potassium 3.0 meq/l- 100-200 meq/l of deficit
-
- Serum Potassium 2.0 meq/l- 400-600 meq/l of deficiet
-
- Serum potassium <2.0 meq/l- >600 meq/l of deficit
-
- Q. A patient has Diabetic ketoacidosis]] with serum potassium of 4.2 meq/l. He is to be started on an insulin infusion. Is potassium replacement required?
- Yes
- In Diabetic ketoacidosis]] there is a flux of potassium outside of the cells
- These lead to normal potassium levels but there is a net deficit of total body potassium further exacerbated by GI and renal losses of potassium
- Hence a potassium level of 4.5 is reflectively of an existing potassium deficit which will be further worsened by insulin therapy
- Hence potassium replacement is required
- In all patients with Diabetic ketoacidosis]] a potassium replacement is a must up to a serum potassium of 5.2 meq/l
- Here the rate of replacement when the potassium is between 3.3-5.2 meq/l should be 20-30 meq/hour
- Q. In which cases should insulin therapy be delayed?
- Insulin therapy should be delayed if the initial potassium in Diabetic ketoacidosis]] is <3.3 meq/l
- Here the rate of potassium replacement should be 40-60 meq/hr
- Q. What are the various potassium preparations?
- The various potassium preparations available for treating hypokalemia include:
- Potassium chloride: This is the most common form used for supplementation, available in oral and intravenous formulations. It is used to treat or prevent low blood levels of potassium (hypokalemia).
- Potassium phosphate: Primarily used when there is a concurrent need to treat or prevent low levels of phosphate (hypophosphatemia) along with hypokalemia.
- Potassium bicarbonate: Used in cases where there is also a need to correct metabolic acidosis, as it provides bicarbonate to help buffer the acid-base balance in the blood.
- Potassium acetate: Sometimes used in intravenous formulations to provide potassium while also acting as a source of bicarbonate after metabolism.
- Potassium gluconate: Often found in oral supplements, it is considered a more gentle option for those who might experience gastrointestinal discomfort from potassium chloride.
- The various potassium preparations available for treating hypokalemia include:
- Q. Which potassium preparation would you use based on the acid-base equation?
- Hypokalemia with acidosis (eg: Renal tubular acidosis)- Prefer potassium bicarbonate or potassium acetate
- Hypokalemia with alkalosis (vomiting, diuretic therapy)- potassium chloride
- Q. Explain why potassium chloride is preferred in hypokalemia with metabolic alkalosis.
- Excess vomiting → Chloride depletion → Enhances renal bicarbonate reabsorption from kidney → Worsens alkalosis → in this situation body tries to conserve sodium in exchange for potassium → worsens hypokalemia
- Hence in the situation of alkalosis if chloride is not given with potassium, only 40% of potassium is retained
- Hence in conditions of alkalosis - potassium chloride corrects hypokalemia faster than potassium bicarbonate
- Q. Which are the various forms in which potassium chloride is available and can be given?
- Potassium chloride is available and can be given in various forms, including:
- Oral tablets: These are available in both immediate-release and extended-release formulations, allowing for flexibility in dosing and patient compliance.
- Oral liquid solution: This form is useful for patients who have difficulty swallowing tablets or capsules and allows for precise dosing adjustments.
- Powder for oral solution: Potassium chloride powder can be mixed with water to create a solution, offering another alternative for those who prefer not to take pills or have specific dosing requirements.
- Intravenous (IV) solution: For patients with severe hypokalemia or those who cannot take oral medications, potassium chloride can be administered intravenously. This method allows for rapid correction of potassium levels under closely monitored conditions.
- Effervescent tablets: These are dissolved in water before ingestion, providing an alternative oral form that may be more palatable for some patients.
- Potassium chloride is available and can be given in various forms, including:
- Q. What is the problem with extended-release or slow-release tablets?
- They can lead to local ulceration
- However, encapsulated preparations are better in these regards
- Q. Is giving potassium-rich food truly helpful in correcting hypokalemia?
- potassium-containing foods and fruits are less effective in correcting hypokalemia
- this is because they mainly contain potassium in the form of phosphate or citrate
- As discussed earlier, in case of associated alkalosis- citrate or bicarbonate preparations are ineffective in correcting hypokalemia
- the potassium content in fruits is too low - eg: one banana has only 2.2 meq/inch of potassium which means to provide just 40 meq of potassium you would need to take 2-3 bananas
- Q. How is the prolonged release of potassium chloride available in India?
- POTRIDE tablet

- ADDKAY Tablet
- Q. Is potassium citrate available in Oral form?
- Yes
- potassium magnesium citrate is widely available as a POTRATE MB6 tablet
- Q. Is the management of hypokalemia in acute and chronic conditions different?
- Yes
- In acute conditions, the ongoing losses need to be matched plus additional potassium is required to increase the serum potassium levels
- In chronic hypokalemia conditions like Primary aldosteronism, the chronic loss is in a state of balance- in such cases potassium-sparing diuretics are very useful
- Q. Which are the two classes of potassium-sparing diuretics?
-
- Those acting on collecting duct- Amiloride & Triamterene
-
- Those acting on the aldosterone pathway - Spironolactone and Eplerenone
-
- Q. Which of these is preferred in which condition?
- In most cases of renal conditions producing hypokalemia other than primary aldosteronism- amiloride is preferred
- In other cases, Spironolactone is preferred
- Q. In which patients with heart failure should spironolactone not be initiated initially?
- Those with baseline potassium >5.0
- Those with creatinine
- More than 2.5 mg/dl in men
- More than 2.0 mg/dl in women
- Q. Does mild to moderate hypokalemia produce symptoms?
- Mild to moderate hypokalemia is defined as potassium or 3.0-3.4 meq/l
- These levels do not produce symptoms generally
- Patients with heart failure or liver disease may have symptoms at this level of potassium
- Q. How do you treat mild to moderate hypokalemia?
- If potassium loss is due to Gastrointestinal losses then this is generally treated with oral medications
- Potassium chloride - if the patient has alkalosis or normal pH
- Potassium bicarbonate- if patient has acidosis
- The dose is 10-20 meq/l three to 4 times a day
- If the potassium loss is due to renal loss
- Without primary aldosteronism- Amiloride
- With primary aldosteronism- Spironolactone
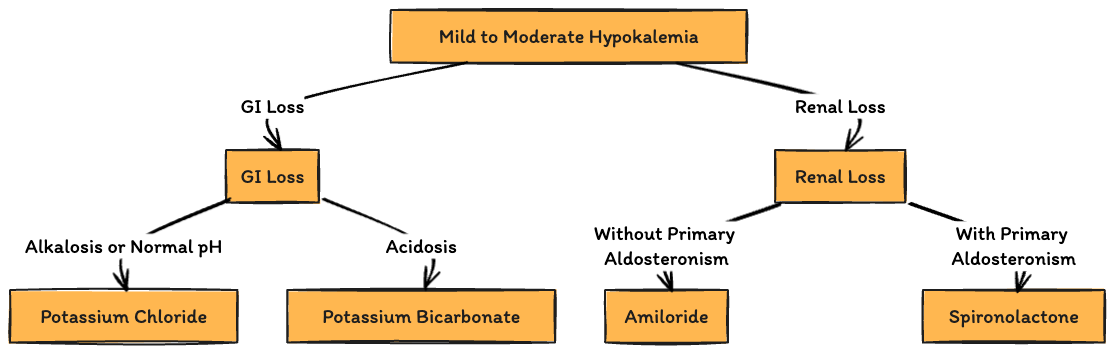
- If potassium loss is due to Gastrointestinal losses then this is generally treated with oral medications
- Q. ADDKAY tablet is 750 mg - how much potassium does this provide in meq/l?
- 750 mg tablet contains 10 meq/l of potassium
- Hence the dose is ADDKAY tablet 750 mg three times a day
- Q. What is the common side effect of the above?
- It can produce ulceration
- Q. What instructions do we give to the patients when we prescribe this tablet?
- Inform patients to take each dose with meals and with a full glass of water or other liquid, and to not crush, chew, or suck the tablets.
- Advise patients to seek medical attention if tarry stools or other evidence of gastrointestinal bleeding is noticed.
- Inform patients that the wax tablet is not absorbed and may be excreted intact in the stool. If the patient observes this, it is not an indication of lack of effect.
- Q. How much potassium citrate is contained in 1 tablet of Potrate MB6?
- 1 tablet contains about 700mg of potassium citrate which is around 7 meq of potassium
- Hence again 3-4 tablets per day would be needed
- Q. Which patients require more rapid correction of hypokalemia?
-
- Those with Hypokalemia with potassium of 2.5-3.0 meq/l
-
- Those symptomatic for hypokalemia
- Arrhythmias
- Marked muscle weakness
- Rhabdomyolysis
-
- Q. What are the issues with Rhabdomyolysis?
- Hypokalemia can itself lead to Rhabdomyolysis
- However, with Rhabdomyolysis, potassium is released in the extracellular system- leading to an increase in serum potassium and even transient hyperkalemia
- Q. How much potassium level increase with 40-60 meq/l of potassium supplement?
- it would depend on the method of replacement and ongoing loss
- However, 40-60 meq/l of potassium replacement can increase the serum potassium by 1-1.5 meq/l but often transiently
- The levels often fall after some time because the potassium gets taken up by cells or lost due to the underlying disease
- Q. How frequently would you monitor the potassium levels in patients undergoing replacement with severe or symptomatic hypokalemia?
- ideally, 4-6 hours till the levels become stable
- Q. What amount of potassium can be given via the peripheral IV line and what potassium level has to be given via the central line?
- Peripheral line
- Upto 40 meq/l of concentration
- Rate of <20 meq/hr
- Central line
- More than 40 meq/l of concentration
- More than 20 meq/hr of the rate of infusion
- Peripheral line
- Q. What is the typical rate of IV potassium administration based on potassium levels?
- Serum potassium of 2.5-2.9 meq/l- Give 10-20 meq/hr of serum potassium via peripheral line
- Serum potassium of <2.5 meq/l - Give 20-40 meq/hr for serum potassium via central line
- Q. What are suggested dilutions for the potassium?
- In 1-litre non-dextrose containing IV bags- add a maximum of 60 meq of KCl
- In small 100-200 ml mini bags-give maximum of 10 meq of potassium via peripheral line
- In small 100-200 ml mini bags-if up to 40 meq needs to be given- give via central line
- Q. Can you give an outline for KCl infusion via peripheral line in moderate hypokalemia?
- 3 x 10 ml Ampules of 10% KCl (40 meq total) in 1 liter of normal saline over 4 hrs via peripheral line
- This delivers 10 meq/hour, with a concentration of 40 meq/l

- Ref: https://medicalguidelines.msf.org/en/viewport/CHOL/english/appendix-8-administration-of-iv-potassium-kcl-25297281.html#section-target-2
- Q. Can you give an outline for KCl infusion via a central line in severe hypokalemia?
- 5 x 10 ml Ampules of 10% KCl (60 meq total) in 1 liter of normal saline over 6 hrs via central line
- Q. When giving potassium to Diabetic ketoacidosis]] patients in normal saline, what care must be taken?
- We often add 40-60 meq of KCl to 1 liter of saline
- This can make the normal saline hyperosmolar
- Hence it is better to add to half normal saline
- Q. What kind of fluid should generally be used to give KCl in nondiabetic situations?
- Prefer Normal saline in such cases- Dextrose-containing solutions can stimulate insulin which in itself can produce hypokalemia