-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
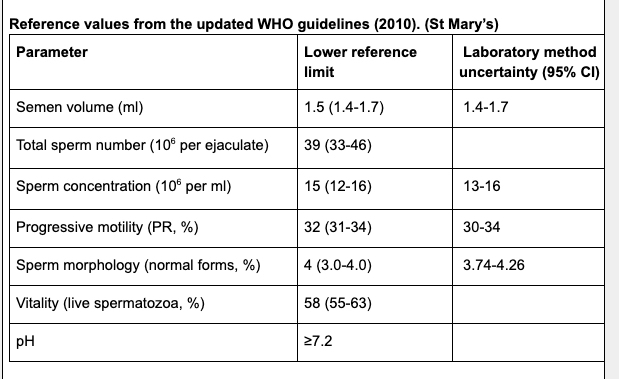
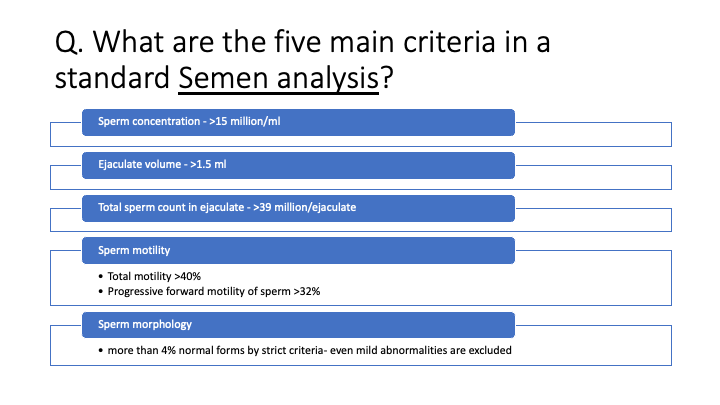
Q. What are the five main criteria in a standard Semen analysis?
- Sperm concentration - >15 million/ml
- Ejaculate volume - >1.5 ml
- Total sperm count in ejaculate - >39 million/ejaculate
- Sperm motility
- Total motility >40%
- Progressive forward motility of sperm >32%
- Sperm morphology
- more than 4% normal forms by strict criteria- even mild abnormalities are excluded
-
Q. What are some other essential criteria?
- Peroxidase positive leukocytes ( million/ml) - less than 1
- Immunobead test ( motile spermatozoa with bound beads %) - less than 50.
- Seminal zinc ( micromol/ejaculate) - more or equal to 2.4
- Seminal fructose (micromol/ejaculate) - More than 13
- Seminal neutral glucosidase ( mU/ejaculate) - more than 20.
-
Q. What are the factors pre-analytical that impact a semen analysis?
-
- Period of abstinence
-
- Any recent illness (lowers sperm quality)
-
- Use of any exogenous drugs like testosterone or glucocorticoids
-
- Delay in assessment after collection of sample
-
- Transportation of sample
-
- Method and completeness of the collection
-
-
Q. What is an ideal period of abstinence before collection of a sample for semen analysis?
- The absence period should be at least 2 days but not more than 7 days
-
Q. How is the sample for semen analysis generated?
- It is generated by masturbation
-
Q. How is the sample transported?
- It should be kept at 20-37 degree C at the time of transportation
-
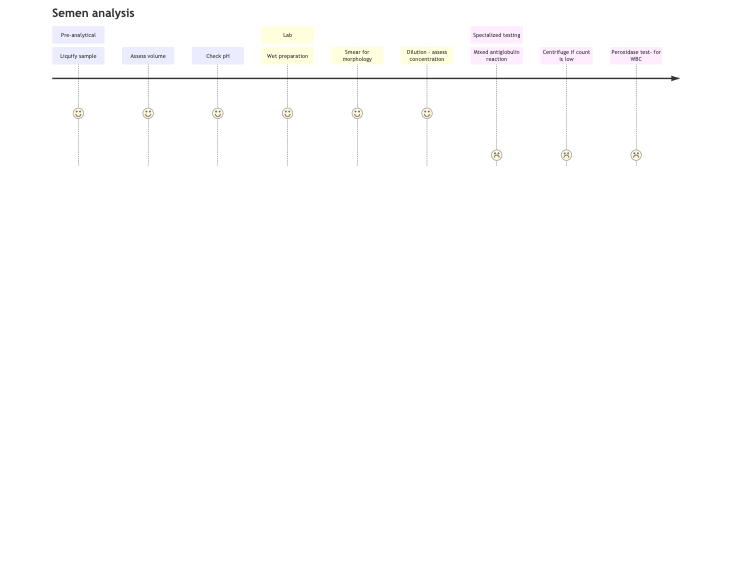
Q. What are the steps for assessment of the semen sample?
-
Q. How is the assessment for motility done?
- It is done using a wet preparation
-
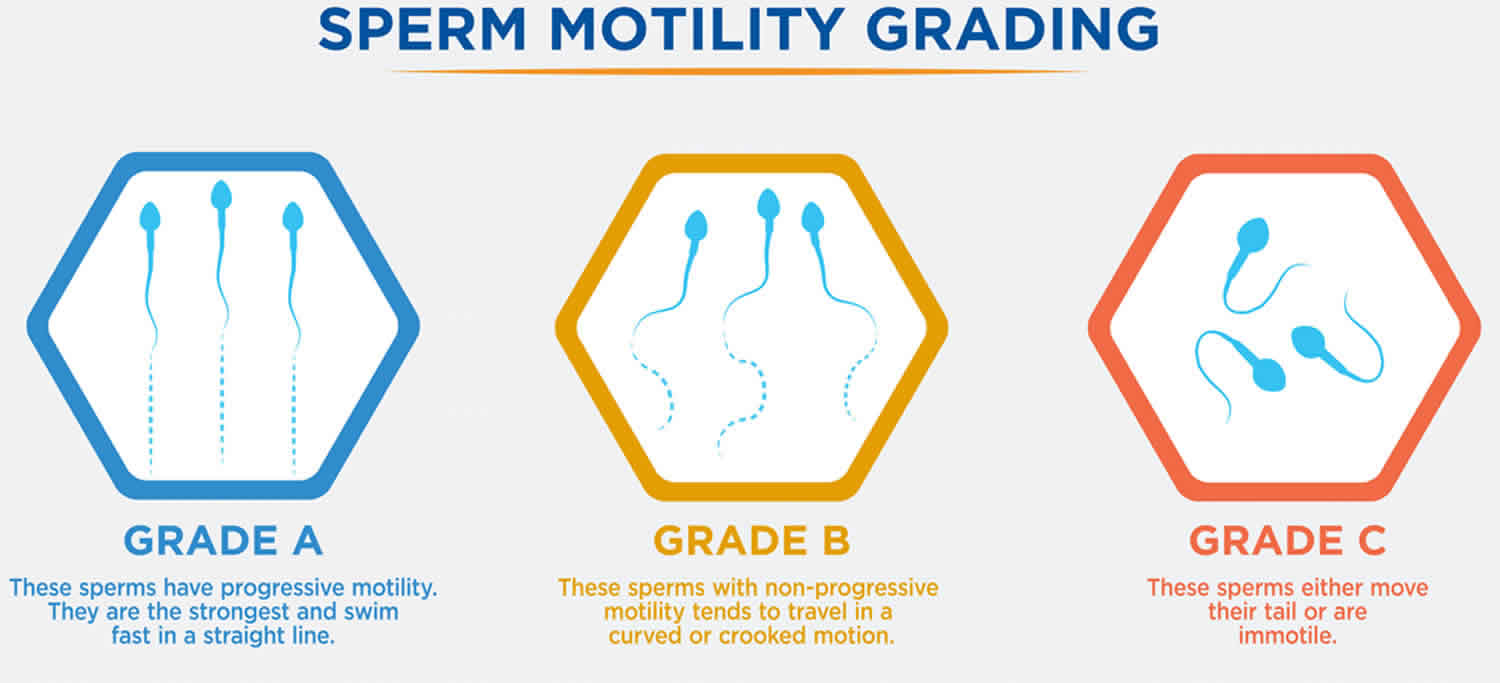
Q. What are the grades of motility?
- Grade A- Progressive forward motility
- Grade B- Non-linear motility
- Grade C- Non-progressive motility
- Grade D- Immotile
-
Q. How is the total motility count calculated?
- Total motility count = Volume in ml x concentration in Million/ml x % motile spems (Grade A to C)
-
Q. True or false, Total motility count is one of the best predictors of male fertility?
- True
-
Q. How is progressive forward motility of the sperm calculated?
- Progressive forawrd motility = Volume in ml x concentration in Million/ml x % motile spems (Grade A only)
-
Q. What is the interpretation of a non-motile sperm?
- A non-motile sperm can either be non-motile due to a defective ciliary mechanism, or it could be a dead sperm
-
Q. Can a non-motile but sperm that is alive be used for IVF?
- It can only be used for ICSI. It cannot be used for conventional IVF or AI since the sperm cannot swim properly, which is necessary for its action.
-
Q. How is the vitality of the sperms tested?
- Vitality refers to whether the sperms are alive or dead
- Vitality is tested using an eosin-nigrosin stain or using hypo-osmotic swelling (HOS) test
-
Q. What is the interpretation of the vitality of the sperm using the eosin-nigrosin stain?
- A dead sperm will have a damaged membrane which would take up the stain. The dead sperm will be stained pink.
- A normal sperm will NOT be stained
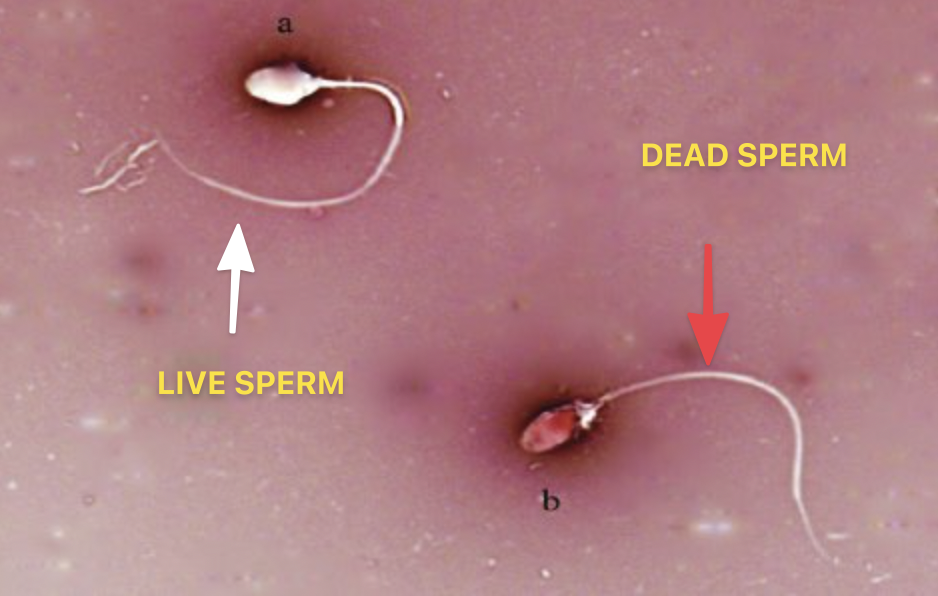
- image from Ref: Khalili MA, Adib M, Halvaei I, Nabi A. Vitrification of neat semen alters sperm parameters and DNA integrity. Urology journal. 2014 May 6;11(2):1465-70.
-
Q. What is the hypo-osmotic swelling (HOS) test?
- This is done by diluting the semen in a hypoosmotic solution
- Normal live sperm will show swelling in the tail because of the entrance of water
- Remember, swollen tail means live sperm
- If >58% of the tails of the sperms are swollen- that suggests NORMAL results
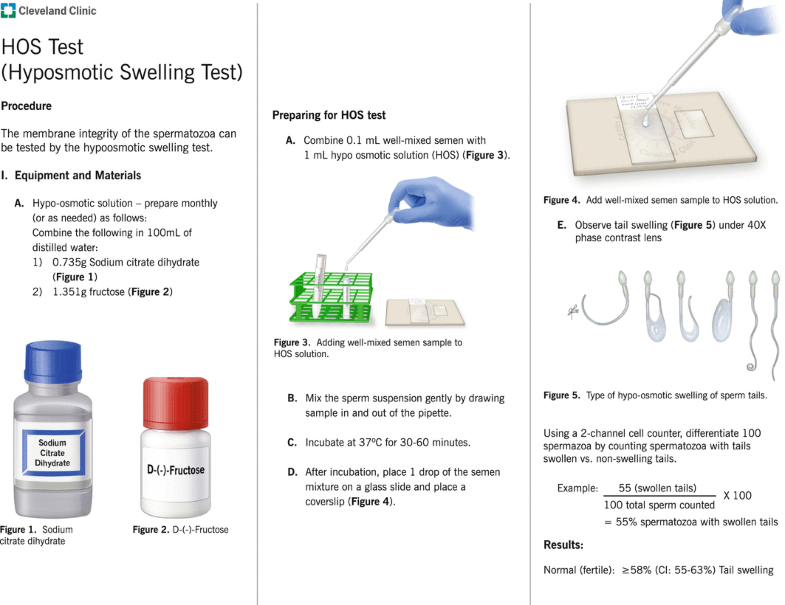
- Ref: Agarwal A, Gupta S, Sharma R. Hypoosmotic swelling test (HOS). InAndrological evaluation of male infertility 2016 (pp. 93-96). Springer, Cham.
-
Q. How is the concentration of the sperm tested?
- This is done using a Neubauer hemocytometer
- If the count is very low- centrifugation is done
-
Q. What is accepted as a normal morphology of the sperm?
- A normal-looking sperm will have some head defects but no angulated tail
- Head - Smooth and oval
- Acrosome- 40-70% of the head
- Midpiece- Symmetrical and linear. It should be 1.5 times the length of the head
- Tail- Uniform and not bent. 8-10 times the size of the head

-
Q. Why are the Anti-sperm antibodies formed?
- The antigen on the sperm surface may be considered foreign for the body
- However, the Sertoli cell makes a tight junction avoiding the sperms to come in contact with the immune system
- However, if this barrier is broken, then the immune system can come in contact leading to the formation of anti-sperm antibodies
- Such a thing can occur in case of vasectomy, torsion of testis, or trauma
-
Q. Anti-sperm antibodies belong to which class of antibodies?
- They belong to IgA and IgG
-
Q. What is the normal WHO level for anti-sperm antibodies?
- <50% of the sperm should be agglutinated with immunoglobulin when testing for anti-sperm antibodies
-
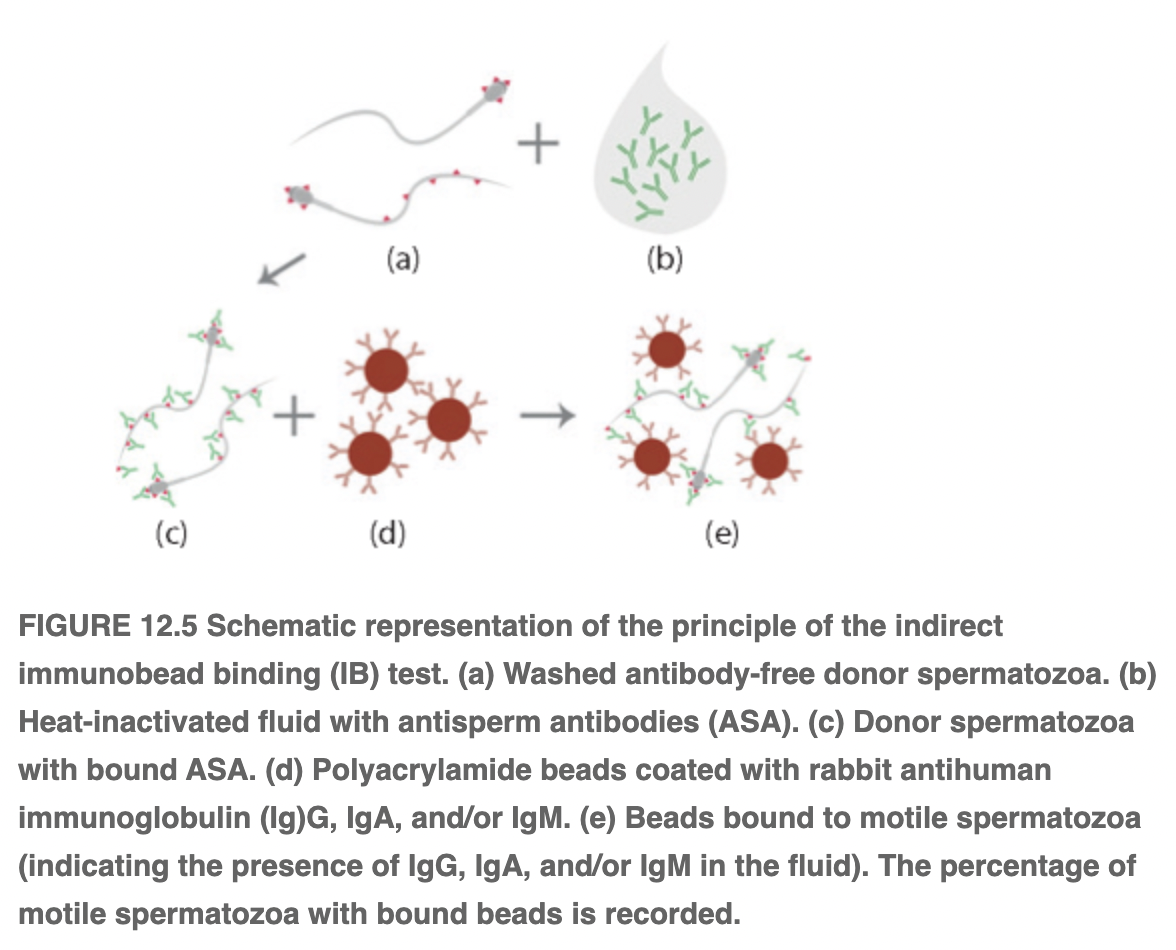
Q. How do we test for anti-sperm antibodies?
- It is done by two methods :
- Direct- directly testing for the antibodies on the spermatozoa
- Indirect- testing for antibodies in sperm free fluid using donor spermatozoa
- There are two tests
-
- MAR test
-
- Immunobead test
-
- #Clinicalpearl
-
Direct test is done for checking for the presence of antibodies on the sperms, while the indirect test is done for checking for antibodies in seminal fluid not containing the sperm
-
- It is done by two methods :
-
Q. Describe the steps in the direct MAR test?
- {{video: https://youtu.be/y1UTFQZy_Dk}}
-
- Take fresh semen suspected to contain anti-sperm antibodies
-
- Take latex particles or RBC bound with anti-sperm antibodies and mix with semen
-
- Take briding antibodies (which are antibodies against anti-sperm antibodies) and mix with the above
-
- The briding antibodies will help form clumps between the latex particles and the sperms if antibodies are present on the sperms, and these clumps will be visible in the microscope
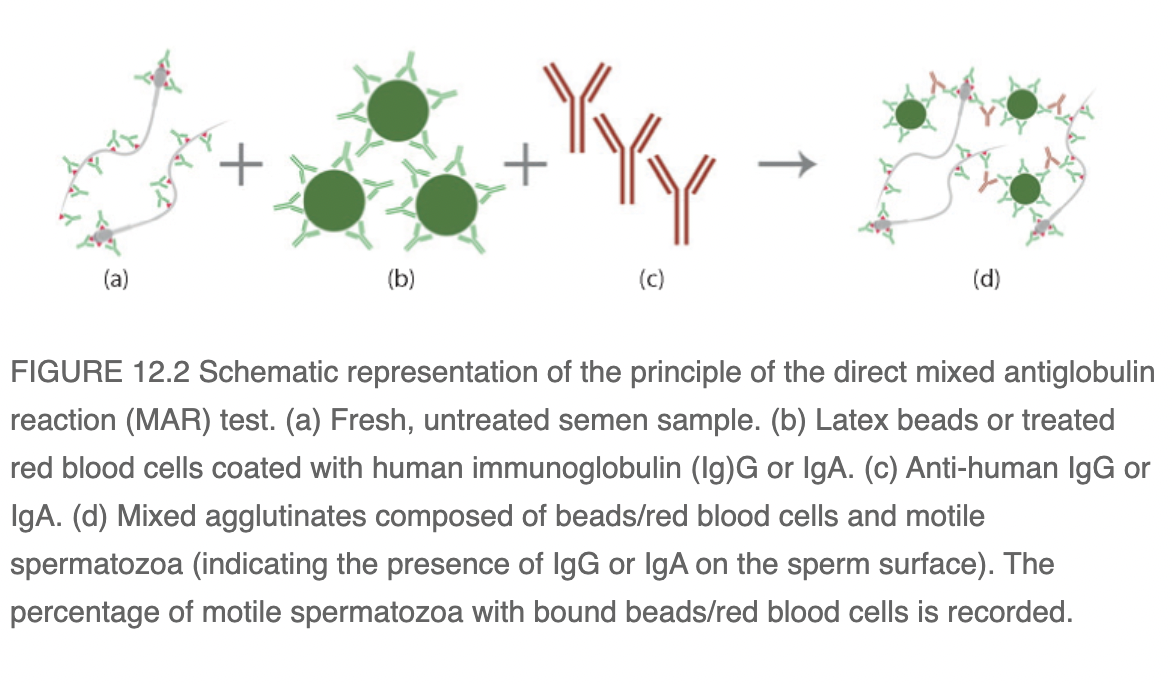
- Ref: https://ebrary.net/42094/health/analytical_techniques_measure_presence
-
Q. Describe the Indirect MAR test?
-
- Here the seminal fluid of the patient is separated from the sperms
-
- A donor sperm not-containing antibodies are taken and mixed with the seminal fluid of the patient. If the seminal fluid of the patient contains antibodies, it will bind with the sperms of the donor
-
- The following steps and interpretation are the same as the direct MAR test above
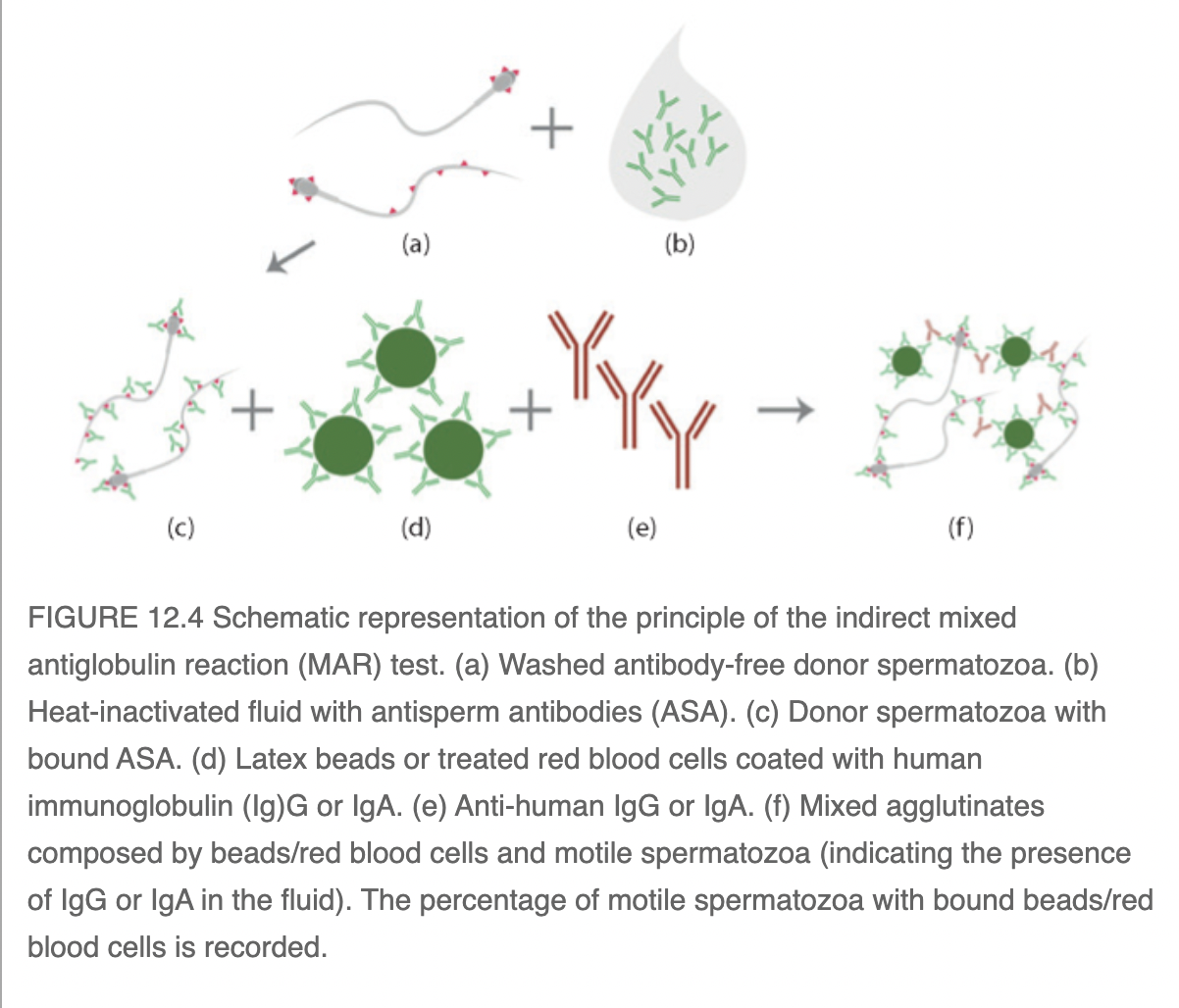
- https://ebrary.net/42094/health/analytical_techniques_measure_presence
-
-
Q. What is the principle of the immunobead test?
- Here, we directly use artificial beads which contain antibodies against the anti-sperm antibodies
- They are mixed with the semen
- If the anti-sperm antibodies are present - then the immunobeads will form clumps, as described above
-
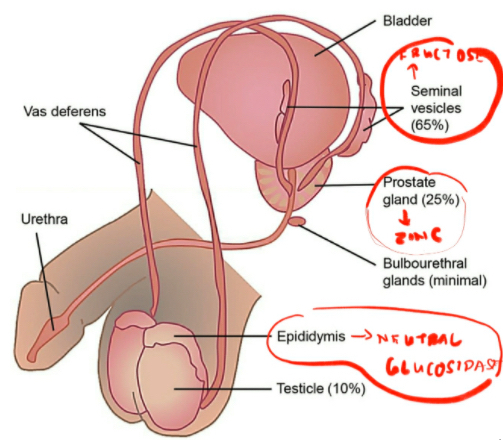
Q. What are the various biochemical tests performed in the semen analysis?
- Peroxidase positive leukocytes ( million/ml) - less than 1
- Immunobead test ( motile spermatozoa with bound beads %) - less than 50.
- Seminal zinc ( micromol/ejaculate) - more or equal to 2.4
- Produced by the Prostate gland
- Seminal fructose (micromol/ejaculate) - More than 13
- Produced by Seminal vesicles
- Seminal neutral glucosidase ( mU/ejaculate) - more than 20.
- Produced by epididymis
-
Q. What is the sources of the fructose in the semen?
- Fructose in the semen is released by the Seminal vesicles
- A positive fructose is normal
-
Q. What does negative fructose with oligo or azoospermia suggest?
- It suggests obstructive azoospermia or absence/loss of function of seminal vesicles
- The absence of fructose suggests obstruction at the level of vas deferens
-
Q. Is WBC ordinarily present in the semen?
- Yes
- However, the quantity is small
- WBC in the semen is tested by peroxidase test, and the level is <1 million/ml
- They are mainly neutrophils
-
Q What is leukocytospermia, and what are their causes?
- Increased peroxidase positive leukocytes in the semen suggests leukocytospermia
- It could be due to
- Genital infection
- Local inflammation
- Smoking
- Alcohol
- Prolonged abstinence
-
Q. What are the consequences of leukocytospermia ?
- Leukocytes lead to increased reactive oxygen species
- This has a negative impact on sperm count, motility, and function
-
Q. When would you suspect Retrograde ejaculation?
- Reduced ejaculatory volume or "dry" orgasm
- Cloudy urine after orgasm
- Testicular volume is normal
-
Q. What are the risk factors for restrograde ejaculation?
- Surgery on the bladder, neck, or prostate
- Diabetes Mellitus
- Multiple sclerosis
- Anti-hypertensive medications
- Treatment of B.P.H
- Tobacco use
-
Q. How is the diagnosis of retrograde ejaculation made?
- Patient is asked to collect semen during masturbation
- Immediately after the act, the patient is asked to pass urine, and the urine sample is collected
- The urine is centrifuged and is examined under a microscope to check the presence of sperms
-
Q. A patient undergoes vasectomy. How soon after the procedure should the semen analysis be done?
- Typically, semen analysis is done 12 weeks after vasectomy (3 months)
-
Q. At what point would a vasectomy be considered unsuccessful?
- If motile sperms are detected even after six months of surgery, then the vasectomy would be considered unsuccessful.
-
Q. What are rare non-motile sperms post vasectomy ?
- In about 20-40% of the patients at the end of 3 months post-vasectomy, we can find some rare non-motile sperms. These sperms generally disappear by 6 months and are unlikely to lead to pregnancy
-
Q. Can a vasectomy be reversed? What time after the procedure can it be reversed?
- Yes
- Vasectomy can be reversed with a microsurgical procedure
- The type of initial surgery and the duration of the period between the surgery and the reversal determine the success of the reversal procedure
- Belker et al. have shown that
- Successful pregnancy can occur in 75% of the cases if the reversal is done within 3 years
- this drops to 30% if reversal is done after 15 years
-
Q. What is Asthenospermia ?
- This refers to reduce the motility of the sperms
- Progressive forward motility <32% is suggestive of an Asthenospermia
-
Q. What is Azoospermia ?
- This refers to the complete absence of sperms even after repetition with centrifugation
-
Q. What is Oligospermia, and what are its grades?
- This refers to reduced sperm counts
- The grades are
- Mild oligospermia: sperm concentration between 10 to 15 sperms/ml
- Moderate oligospermia: between 5 to 15 sperms/ml and,
- Severe oligospermia: below 5 sperms/ml.
-
Q. What is teratospermia ?
- This refers to abnormal sperm morphology. Normal sperms are less than 4% it suggests teratospermia
-
Q. What is Oligoasthenoteratospermia (OAT) ?
- This refers to reduced sperm count, reduced progressive forward motility, and reduced normal morphology of the sperms
- This is the most common pattern observed in infertility