-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Q. What are the various terminologies used for this condition?
- Idiopathic hypogonadotropic hypogonadism
- Congenital hypogonadotropic hypogonadism
- Isolated gonadotropin-releasing hormone deficiency
- Kallman syndrome (A subform of the disease having anosmia)
-
GENETICS
-
Q. What are the modes of inheritance of Congenital hypogonadotropic hypogonadism (CHH)?
- Autosomal dominant
- Autosomal recessive
- X linked recessive
-
Q. What suppresses the GnRH during childhood?
- GABA and opioid peptides
-
Q. What enhances GnRH secretion?
- Glutamate and Kisspeptin
-
Q. Summarize the potential genetic defects that lead to IHH?
- Defective migration of GnRH neurons
- Defective secretion by GnRH neurons
- Defective action of Kisspeptin on GnRH neurons
- Defective action of GnRH neurons on FSH and LH - GnRH receptor defect
- Defect in pituitary transcription factors part of CPHD
-
Q. How common are normosmic and anosmic IHH?
- Anosmic- 50-52%
- Normosmic- 48-50%
-
Q. Which is the most common cause of Normosmic IHH?
- Inactivating mutation in GnRH receptor
- It is also the most common AR form of IHH
-
DEFECT IN GNRH DEVELOPMENT AND MIGRATION
-
Q. What are classical Clinical features of KAL1 mutation?
- X linked
- Ansomia
- Bimanual synkinesia
- Unilateral renal agnesis
- Anosmin-1 defect
- Poor migration of GnRH neurons
-
Q. How do mutations in FGF8 and FGFR1 present?
- Autosomal dominant (AD) inheritance
- Cleft lip/cleft palate
- Maybe Normosmic or anosmic
- Variable degree of hypogonadism, which often reverses
- Dental abnormalities
- Ear abnormality
- Helps in the development of GnRH neurons in their niche
-
Q. How do PROK2 or PROKR2 present?
- AD or Autosomal recessive (AR)
- Normosmic or anosmic
- Helps in the development and migration of GnRH neurons
-
Q. How do defects in CHD7 present?
- Presents as CHARGE syndrome
- C - Coloboma of iris
- Heart problems
- Atresia choanae
- R- retardated growth and development
- G- genital abnormality
- E- ear abnormality
-
Q. What is choanal atresia?
- Choanal atresia is a congenital disorder where the back of the nasal passage (choana) is blocked, usually by abnormal bony or soft tissue (membranous) due to failed recanalization of the nasal fossae during fetal development.
-
DEFECT IN GNRH SYNTHESIS AND RELEASE
-
Q. How do mutations of GPR54/KISSR or KISS1 present?
- Presents with Normosmic IHH
- GPR54/KISSR (receptor) mutation are known
- But KISS1 (ligand) mutation are not known
- They are Autosomal recessive
-
DEFECT IN GNRH FUNCTION
-
Q. How do patients with LH beta defects present?
- Males- absent puberty and azoospermia
- Females- large ovaries with normal/late menarche and oligomenorrhea due to anovulatory cycles
-
Q. How do patients with FSHbeta mutation present as?
- Females – primary amenorrhea and lack of secondary sexual characteristics
- Male- Azoospermia
-
Q. Which genetic test to do if a child has cleft lip or cleft palate?
- FGF8 or FGFR1
-
Q. What about bimanual synkinesis?
- KAL1
-
Q. What is there is obesity with hypogonadotropic hypogonadism?
- Leptin
- Leptin receptor
- PCSK1
- Prader Willi
- Bardet Bledel
-
Q. What genetic test would you perform if the child has CHH hearing defect?
- CHD7- CHARGE syndrome
- SOX10
- IL17RD
-
Q. Hypo hypo with Split-hand foot malformation?
- FGFR1
-
Q. Enlist the 6 genes involved in Kallmann syndrome (Hypo hypo with anosmia)?
- KAL1- X linked
- FGF8, FGFR1- AD with incomplete penetrance
- PROK2, PROK2R- AR/AD
- CHD7
-
KAL1 gene mutation- Kallman syndrome
-
Q. What is the primary defect in this condition?
- Impaired migration of GnRH neurons to the ventral hypothalamus during embryogenesis
-
Q. Which protein helps in this migration?
- Anosmia
- This is the product of the KAL1 gene
-
Q. What is the typical clinical phenotype of KAL1?
- They are the most severe phenotype, with
- Micropenis
- bilateral cryptorchidism
- Small testis
- Poorest response to spermatogenesis
- Most penetrant of the genes
-
Q. Can KAL1 mutation occur in Non- anosmic individuals?
- It has never been reported in Non-ansomic individuals
-
FGFR1 mutation
-
Q. What is the mode of inheritance in FGFR1 mutation?
- It is Autosomal dominant
-
Q. Does it cause anosmia or not?
- It can lead to both anosmic and non-anosmic features
-
Q. Is it more common in males or females?
- More in males
- This is because in cases of halpoinsuffieicny, increase anosmin in females offsets the defect due to FGFR1 mutation
-
Other mutation
-
Q. How does FGF8 present?
- Similar to FGFR1
- Both anosmic and non – anosmic forms
-
Q. How do mutations in PROK2 and PROKR2 present?
- They in varied form with both KS and nIHH
- Thought to be AR, but other forms of inheritance also
-
Q. What are, Kisspeptin, Metastin, and GPR54?
- This system is a major gatekeeper of the Pubertal pathway
- Kisspeptin is the 145 amino acid precursor
- This is cleaved to produce Metastin, which is 54 amino acid final product
- This acts on GPR54, which is the receptor- now this is called Kisspeptin receptor
-
Q. What is CHARGE syndrome?
- Coloboma,
- heart defect,
- atresia choanae (also known as choanal atresia),
- retarded growth and development,
- genital abnormality,
- ear abnormality
-
Q. What is the diagnostic criteria used for the diagnosis of CHARGE syndrome?
- Blake-Verloes criteria
-
Q. CHARGE syndrome is caused by a mutation in which gene?
- CHD7 gene
-
**BIOLOGY OF GNRH NEURONAL SYSTEM **
-
Q. Where do GnRH neurons originate?
- They originate in the olfactory placode and migrate to the hypothalamus
- They arise both from the neural crest and ectodermal progenitors
-
Q. Where are the GnRH neurons present at birth?
- By birth, they have reached their final place in the hypothalamus
-
Q. What is the KAL1 gene called in new nomenclature?
- It is now called ANOS1
-
Q. Which genes help in the development of the GnRH neuron in its niche and also craniofacial development?
- FGF8
- CHD7
- SOX10
-
Q. Which genes help in the migration of GnRH neurons?
- KAL1
- PROK2 and PROKR2
- WDR11
- SEMA3A
- FEZF1
-
Q. What cells produce INSL3 in boys?
- Leydig cells
-
Q. What is the impact of LH and FSH on the ovary?
- LH- theca cells to produce androgens
- FSH- Granulosa cells to produce estrogen
-
Q. What produces inhibin B and AMH in boys and girls?
- Boys- Sertoli cells
- Girls- granulosa cells
-
Q. How can CHH be diagnosed in infancy?
- Males – presenting with Micropenis/ Cryptorchidism must be studied
- Females with a family history of CHH
-
Q. When is hormonal testing for CHH done in infancy?
- The goal is to detect the presence/absence of mini puberty
- Hormonal profile is done at 4-8 weeks
- FSH is a better marker than LH
- Undetectable FSH and Poor response to GnRH is diagnostic of IHH in infancy
-
CLINICAL PRESENTATION
-
Q. Is IHH/C.H.H more common in males?
- True
- It is mainly seen in males with M: F ratio of 5:1
-
Q. What is the presentation of CHH during the neonatal period?
- Micropenis
- Cryptorchidism
-
Q. In which mutation cleft lip/cleft palate is more common?
- FGFR1/FGF8 mutations
-
Q. What is Kallmann’s syndrome?
- Ansomsia + Hypogonadotropic hypogonadism is Kallmann’s irrespective of the underlying mutation
-
Q. How do CHH present in childhood?
- Delayed puberty
- Skeletal abnormality – Cleft lip/cleft palate
- Anosmia
-
Q. Do all patients with CHH have delayed puberty of the same variety?
- No
- There is a difference in presentation
- Some have severely delayed puberty from the onset
- Others have some pubertal development followed by the pubertal arrest
- Some have normal puberty but have problems in adulthood with infertility- this is called adult-onset HH
-
Q. Do patients with CHH have eunuchoid proportions?
- Yes
- It is typical
-
Q. Can these patients have pubic hair?
- Yes
- Pubic hair is often present due to adrenarche being present- DHEA-S is usually produced normally
- If adrenarche is also absent, think of DAX1 mutation or CDGP
-
Q. What is the fertile eunuch variant of the syndrome?
- Seminiferous tubule and testis size is normal
- But Leydig cell function is impaired, so the Testosterone is low
- So fertility is preserved, but testosterone is low
- This is a fertile eunuch variant of IHH
-
Q. Why is gynecomastia atypical in these patients?
- This is because there is no FSH and LH- hence little testosterone and low testicular aromatase activity –leading to little estrogen formation
-
Q. Which are the associated congenital disabilities seen in these patients?
- Unilateral renal agenesis
- Syndactyl
- Cleft lip/ palate
- Anosmia/hyposmia
- Unilateral/bilateral cryptorchidism
- Synkinesia (mirror movements)
- Color vision
-
Q. Which of the above are commonly seen with KAL1 mutation?
- Unilateral renal agenesis and synkinesia are classically seen with KAL1 mutation
-
Q. Which test is used to identify the anosmia/hyposmia in these patients?
- University of Pennsylvania smell identification test (UPSIT)
-
Q. What will be the MRI findings in these cases?
- Pituitary will be normal
- Small cuts 1 mm in size through the olfactory placode to look for the olfactory bulb must be done
-
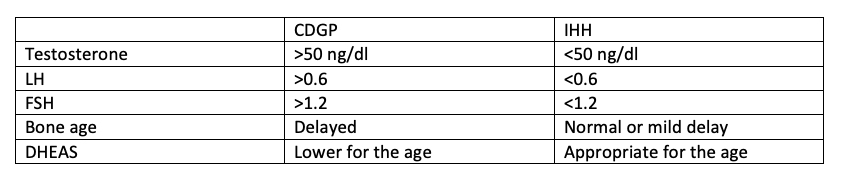
Q. How will you differentiate Constitutional delay of growth and puberty (CDGP) from Idiopathic hypogonadotropic hypogonadism ?
- Step 1: History and Examination
- Points towards CDGP
-
- Family history of CDGP
- o Age of menarche of Mother- >15 years is delayed (After 10th grade)
- o Continued growth of father after completing school
- o Growth spurt after 11th grade in father
- o Started shaving after 11th grade
-
- Points towards IHH
-
- Anosmia
-
- Testicular volume 1-2 ml with a bone age of >12 years
-
- Micropenis at birth
-
- Cryptorchidism at birth
-
- Midline defect
-
- Cleft lip / cleft palate
-
- Points towards CDGP
- Step 2: Basic Investigations
- Tests to order
-
- Total Testosterone
-
- LH
-
- FSH
-
- Bone age
-
- DHEAS
-
- Tests to order
- Step 3- Advanced Tests and Stimulation tests
-
- Inhibin B
-
- GnRH Agonist testing
-
- HCG stimulation test
- Inhibin B
- • Value < 35 pg/ml- IHH for sure
- • 35-100 pg/ml- Either way-more in favor of CDGP
- • >100 pg/ml- CDGP for Sure
-
-
- GnRH agonist testing
- LUPEROLIDE PROTOCOL (Lakhani protocol developed from Street et al.)
-
- Baseline LH
-
- Inj LUPRIDE 1 mg vial (0.5ml) in Insulin – 100 IU syringe order
- a. 0.25 ml (0.5 mg) – 25 units in Insulin syringe
- b. Inject Subcutaneously
-
- Repeat LH after 2 hr and 4 hr
- Interpretation
-
- Peak LH > 6.1 - Suggestive of CDGP
-
- Peak LH <2.8 IHH
-
- 2.8-6.1- either way – Favour CDGP
-
-
- TRIPTORELIN PROTOCOL
-
- Baseline LH
-
- Inj DECAPEPTYL (Triptorelin) 1 ml subcutaneous (100 ug)- 100 IU in insulin syringe
-
- Check LH and FSH after 2 hrs and 4 hrs
-
- If Peak LH >5 – suggestive of CDGP
- a. Dergos et al. say 14 IU/l is more discriminatory
-
- HCG stimulation test
-
- Baseline testosterone
-
- In HCG (FERTIGYN), 1500 IU IM on alternate days for 3 days
-
- Day 7 – Repeat testosterone
- a. >230 ng/dl – CDGP
-
- ALTERNATE SINGLE DOSE HCG PROTOCOL (DERGOS et al.)
-
- Baseline Testosterone
-
- Inj HCG (FERTIGYN) – 5000 IU im
-
- Repeat testosterone after 72 hrs
- a. Tetosterone >260 ng/dl- CDGP
- b. <86 ng/dl- IHH
- Step 4- Follow Up
-
- Inj TESTOVIRON 50 mg monthly for 3 months
-
- Recheck Testosterone 1 month after the last injection
- a. Testosterone > 300 ng/ml- Suggestive of CDGP
- b. <300 ng/ml- IHH
-
- Step 1: History and Examination
-
**TREATMENT **
-
Q. What are the treatment options for these patients?
- Gonadal steroids
- Human gonadotropins
- Pulsatile GnRH
-
Q. What is the disadvantage of giving gonadal steroids to these patients?
- It impairs spermatogenesis
-
Q. How is Pulsatile GnRH given?
- It is given via a minipump that infuses GnRH every 120 min subcutaneously over the 60s
- This matches the LH pulse, which is every 120 min
- Starting dose is 25 ng/kg/bolus
-
Q. Give the treatment protocol for CHH using HCG and HMG
- Step 1- Baseline investigations
-
- Document Testicular volume
-
- Serum testosterone
-
- FSH / LH
-
- Inhibin B (optional)
-
- Semen analysis
-
- Step 2- Start HCG
-
- Inj HCG 2000 IU Intramuscularly/Subcutaneously three times a week on Monday, Wednesday, and Friday
- a. It may be a powder that needs to reconstituted
-
- Serum Testosterone monthly
-
- Target testosterone to 400-800 ng/dl
-
- Increase dose of HCG by 1000 IU every month if the target testosterone is not achieved
-
- Once Testosterone is in target range- Sperm count every month
-
- Target sperm count of 5-10 million/ml
-
- If the sperm count is <5 million /ml after testosterone has been normal for 6 months, than add HMG
-
- Step 3- HMG
-
- In HMG 75 units INTRAMUSCULAR/Subcutenous in the same syringe as HCG start with once a week - can be increased further if required.
-
- Monitor sperm count every 1-2 months
-
- If sperm count <5 million/ml – increase dose of HMG to 150 IU
-
- Step 1- Baseline investigations
-
Q. Can CHH reverse?
- Spontaneous reversal is often seen in many patients
- Patient on gonadotropins with normal testis size and testosterone- Gonadotropins may be stopped for 2-3 months to assess reversibility
- Patients on gonadal steroids- stop the testosterone for 2-3 months and re-evaluate if the testis is normal in size. Testosterone will not normalize the testis size normally
-
Q. What proportion of patients with CHH have a spontaneous reversal?
- 10%
-
Q. What is CHH with Cerebellar ataxia?
- Gordon Holmes syndrome
-
Q. Why do patients with CHH have no genital ambiguity?
- This is because in the 1st trimester- the testosterone is produced by fetal Leydig cells in response to placental HCG
- Only if there is Testosterone deficiency in 1st Trimester – there is genital ambiguity
- Hence these patients do not have genital ambiguity
-
Q. Can Kallmann be diagnosed before puberty?
- It is sometimes diagnosed in infancy with micropenis and cryptorchidism
- Later on, it is diagnosed in childhood with anosmia and synkinesis but suspected only if there is a family history of this syndrome
-
Q. Do patients with CHH present as short stature?
- Generally no
- They generally have normal structural development in childhood
-
Q. Why is inhibin B low in patients with CHH?
- Inhibin B is a marker of Sertoli cell function, which in turn is dependent on FSH
- Since FSH is low- the Sertoli cell function is impaired, and hence inhibin B is low
- This also correlates with the testicular volume
-
Q. What is the role of AMH in the diagnosis of CHH?
- AMH marks pubertal testicular maturation
- Because of the lack of intratesticular testosterone concentration, AMH value is also low
-
Q. Which secondary cause of hypogonadotropic hypogonadism closely mimics CHH?
- Primary juvenile hemochromatosis
- Hence ferritin and Transferrin saturation must be done in all these cases
-
Q. What are the role of MRI in Kallmann?
- Rule out other etiology of hypogonadotropic hypogonadism
- Look for the absence of olfactory bulbs
- Cerebellar involvement- Gordon holmes syndrome
- Corpus callosum defects- often associated
-
Q. What is the importance of doing USG in patients with Kallmann's?
- To look for renal agenesis
- To document exact testicular volume
- To determine the normal anatomy of the Seminal vesicles and vas deferens
-
Q. Which 2 tests in the physical examination are essential for classifying a case of hypo hypo?
- Semiqualitative test for olfaction in the index case and family members- to look for anosmia vs. hyposmia
- Close examination of the outer ear and hearing defect – CHARGE syndrome
-
Q. What test is used for smell identification in patients with CHH?
- University of Pennsylvania smell identification test
- This is currently the gold standard for smell identification
-
Q. What is the Indian smell test kit?
- I-smell test
- This is developed by Gupta et al. of GB Pant
-
Q. Which are the new biomarkers in the diagnosis and follow-up of CHH patients?
- Kisspeptin
- INSL3
- Inhibin B
- AMH
-
Q. What is Oligogenecity?
- Two or more mutations present in the same CHH patient
-
Q. What is the difference between camptodactyly and clinodactyly?
- Clinically, a bending or curvature of the finger in the plane of the palm is described as clinodactyly, a word derived from the Greek liner, “to bend,” and dactylos, “a finger.”
- A flexion deformity at the proximal interphalangeal joint is camptodactyly from the Greek “bent finger.”
-
Q. Which condition presents with adrenal insufficiency before puberty and Hypo hypo during puberty?
- AHC- Adrenal hypoplasia congenital, also called congenital X linked adrenal hypoplasia
- This is caused by DAX1 mutation
- Classic X-linked adrenal hypoplasia congenita
- Classic X-linked AHC includes the triad of a) primary adrenal insufficiency (PAI), b) hypogonadotropic hypogonadism (HH), and c) impaired fertility.
- It has a direct effect on spermatogenesis also
- Hence attempts to improve spermatogenesis with HCG – shows inadequate response
- AHC- Adrenal hypoplasia congenital, also called congenital X linked adrenal hypoplasia
-
Q. What is Gonadorelin?
- It is a natural form of GnRH