-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Q. Define Menopause
- Menopause is the permanent cessation of menses
- It is defined 12 months after the last menstrual cycle
-
Q. What is the average age of menopause worldwide?
- 51.4 years
- It has not changed over a period of time
- It is determined mainly by genetic factors
- smoking reduces the age of menopause
-
Q. What is the average age of menopause in India ?
- 46.2 years
-
Q. What is late menopause?
- More than 54 years
-
Q. What is early menopause?
- 40-45 years
-
Q. What is Premature ovarian insufficiency (POI)?
- Menopause < 40 years of age
-
Q. What is the impact of smoking on menopause?
- Induces early menopause
-
Q. Can AMH predict the age of menopause
- Yes
- AMH <0.2 ng/dl
- Median time to menopause is:
- 45-48 years age - 6 years
- 35-39 years - 9.94 years
- Median time to menopause is:
- A recent study published in JCEM says
- AMH is a helpful predictor for menopause, but its effectivity as a predictor reduces with aging
- Up to the age of 35-40, it is a valuable predictor of early menopause
- for every 0.1 ng/ml reduction in the AMH value below 2 ng/ml - the risk of early menopause increases by 14%
-
Q. What happens to Inhibin B as the patient nears menopause?
- Inhibin B levels start declining
- It is the earliest marker of follicular decline
-
Q. Which is the most prominent source of estrogen post-menopause?
- Estrone
- This is derived from peripheral conversion of adrenal androstenedione
-
Bone loss and menopause
-
Q. What is the rate of bone loss in the perimenopausal period?
- The rate of bone loss 1.5 years before menopause and 1.5 years after menopause is 2.5% per year
- Compare to premenopausal women in which the bone loss is 0.13% per year
-
Q. What is a segment of bone predominantly lost in the perimenopausal period?
- The bone loss is mainly from the trabecular bone (spine) instead of the cortical bone loss
-
- Estrogen is more important for trabecular and overall bone formation
- However, Testosterone is more important for periosteal apposition
- This is the reason why men tend to have thicker cortical bones
-
Q. What are the estrogen receptors present on the bone?
- Both ER-alpha and ER-beta are present on the various cells of the bone
- ER-alpha is more critical for bone effects
- ER-beta is predominating in the trabecular bone
-
Q. Does estrogen increase bone turnover, or does it reduce bone turnover?
- Estrogen is known to reduce the bone turnover
- It causes apoptosis of osteoclasts - this is the primary action
-
Q. What is the impact of estrogen on pro-inflammatory factors?
- Estrogen reduces the pro-inflammatory factors like IL-1, IL6, and TNF-alpha
- These factors inhibit the action of RANK-Ligand
-
Q. What is Riggs' theory of two phases of bone loss that occur following Menopause?
- The first is the rapid phase of bone loss
- This occurs in the early perimenopausal period
- This is mainly trabecular bone loss
- This is devastating, and about 20-30% of the bone is lost in 4-5 years
- The second phase is a slower phase of bone loss
- This is associated with secondary hyperparathyroidism
- this is mainly cortical bone loss
- it occurs about 1-2% per year
- The first is the rapid phase of bone loss
-
Q. Do genetic factors influence this bone loss?
- Genetic factors have more influence on the attainment of the peak bone mass rather than on the bone loss that occurs after menopause
-
Q. How can one assess bone microarchitecture?
- HRpQCT (High-resolution peripheral Quantitative CT) can help assess the bone microarchitecture
-
Q. What dose of conjugated equine estrogens (CEE) is required to prevent bone loss?
- The standard therapy does is 0.625 mg
- However, doses of 0.3 mg can also successfully prevent bone loss
-
Q. Does Tibolone prevent bone loss ?
- Yes
- Tibolone has also been known to prevent bone loss
-
Q. What should be the calcium and Vitamin D intake in postmenopausal women?
- Calcium- 1200-1500 mg/day
- Vitamin D - 400-800 IU/day
-
Cardiovascular effects of Menopause
-
Q. Is it true that younger women have less CV risk than men?
- Yes.
- Premenopausal women have three times less CV risk compared to men of the same age
- Early menopause/Premature ovarian insufficiency (POI) or menopause before the age of 35 years substantially increases the lifetime CV risk.
- Despite this, CV disease is the leading cause of death in women- however, the risk becomes equal to men only at 70-75 years of age.
- Surgical oophorectomy done early also increases the CV risk. Oophorectomy up to the age of 60 years increases the CV risk!
-
Q. What happens to lipid profile after Menopause?
- All components of the lipid profile worsen
- Increase in total cholesterol
- Increase in LDL
- Increase of oxidized LDL
- Reduction of HDL
- Increase of VLDL
- All components of the lipid profile worsen
-
Q. Are Estrogen and progesterone receptors found on the coronary arteries?
- Yes!
- ER-beta is found on the coronary arteries
-
Q. What is the timing hypothesis?
- Subanalysis of the Women's health initiative and other studies have shown the dual nature of the CV risk in patients on Menopause hormonal therapy
- It says if the MHT is started <6 years of menopause or in younger women- there is a reduction in the CV risk
- However, if it is used later- there is increased CV risk
- The duration of therapy also has an impact- with a shorter period of treatment <5 years- being cardioprotective
- This is the timing hypothesis
- Subanalysis of the Women's health initiative and other studies have shown the dual nature of the CV risk in patients on Menopause hormonal therapy
-
Q. Is there a mechanical action here for the timing hypothesis?
- Yes
- It is said that once Atherosclerosis sets in, the coronary arteries do not respond to the estrogen via its receptors
- Hence younger women may benefit from Menopause hormonal therapy, but older women do not have this estrogen protective effect on the vessels. On the other hand, the additional risks like coagulation, etc., increase.
- Another theory is that with aging, cholesterol called 27-hydroxycholesterol accumulates in the body, which competes with estrogen for binding with its receptors.
-
Q. What are the other changes that occur with Menopause that impact the CV risk?
- Increased risk of diabetes mellitus
- Increased inflammatory markers
- Reduced blood flow to all vascular beds
- Reduced prostacyclin
- Nitrous oxide formation and activity reduces
-
Q. Is there an increased coagulation risk?
- No
- Increased risk of coagulation is countered by an increase of anticoagulation factors
-
Q. Why is there an increased risk of diabetes mellitus in these women?
- This is because of increased Insulin resistance
- This is also reversed by estrogen
-
Q. What is Early harm theory?
- This is similar to the timing hypothesis
- Women's health initiative subanalysis showed that women that have to increase CV risk with Menopause hormonal therapy are women who are older or already have evidence of Atherosclerosis
- Now, the risk of an event in them occurs early- within 1-2 years of starting the Menopause hormonal therapy
- The possible explanation given for that is that perhaps estrogen increases the plaque instability hence leading to the CV event
- Also, it was observed that women on statin did not have increased CV risk!
- And we know that statin causes plaque stability
-
Q. Can you substantiate this from a study done on primates?
- Several interesting studies are done with this theory in primates.
- In these studies, the primates were subjected to oophorectomy and then given estrogen
- If the hormonal therapy was started within 1-2 years of oophorectomy - a substantial benefit was seen. However, this benefit was lost if the treatment was started late
- Additionally, primates on an atherogenic diet early on had blunted benefit compared to those on a more healthy diet early on.
-
Q. What is the argument against the timing hypothesis?
- One paradox of the timing hypothesis is that younger women per se may have a reduced risk of CV event
- Hence we will need to follow them up for a long time to see the benefit vs. harm.
- Alternatively, we can use some other surrogate markers of CV risk like CT Calcium score and Carotid intima-media thickness
-
Q. Have these surrogate markers been studied in any trials?
-
Yes
-
Two trials have evaluated this:
- KEEPS trial
- This trial found benefits in CT Calcium score but not in Carotid intima-media thickness
- However, this trial did not have a comparative arm and was conducted only for a follow-up of 4 years
- ELITE trial
- This trial found a benefit in the Carotid intima-media thickness but no benefit in the CT Calcium score in women who were started on Menopause hormonal therapy early on
- KEEPS trial
-
Q. Why is it important to have Menopause hormonal therapy as an option for women for CV risk reduction?
- The benefits seen by the timely use of MHT in these women are much more substantial than any other therapy for CV risk reduction in women
- It must be remembered that aspirin and statin used in men for CV risk reduction do not have as much benefit in women
- An only intervention which has substantial benefit apart from the Menopause hormonal therapy are Lifestyle measures!
-
Q. Summarize the topic of Menopause hormonal therapy and CV risk?
- The timing hypothesis
- Early initiation of MHT (<10 years of onset of menopause and <60 years) has substantial benefit in terms of CV risk reduction
- The Early harm hypothesis
- The women already having Atherosclerosis have a negative impact of MHT.
- Women with Premature ovarian insufficiency (POI) definitely must be given MHT- because the risk is very high in these women
- The types of Estrogen and progesterone preparations may also have some impact.
- The timing hypothesis
-
-
Stroke
-
Q. Risk of what type of stroke is increased in women on menopause hormonal therapy?
- There is an increased risk of Ischemic stroke and not hemorrhagic stroke
-
Q. Do the dose of estrogen impact the risk of stroke?
- Yes.
- The stroke risk is influenced by the dose of the estrogen
-
Q. Is the risk the same in younger postmenopausal women?
- Interestingly, according to the authors of the chapter, the risk in younger postmenopausal women is mainly due to thrombosis risk, and this risk is marginal
- This is the same as younger women developing thrombosis on OCP
- Transdermal estrogen therapy and a lower dose of estrogen reduces the risk of a thrombotic stroke
-
Q. What are the risk factors for developing Venous thromboembolism in these women?
- The absolute risk is negligible. However, it must be kept in mind
- The VTE events generally occur within the first 1-2 years of estrogen therapy
- The type of estrogen used has an impact- transdermal estrogen has less risk
- Type of Progesterone used also has an impact- again; Medroxyprogesterone has a higher risk compared to newer micronized or natural progesterone
- Obesity is a risk factor
- Prior history of embolism- strong risk factor
- Factor, V Leiden mutation, is a risk factor
- Family history of Embolic events must be kept in mind
-
Q. Apart from VTE, what is the other estrogen-specific risk in relation to stroke?
- Some women have an idiosyncratic reaction to estrogen that leads to accelerated hypertension
-
Diabetes mellitus
-
Q. What are the body composition changes that occur with menopause?
- Increase central fat deposition
- Weight gain
- Reduced muscle mass- Sarcopenia leading to Sarcopenic obesity
-
Q. Is Increased risk of diabetes after menopause because of aging or because of estrogen deficiency?
- This has been a topic of debate for a long time.
- The SWANN study has shown that the risk of Type 2 Diabetes mellitus was higher in women having lower estrogen levels - hence there is a dependence on estrogen as well
- Additionally, several studies have shown that early menopause is associated with a higher risk of type 2 diabetes mellitus
-
Q. What are the reasons for the development of Type 2 Diabetes mellitus after menopause?
- The risk of type 2 diabetes is mainly driven by increased Insulin resistance
- This is because of
- Reduce the efficiency of ER-alpha receptor reduces energy expenditure leading to more fat accumulation
- Menopause is a state of relative androgen excess leading to increased insulin resistance
- Change in body composition - produces sarcopenic obesity, which is a state of low-grade inflammation
- There is evidence from animal studies that estrogen helps maintain good insulin secretion, and reduced insulin secretion is seen after oophorectomy in animal studies. This may be contributory to the increased risk of Type 2 diabetes.
-
Q. Is there are correlation between Vasomotor symptoms and risk of Type 2 Diabetes mellitus?
- Yes
- Several studies have shown that perimenopausal women with Vasomotor symptoms are 18% more likely to develop type 2 diabetes
-
Q. Does Menopause hormonal therapy reduce insulin resistance?
- Yes
- Meta-analysis of several trials, which included Women's health initiatives etc. showed that there is a 36% reduction of HOMA-IR values following the initiation of MHT
-
Q. Is the mechanism of reduction of Insulin resistance with Menopause hormonal therapy because of reduction of weight?
- No
- The benefit of MHT on Insulin resistance seems to be weight neutral
- There is improvement despite not losing weight
- This must be because of
- Estrogen improves insulin resistance in peripheral organs
- Estrogen improves insulin secretion from pancreatic beta-cells
-
Q. Does the effect of progesterone neutralize the beneficial effect of estrogen?
- Yes and No
- It depends on the type of progesterone
- Medroxyprogesterone acetate is known to have glucocorticoid like activity and hence increases insulin resistance
- Levonorgestrel has androgenic property and hence again would increase Insulin resistance
- The following progestins do not increase insulin resistance
- Dydrogesterone
- Norethisterone acetate
- Micronized progesterone
-
Q. Does transdermal estrogen have more benefit on the metabolic parameters?
- No
- On the contrary, oral estrogen is more beneficial for glucose metabolism, perhaps due to its increased hepatic first phase metabolism
- Transdermal estrogen has less benefit for glucose metabolism
-
Decision to use Estrogen
-
Q. What are the current broad recommendations for the use of Menopause hormonal therapy?
-
- Use it for younger women
- <60 years
- <10 years since menopause
-
- Use it for a short duration
- around five years
-
- Use of modern estrogen and progesterone preparation
-
- Don't use it for cardiovascular or bone protection
-
- Use mainly for vasomotor symptom relief
-
-
Q. In terms of CV risk calculators, which patients can be given Menopause hormonal therapy and which patients cannot be given Menopause hormonal therapy?
- 5-10% CV Risk - Use Transdermal estrogen
- More than 10% risk- avoid all together
-
Q. What about breast cancer risk?
- Using the national cancer institute breast cancer risk
- Intermediate risk - 1.6-5%- Use with caution
- High risk - >5%- Avoid MHT
- Using the national cancer institute breast cancer risk
-
Phytoestrogens
-
Q. What are Physoestrogens ?
- They are plant-based estrogen
- They are not active on their own- however, when given orally, the colonic bacteria cleave the glycoside component to produce the biologically active form
- Phytoestrogens are like SERMS- they have agonist action in some tissue and antagonist action in some tissues
-
Q. What are the clinical benefits of Phytoestrogens?
- They are mainly helpful in Vasomotor symptoms of menopause
- They have little benefit on vaginal dryness and boneless
-
Q. Are they proven in any clinical trials?
- No
- They are not recommended for use by all the available guidelines
-
-
Menopause hormonal therapy
-
Q. What are the two common groups of symptoms of menopause
-
- Vasomotor symptoms
- Hot flashes
- Night sweats
-
- Urogenital symptoms
- Atrophic vagina - leading to irritation and dryness
- Dyspareunia
- Atrophic urethral epithelium- lead to micturation disorders
- These symptoms rapidly improve with Menopause hormonal therapy
-
-
Q. What was the purpose of Menopause hormonal therapy given in the past?
- In the past, MHT was given to prevent
-
- Coronary artery disease
-
- osteoporosis
-
- Dementia
-
- In the past, MHT was given to prevent
-
Q. What did the Nurses' Health Study show? #ClinicalTrials
- It showed
- Reduced risk of Coronary artery disease
- Increased risk of breast cancer in the combined E+P group
- It showed
-
Q. What did the Women's health initiative show? #ClinicalTrials
- This was a prospective RCT
- It was stopped early
- The combined E+P group showed
- Increased risk of Cardiovascular disease
- Coronary artery disease
- stroke
- Venous thromboembolism
- Increased risk of breast cancer
- Reduced risk of
- Colon cancer
- fragility fracture
- Increased risk of Cardiovascular disease
- The Estrogen only group in women who underwent hysterectomy showed
- Slightly increased risk of breast cancer and Coronary artery disease
- Reduced risk of fragility fracture
-
Q. What was the difference between the Women's health initiative and other earlier trials which showed the CV benefit of Menopause hormonal therapy?
- The earlier studies were observational while; the WHI was a prospective RCT
-
Q. What is the timing hypothesis?
- Subanalysis of the Women's health initiative and other studies have shown the dual nature of the CV risk in patients on Menopause hormonal therapy
- It says if the MHT is started <6 years of menopause or in younger women- there is a reduction in the CV risk
- However, if it is used later- there is increased CV risk
- The duration of therapy also has an impact- with a shorter duration of treatment <5 years- being cardioprotective
- This is the timing hypothesis
- Subanalysis of the Women's health initiative and other studies have shown the dual nature of the CV risk in patients on Menopause hormonal therapy
-
Q. In the Women's health initiative trial with the use of Estrogen and progesterone, in what conditions were an absolute increased and increased benefit-risk seen?
- Increased risk
- Coronary artery disease
- stroke
- Venous thromboembolism
- breast cancer
- Increased benefit
- Colon cancer
- Hip Fracture and any fragility fracture
- New-onset of Diabetes
- Increased risk
-
Q. In the Women's health initiative trial with the use of Estrogen only therapy in women with hysterectomy, in what conditions were an absolute increased and increased benefit-risk seen?
- Increased risk
- stroke
- Venous thromboembolism
- Increased benefit
- Colon cancer
- Hip Fracture and any fragility fracture
- New-onset of Diabetes
- Coronary artery disease
- breast cancer
- #ClinicalPearl: In the Women's health initiative study - Estrogen only therapy was associated with benefits in terms of CV risk and breast cancer compared to E +P therapy. However, the risk of stroke was retained
- Increased risk
-
Q. Despite these risks mentioned above, did the mortality increase?
- Interestingly, despite the increased risk, the all-cause mortality was NOT higher in the women treated with Hormonal therapy
- This includes both CV and Breast cancer mortality
-
Q. Does the use of estrogen improve cognition and the risk of dementia?
- Estrogen used in women >65 years did not show any improvement in reducing the risk of Dementia
- On the contrary E+P use, increased the risk of dementia
-
Q. Which estrogen and progesterone were used in the Women's health initiative trial?
- estrogen - conjugated equine estrogens (CEE) - 0.625 mg/day
- Note, this dose is much higher than that required to relieve vasomotor symptoms of menopause
- Progesterone- Medroxyprogesterone acetate - 2.5 mg/day
- estrogen - conjugated equine estrogens (CEE) - 0.625 mg/day
-
Q. Is there an increased risk of endometrial cancer with Hormonal Therapy?
- In women with a uterus, estrogen use alone increased the risk of endometrial cancer
- However, E+P therapy DOES NOT increase the risk of endometrial cancer
-
Q. What are the current broad recommendations for the use of Menopause hormonal therapy?
-
- Use it for younger women
- <60 years
- <10 years since menopause
-
- Use it for a short duration
- around 5 years
-
- Use of modern estrogen and progesterone preparation
-
- Don't use it for cardiovascular or bone protection
-
- Use mainly for vasomotor symptom relief
-
-
Q. What was the mean age of patients in the Women’s health initiative?
- 63 years
-
Q. How long can MHT continue?
- Estrogen + Progesterone - <5 years
- Estrogen alone- can used longer in hystrectomized patients
-
Q. Enlist the benefits of MHT?
- Reduced Fracture risk
- Reduced hot flushes
- Reduced vaginal dryness
- Reduced UTI
- Reduced colorectal cancer
- Reduce Osteoarthritis
- Reduced type 2 diabetes
- Reduced Coronary artery disease
-
Q. Give the harmful effects of MHT?
- Increase stroke
- Increased Breast cancer (E + P)
- Increase ovarian cancer (mild increase)
- Increase Venous thromboembolism
- Increase cholecystitis
-
Q. Give a snapshot of cancer and MHT?
- Breast cancer
- An increased risk with E + P
- Reduced with Estrogen alone
-
- Ovarian cancer
- a mildly increased risk with E + P
-
- Endometrial cancer
- An increased risk with E alone
- No increase with E + P
-
- Colorectal cancer
- Reduce risk with E + P
-
- Nonsmall cell carcinoma- reduced survival
- Breast cancer
-
Q. What is the current stature on CV risk and MHT?
- Increase CV risk seen with WHI
- However, the mean age of the patient in WHI was >60years
- In women 50-59 years, it may reduce CV risk
- Also use of Medroxyprogesterone, and Conjugated estrogen in WHI may have something to do with CV risk
- 2015 meta-analysis in women <10 years since menopause on MHT- reduce CV risk and reduce mortality
-
Q. What kind of stroke was seen in women on MHT?
- Ischemic stroke
-
Q. What type of estrogen preparation has less VTE and stroke risk?
- Transdermal estrogen
-
Q. Give the Forearm fracture paradox?
- Forearm fracture dramatically increase in women after the age of 50 years while it increases in men only after 80 years
- Mainly due to increased fall in women
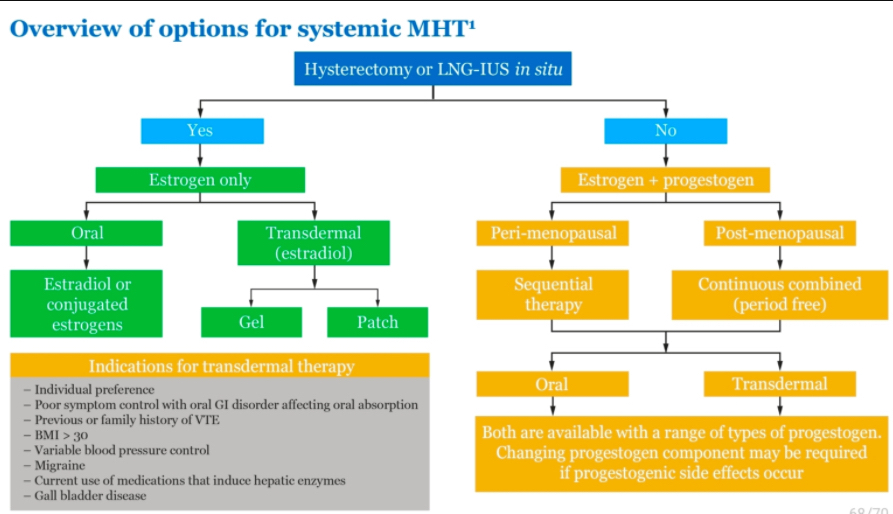
Q. What are the methods for giving Menopause hormonal therapy ?
- 
-
Q. What is the difference between continuous sequential and continuous combined therapy ?
- Continous sequential therapy
- Estrogen alone for 14 days - then next 14 days E + P
- Total 28 days cycle
- no breaks
- when the next cycle starts - the withdrawal bleeding occurs in the first few days of starting the next cycle
- Continous combined therapy
- E + P daily from day 1 to day 28
- No bleeding occurs
- useful for late menopause
- Continous sequential therapy
-
**Selective estrogen receptor modulators SERM
-
Q. Broadly speaking- what are Selective estrogen receptor modulators SERM?
- They have estrogen receptor agonist and antagonist actions in different tissues
-
Q. What are the advantages and disadvantages of using Raloxifene?
-
Advantages
- Reduces the risk of vertebral fractures
- Not significant impact on non-vertebral fractures
- CV risk-neutral
- Reduces the risk of breast cancer
- The overall risk reduction is similar to tamoxifen
- However, it has benefit in risk reduction only in ER-alpha positive breast cancer
- Reduces the risk of vertebral fractures
-
Disadvantages
- Clinical symptoms like Hot flashes and leg cramps are seen
- Does not per se increase the risk of stroke but known to increase the risk of fatal strokes
- Increases the risk of venous thromboembolism
-
Dose is 60 mg/day
-
-
Q. Tell me something about other SERM?
-
- tamoxifen
- Is reduces the risk of breast cancer
-
- Bazedoxifene
- It reduces the risk of fractures
- Also shows improvement in vasomotor symptoms and vaginal dryness and atrophy
- Neutral for breast cancer and endometrial cancer
-
- Tibolone
- It improves Vasomotor symptoms
- Also reduces the risk of vertebral fractures and non-vertebral fractures
- However, it increases the risk of stroke
-