- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
-
Video:
-
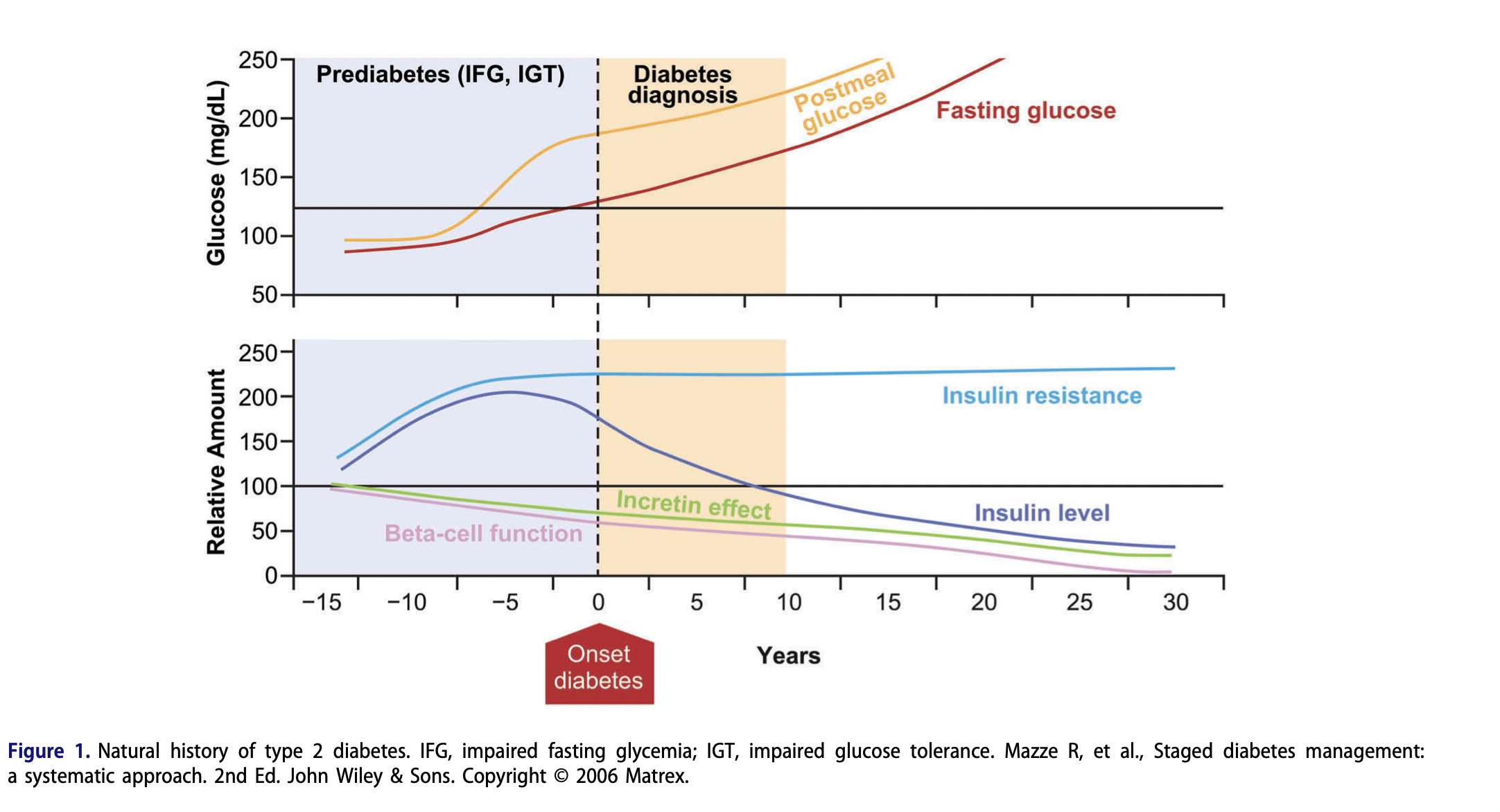
Q. Summarize the Pathogenesis of Type 2 Diabetes and its natural history with a picture ?
-
Q. How many islets of langerhans do we have and how many Beta-cells in each of them ?
- We have 1 million islets of langerhans
- Each islet has 1000 Beta-cells
-
Q. What % of Beta-cells function is lost at the time of diagnosis of Type 2 Diabetes mellitus and what % is lost every year ?
- 50% is lost at the time of diagnosis
- 4-5% reduction every year
-
Q. What does insulin output depend upon ?
- It depends upon
-
- beta-cell mass
-
- beta-cell function
-
- It depends upon
-
Q. What is the current debate in the role of Beta-cells in Type 2 diabetes ?
- The current debate is whether is there a reduction in beta-cell mass that leads to type 2 diabetes or it is reduction in beta-cell function that leads to diabetes
-
Q. Why is this debate important ?
- This is important because if there is only loss of function and not mass to potential of remission from disease is high
- However, if there is a loss of mass and less issue with function- the potential of remission over a long term is questionable
-
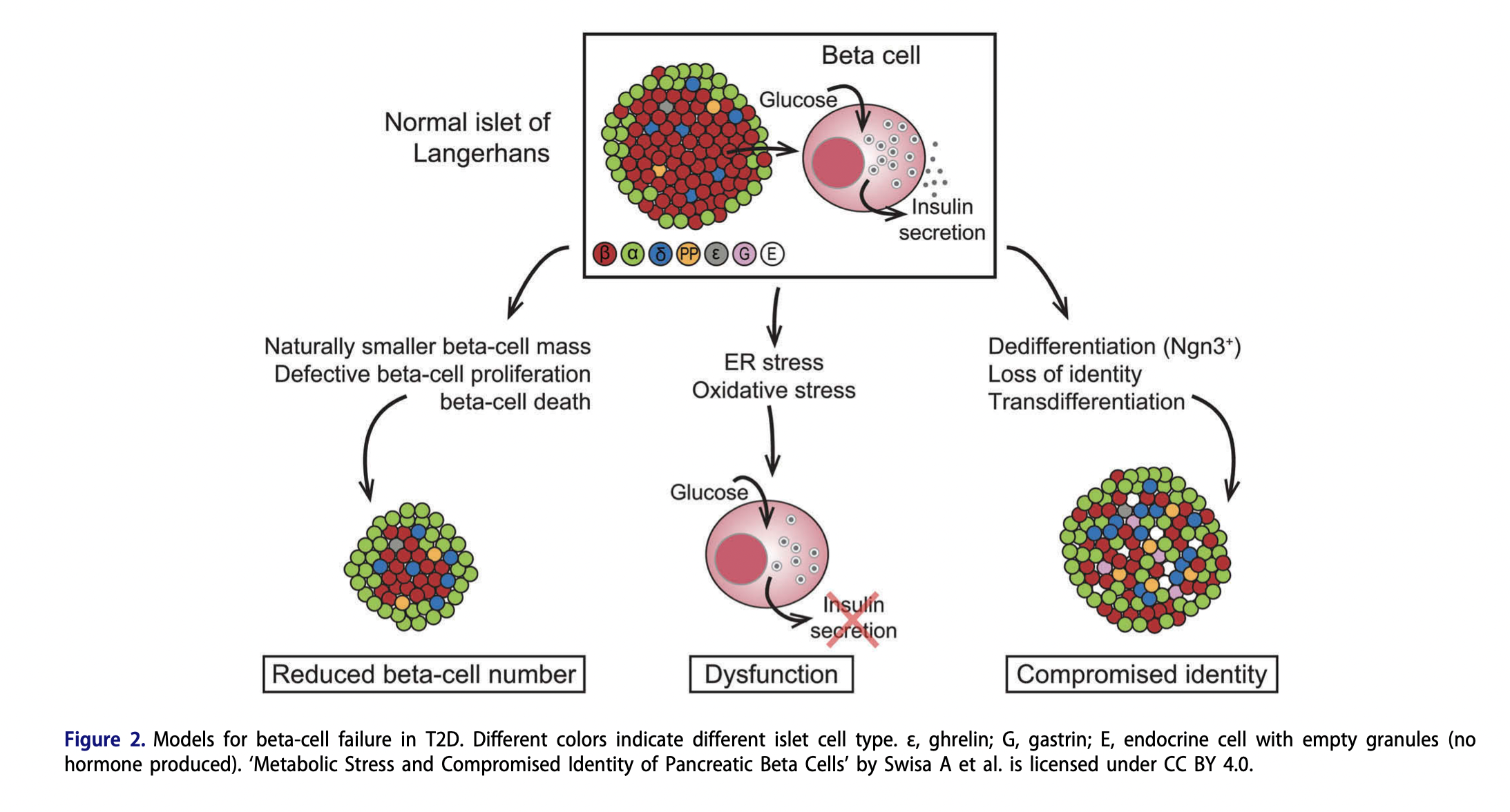
Q. What are Swisa's three models for Beta-cell failure in Type 2 Diabetes mellitus ?
-
- Reduced beta-cell number
-
- Beta-cell dysfunction due to (Also called beta-cell exhaustion )
- Endoplasmic reticulum stress
- Oxidative stress
-
- Compromised identity of Beta-cells
- or Dedifferentiation / transdifferentiation of beta-cells
-
-
Q. First model - What leads to reduction of reduced beta-cell mass ?
-
- People may have low beta-cell to begin with (Fetal programming)
-
- Beta-cell may undergo apoptosis
-
- Aging leads to decline in beta-cell mass
-
-
Q. Second model - What leads to reduced beta-cell function ?
-
- Endoplasmic reticulum stress
- Endoplasmic reticulum stress is an important cause of beta-cell loss in both type 1 and Type 2 Diabetes mellitus
-
- Oxidative stress
- This is where the phenomenon of Glucose Toxicity (Glucotoxicity) comes into picture
- This is the recoverable part of Beta-cell dysfunction
- There might be temporary stunning of beta-cells due to Hyperglycemia
-
-
Q. ER Stress and Beta-cells
-
Q. Third model - compromised identity - Transdiffertiation of Beta-cells to other cells
-
Q. Of the above two models - which is more important ?
- Model 2 is more important
- This is because reduction of beta-cell mass can be compensated by increase in beta-cell function
- A patient can have diabetes even with normal beta-cell mass
- On the contrary- increase of beta-cell mass may not always compensate for reduced beta-cell function
- This is a very important thing to understand

-
Q. According to a study, which drugs lead to how much of monotherapy failure?
- At 5 years
- Glyburide- 34%
- Metformin- 21%
- Rosiglitazone- 15%

- At 5 years
-
Q. Enlist the various tests that are useful for the Assessment of beta-cell function ( beta-cell function ) in clinical practice ?
-
- Proinsulin:Insulin ratio
-
- HOMA-Beta
-
- Mixed meal stimulation test
-
- OGTT
-
-
Q. What are the usual C-peptide in Fasting and post-meal states in euglycemic individual ?
- Fasting - 0.9-1.8 ng/ml
- Post -meal- 3-9 ng/ml
-
Q. What is the best-cutt of blood C-peptide levels to determine insulin use in a post-prandial sample ?
- 2 hour post meal- C-peptide <6 ng/dl (<2.02 nmol/l) is a stong predictor of insulin requirement
-
Q. What is the interpretation of Random C-peptide value ?
- The RBS >140 mg/dl for interpretation
- Random c-peptide
- <0.6 ng/ml ==> Absolute insulin deficiency
- <1.8 ng/ml ==> Likely Type 1
- 0.6-6.0 ng/ml ==> Requires mixed meal stimulation test
- More than 6.0 ng/ml==> Rules out Type 1

- Convert nmol/l to ng/dl by multiplying by 3