- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
-
Q. Enlist the various disorder associated with severe insulin resistance.
- Defect in insulin receptor gene
- Leperchunism- most severe
- Rabson Mendenhall syndrome – Moderate
- Type A IR syndrome – mildest- HAIR- AN syndrome
-
- Antibodies against insulin receptor
- Type B insulin receptor syndrome
- Ataxia telegectasia
- Defect in insulin receptor gene
-
- Lipodystrophic syndromes
- Congenital generalized Lipodystrophy – Bernerdenelli Seip syndrome
- Familial partial lipodystrophy – Donnigan syndrome, Koberling syndrome
- Acquired generalized lipodystrophy- Lawrence syndrome
- Acquired partial lipodystrophy- Barraqurer- Simmons syndrome
- HIV lipodystrophy
-
**Leperchaunism **
-
Q. What is the other name of this syndrome?
- Donohue syndrome
-
Q. What is the main defect in this disorder?
- There is a defect in the gene coding for insulin receptor
- Hence these patients have an absence of insulin receptor – INSR gene
-
Q. What are the clinical features?
- Short stature
- Severe insulin resistance
- Fasting Hypoglycemia and post-prandial hyperglycemia
- Growth retardation starting from intrauterine life
- Autosomal recessive
- Death by 1 year of age
- A very rare disorder
-
Q. What is the treatment?
- IGF1
-
**Rabson mendenhall syndrome **
-
Q. Tell me something about this syndrome.
- It is similar to Leperchaunism but milder
- They survive till adolescence
-
Q. What are the Clinical features of this syndrome?
- Diabetes by 5-6 years requiring high dose of insulin
- Coarse senile facies
- Dysplastic dentition
- Pineal gland hyperplasia
-
**Type A insulin resistance syndrome **
-
Q. What is Type A insulin resistance syndrome?
- This is a mutation in the insulin receptor
- Patients generally present in adolescence with features of insulin resistance and hyperandrogenism
-
Q. What is the other name of this syndrome?
- This is the one called HAIR-AN syndrome
- H- hyperandrogenism
- Insulin resistance
- Acanthosis nigricans
- Pearl
- Insulin receptor disorder
- Mildest- Type A IR syndrome
- Moderate- Rabson Mendenhall syndrome
- Severe – Leperchaunism
- This is the one called HAIR-AN syndrome
-
**Type B insulin resistance syndrome **
-
Q. What is the pathogenesis of this syndrome?
- This is due to antibodies against insulin receptors- this is called AIRA - anti-insulin receptor antibody
-
Q. What are the clinical features of this syndrome?
- Typically present in middle age females
- May have associated with other autoimmune disorders
-
Q. Will this always lead to hyperglycemia?
- No
- It can lead to hypoglycemia or hyperglycemia depending on whether the antibody is activating or blocking
-
Q. Of the two, which presentation is more common?
- Hyperglycemia is more common than hypoglycemia
-
Q. Which other syndrome is associated with antibodies against insulin receptors?
- Ataxia telegectasia
-
Q. What is the typical age of presentation?
- 30-50 years
-
Q. Is it associated with other autoimmune diseases?
- Yes
- Has been reported with SLE and other autoimmune disorders
-
Q. When is the antibody stimulatory and when is it blocking?
- At low titers the antibody tends to be stimulatory - leading to hypoglycemia
- In high titers, it tends to be blocking- leading to hyperglycemia
-
Q. Does it follow a consistent pattern?
- No
- It waxes and wanes
- Sometimes the antibody disappears leading to periods of euglycemia
-
Q. What is the characteristic biochemical signature of this disorder?
- They have insulin resistance but Triglyceride is NOT elevated
- This is the sin-quo-non of this condition
-
Q. Apart from this what are the other markers of this condition?
- Fasting insulin levels >20 mIU/l
- Lean patient requiring >3 units/kg/day
-
Q. Is the antibody available commercially?
- No
- It is done only in selected research labs
-
Q. What are the clinical features?
-
- Weight loss is typical
- They are severely catabolic during the hyperglycemic phase
-
- Acanthosis nigricans
- which improves with improvement in the disease state
-
- Hyperandrogenism
-
-
Q. When do they develop hypoglycemia?
- So they have a hypoglycemic phase and a hyperglycemic phase
- During the hyperglycemic phase- they need massive amounts of insulin- but they don't develop hypoglycemia because of that
- Hypoglycemia develops when the hyperglycemia phase resolves and it is often spontaneous
- So basically these two states are often separate- and though they can both exist in the same person- they exist at different times
- Hypoglycemia can be severe enough to cause mortality
-
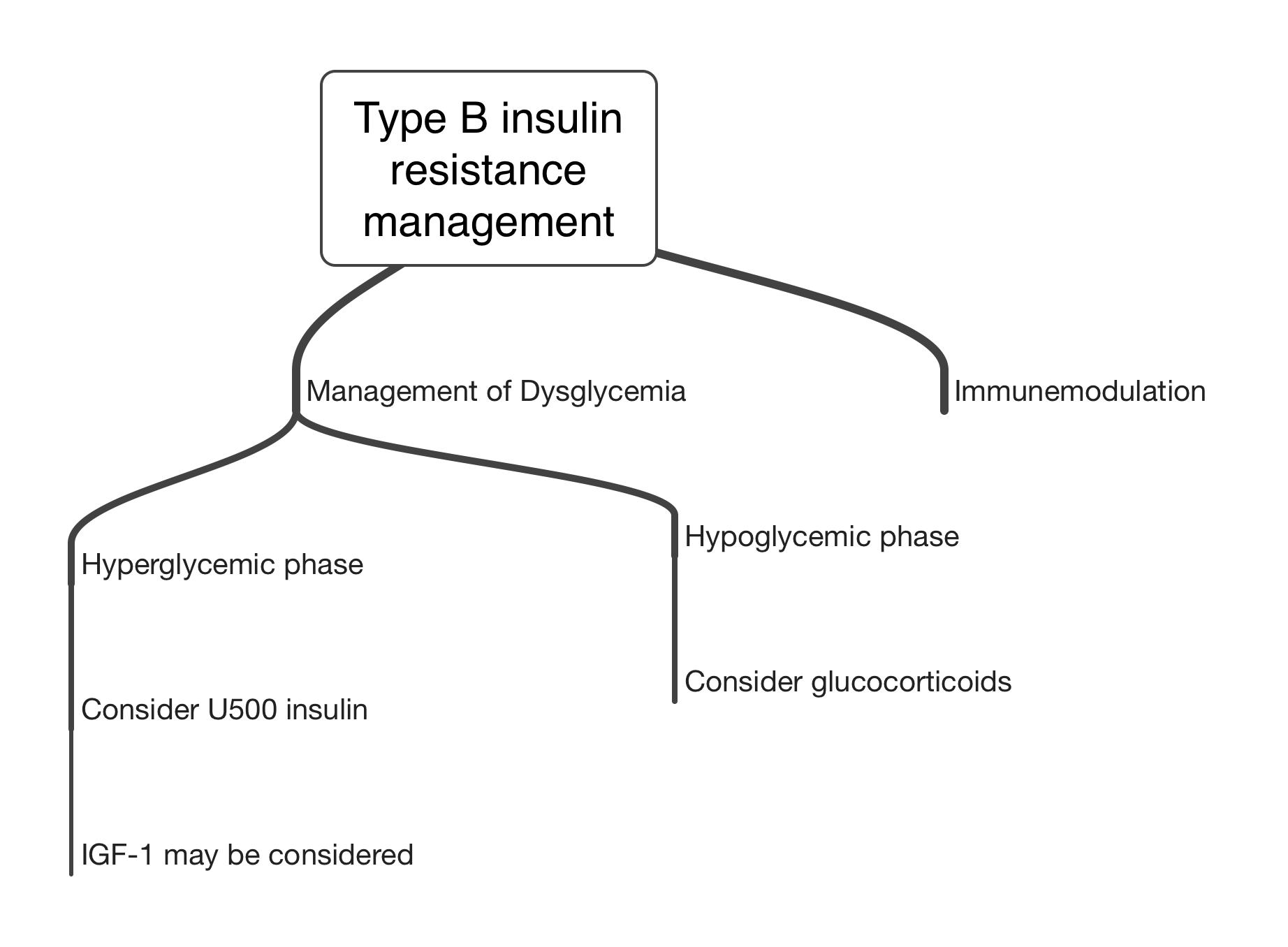
Q. What are the aspects of managing this disorder?
-
Q. How is the hyperglycemia phase managed?
- U500 or other concentrated insulin is the treatment of choice
- Try to target normal fasting glucose levels
- OAD doesn't seem to work
- Please note- achieving fasting glucose in a normal range is a sign of reducing antibodies- in this stage, they can have partial agonist action of antibodies - this can lead to hypoglycemia in the future hence it is a good time to reduce insulin doses
- IGF-1 is found to be useful for correcting hyperglycemia in anecdotal reports
-
Q. How is hypoglycemia treated?
- With glucocorticoids
-
Q. What immunomodulation therapy is recommended?
- A combination of Rituximab + high dose pulse glucocorticoids + cyclophosphamide is found to be effective
- Azathioprine is given during the maintenance phase
- Be careful when giving immunomodulation during the hyperglycemia phase- because it can reduce antibodies which can make it stimulating and produce hypoglycemia- this can be fatal