- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
Related Video lectures
- New Classification for Diabetes
- Video on Precision medicine:
Outline and Definitions
Q. Give an outline of Precision medicine in Diabetes ?
- 
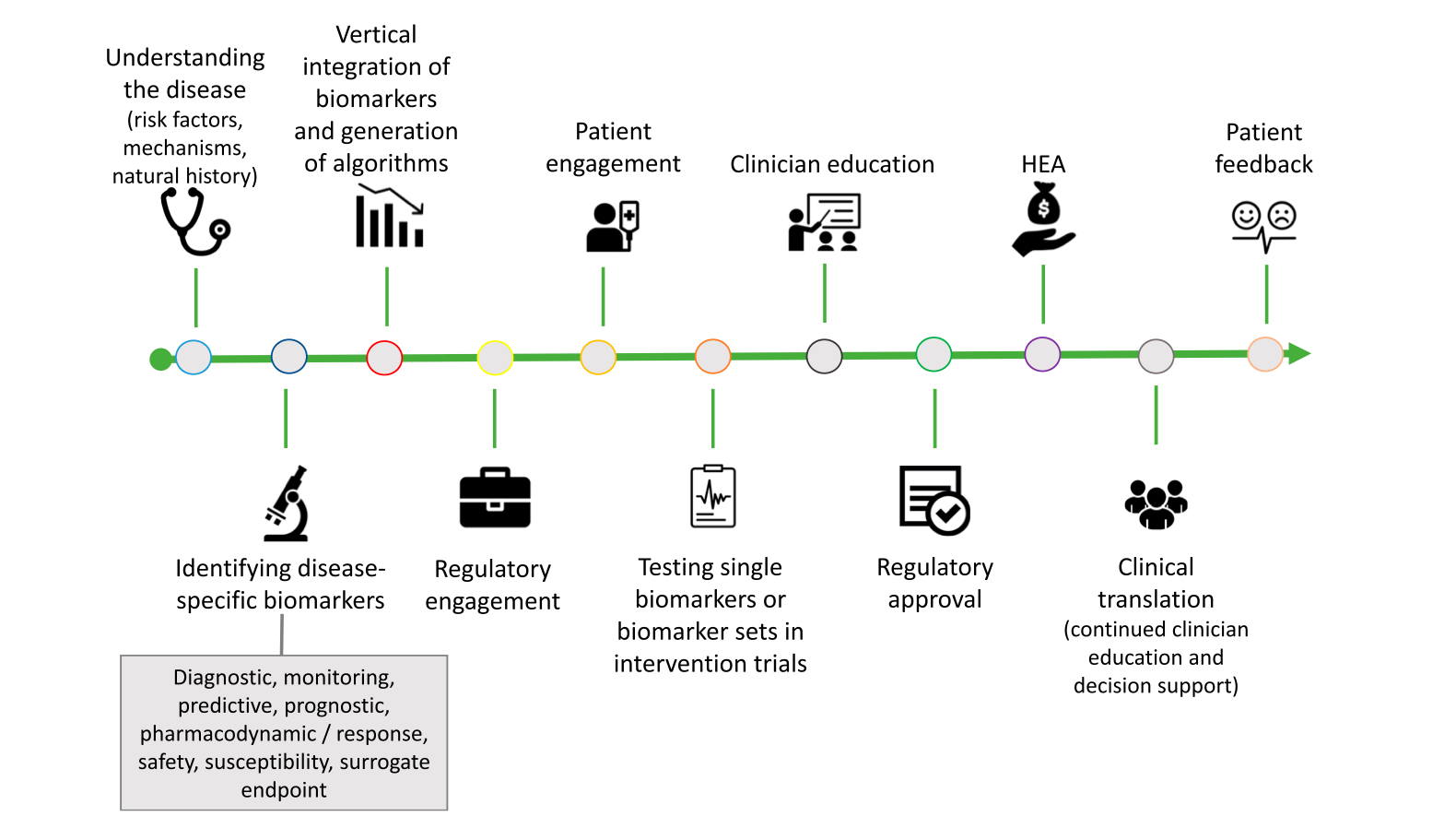
- Q. Give the pathway to precision medicine as given by the ADA ?
- Q. What is PMDI ?
- PMDI stands for Precision Medicine in Diabetes Initiative by ADA with EASD
- Mandate: Establish consensus on the viability and potential implementation of precision medicine for diagnosis, prognosis, prevention, and treatment of diabetes
- Focus: Assessing evidence, promoting research, providing education, and developing guidelines for precision medicine in diabetes
- Activities: Organizing symposia, stakeholder meetings, educational approaches, planning global clinical research network, and information dissemination
- Governance: Executive Oversight Committee, comprising representatives from founding organizations (ADA and EASD) and co-chairs of the initiative
- Steering Committee: Provides leadership and direction, currently composed of academic leaders in precision diabetes medicine from the U.S. and Europe, a representative from NIDDK, and Executive Oversight Committee members
- PMDI Task Force: Collaboration between Executive Oversight Committee and Steering Committee, working to achieve the mission of precision diabetes medicine
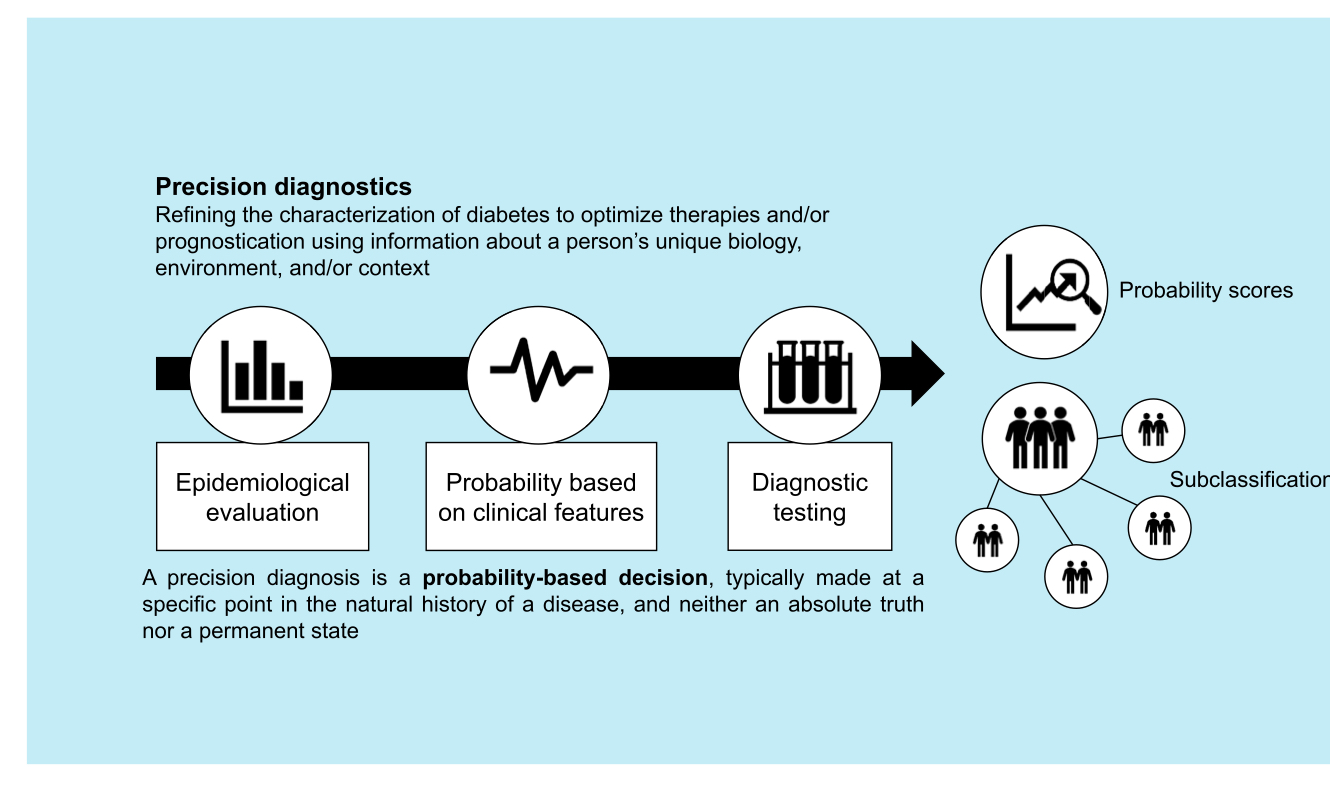
- Q. What is Precision diagnosis ?
- Involves refining the characterization of diabetes diagnosis for therapeutic optimization or improved prognostic clarity using information about a person's unique biology, environment, and/or context.
- May involve subclassifying the diagnosis into subtypes, or utilizing probabilistic algorithms that help refine a diagnosis without categorization.
- Often necessary for successful precision therapy, whether for prevention or treatment.
- Can be conceptualized as a pathway that moves through stages, rather than a single step.
- Diagnostic stages include:
-
- evaluation of prevalence based on epidemiology (e.g., age, sex, ancestry);
-
- probability based on clinical features; and
-
- diagnostic tests interpreted in the light of stages 1 and 2.
-
- A diagnosis in precision medicine is a probability-based decision, typically made at a specific point in the natural history of a disease, and neither an absolute truth nor a permanent state.
- Q. What are all the inputs into the Precision medicine in Diabetes algorithm ?
- Single gene defects: Characterization of diabetes caused by specific gene defects allows for targeted therapies
- Islet autoantibody biomarkers: These help clarify autoimmune diabetes from other forms of the disease, facilitating immune intervention trials, preonset monitoring, and detection of environmental triggers.
- Genomic risk: Assessment of individual genomic risk profiles contributes to better understanding and classification of diabetes subtypes.
- Multiple biomarkers: Identification of various biomarkers that alter the risk of type 2 diabetes (T2D) reveals new biological pathways and potential therapeutic targets.
- Genetic variants: Presence of specific genetic variants can help identify process-specific subgroups in T2D and inform the selection of optimal therapeutic approaches.
- Biological and lifestyle/environmental predictors: These factors can be used to determine the predictors of drug response and clinical outcomes.
- Public health strategies: Incorporation of population-level health strategies to address the growing diabetes burden and assess their effectiveness.
- Pharmacological therapies: Evaluation of the 12 different drug classes currently approved by the U.S. Food and Drug Administration (FDA) for diabetes treatment.
- Tools, resources, and data: Utilization of available tools, resources, and data to support the development and refinement of the precision medicine in diabetes algorithm.
- Collaboration with stakeholders: Broad stakeholder engagement, including partnerships with organizations like ADA, EASD, NIDDK, and JDRF, to ensure the successful implementation of precision diabetes medicine
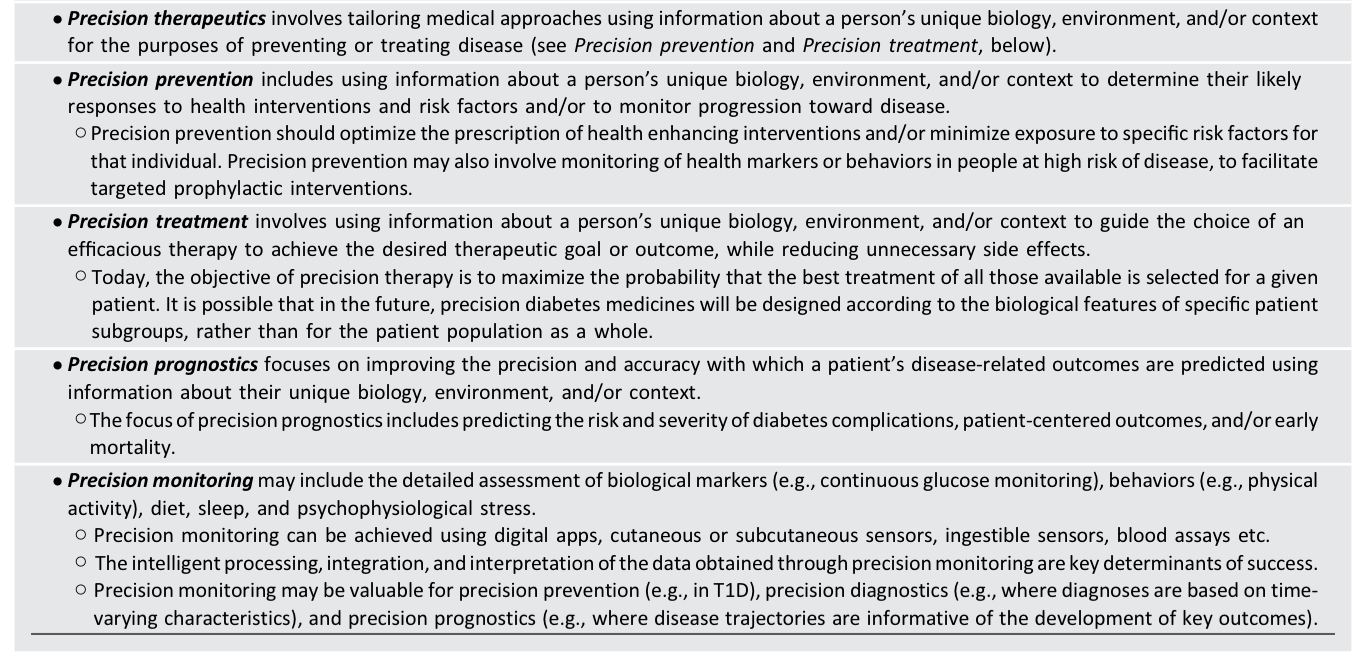
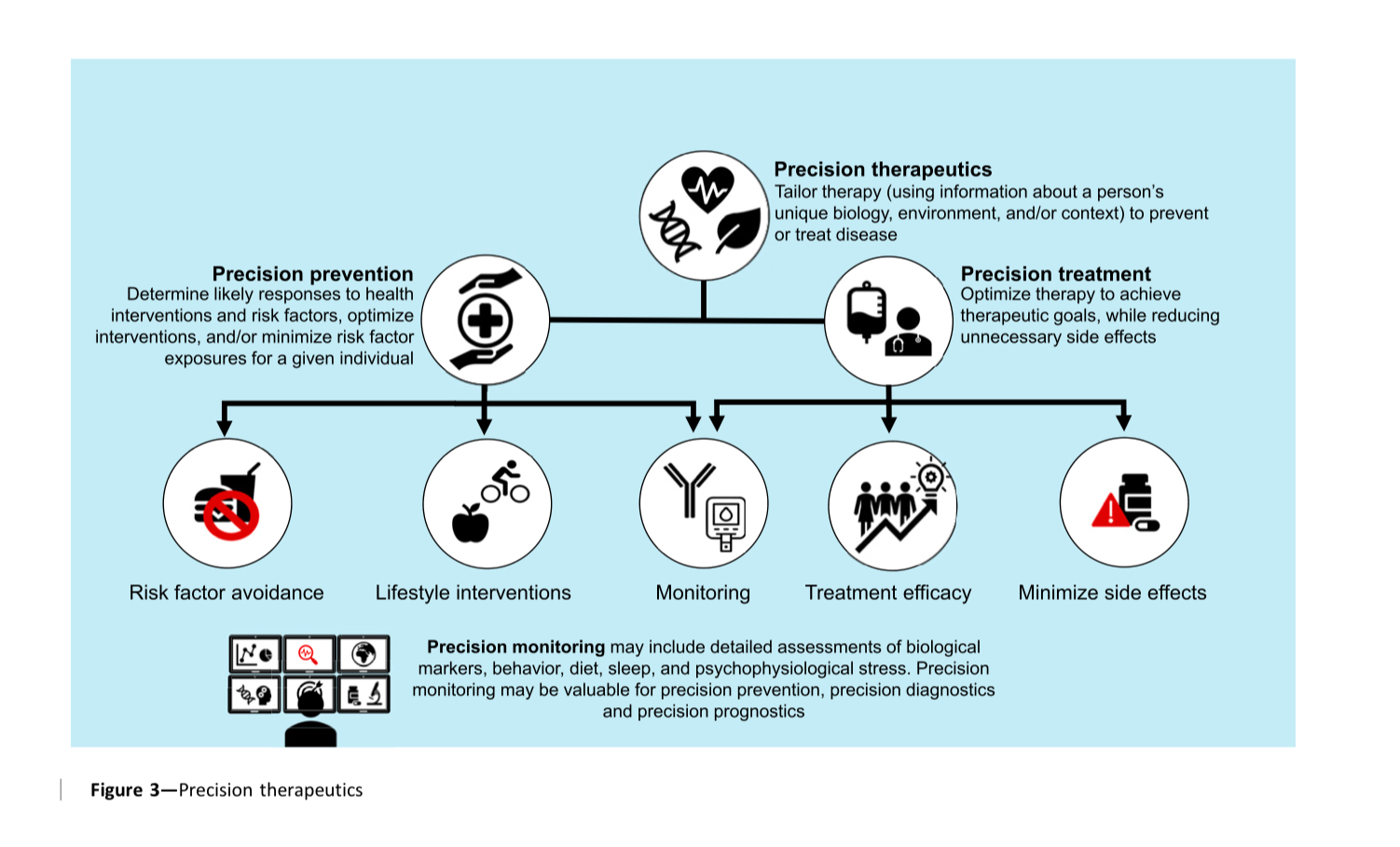
- Q. What are the various other definitions with regards to Precision medicine ?
- Q. What is Precision diagnosis ?
- It is ability to subclassify diabetes so that we can apply precision medicine to the same
- Q. What is the role of Precision diagnosis in Type 1 Diabetes ?
- It is mainly useful for prevention trials for Type 1 Diabetes ( Prediction and prevention of type 1 diabetes )
- Phenotvpes:
- • Age: Younger patients present with more severe pancreas pathology
- • Ethnicity: Risk varies according to ethnicity
- Genetics:
- Young vs. older onset: Associations with different HLA types:
- • <2 years associated with HLA-DRB10401/DQA10301/DQB1*0302 genotype
- • >6 years, associated with HLADRB10301/DQA10501/DQB1*0201 genotype
- Young vs. older onset: Associations with different HLA types:
- Metabolic/Pathologic:
- • Variability in Proinsulin processing in 3 cells
- • Variability in insulitis
- • B Cell function
- Immunology:
- •Variability in appearance of autoantibodies depending on age (<2 y: IAA; >6 y: GADA)
- Variation in the early activation of "innate immunity" and interferon signatures
- T and B cell signatures in young vs. older patients
- B cell pathology?
- Q. What are the potential subtype classification we can do for Type 1 Diabetes ?
-
- Age of the onset of the disease
-
- Age of onset of the islet autoantibody
-
- Which antibody first appears
-
- Persistence of beta-cell function and C-peptide levels
-
- Q. Is there any risk score that can predict Type 1 Diabetes ?
- Yes
- There is a T1 genetic risk score
- Q. What are the stages of Type 1 Diabetes ?
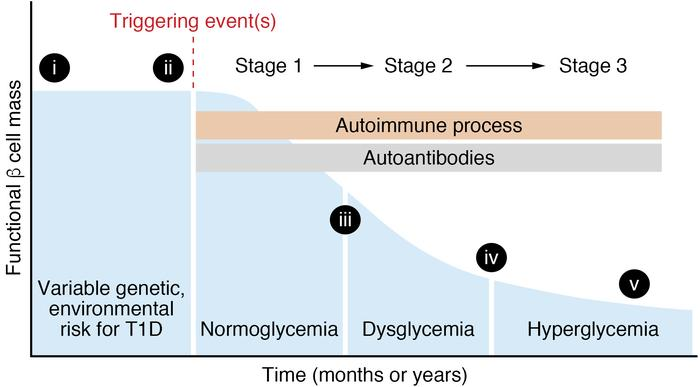
- The three stages of type 1 diabetes evolution are:
- Stage 1: autoantibodies plus normoglycemia.
- Stage 2: autoantibodies plus asymptomatic dysglycemia.
- Stage 3: autoantibodies plus symptomatic hyperglycemia.
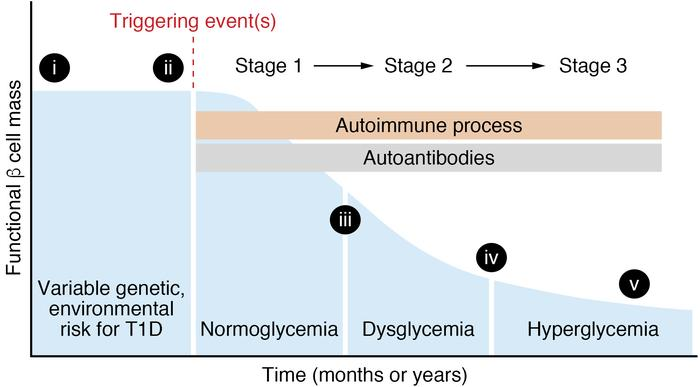
- The three stages of type 1 diabetes evolution are:
- Q. A young patient is in stage 2 of type 1 diabetes as described above. What is his lifetime risk of developing type 1 diabetes ?
- Life time risk is 100%
- Q. What about precision diagnosis in type 2 diabetes ?
- The core here is Clusters of type 2 diabetes as discussed earlier
- Q. What is the role of Precision diagnosis in interpreting Glycated hemoglobin (HbA1c) values ?
- Role of precision diagnosis in interpreting HbA1c values:
- Facilitates a more accurate assessment of blood glucose levels
- Considers factors impacting hemoglobin and red cell stability
- Takes into account genetic variants that alter HbA1c levels
- Guides interpretation of assay results based on patient's ancestry and specific genetic information
- Enables better monitoring of blood glucose levels in diabetes patients
- Role of precision diagnosis in interpreting HbA1c values:
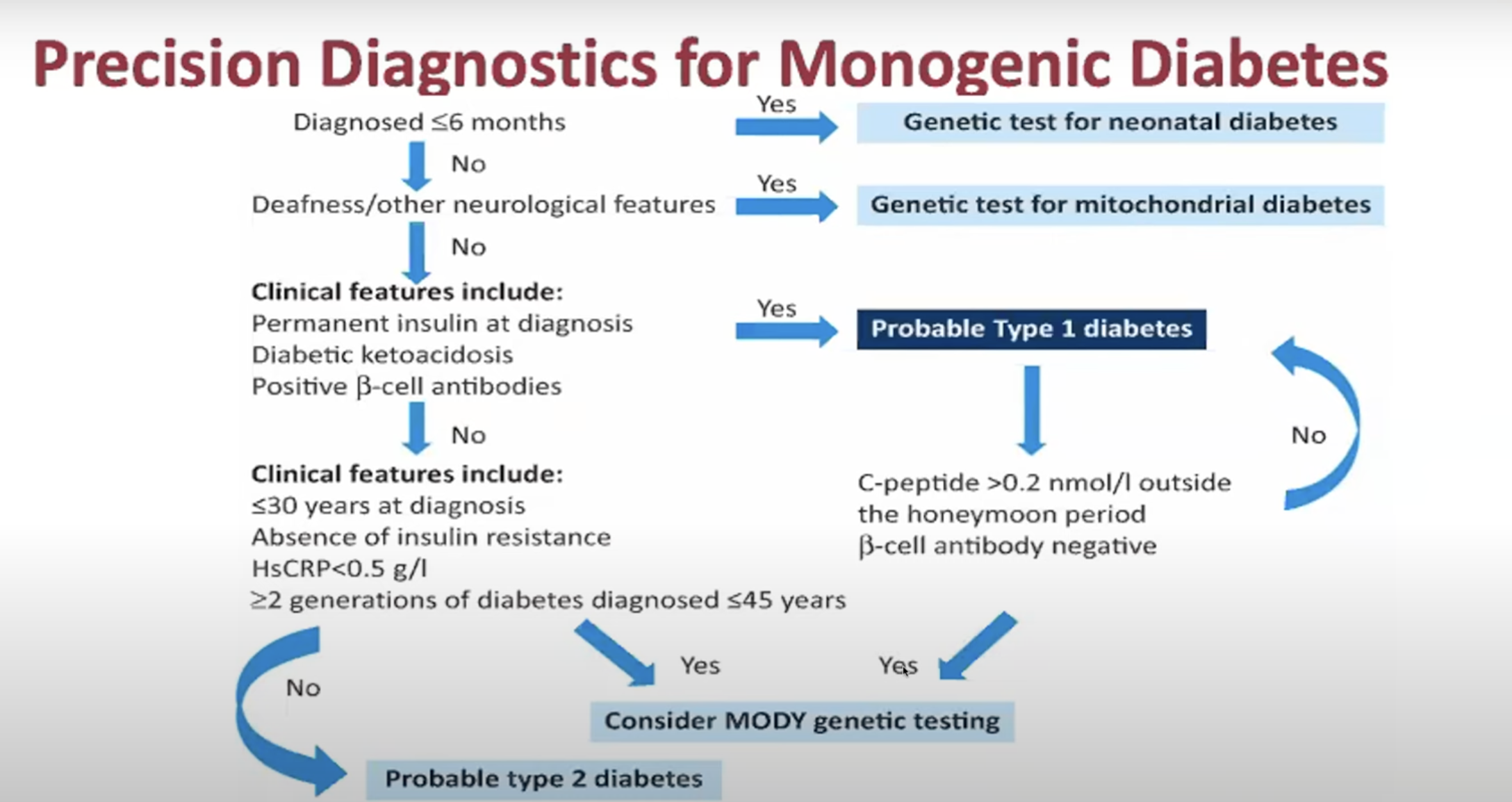
- Q. Which patients should be particularly closely screened for Monogenic diabetes
-
- Diabetes onset <6 months of age- 80% likelihood of monogenic diabetes
-
- use of MODY (Maturity onset of Diabetes of Young) calculator
-
- Pediatric diabetes with all three antibodies negative
-
- Q. Do we have an early example of Precision medicine from the ADOPT trial ?
- The trial found that men had better response to Sulphonylurea while women had better response to Thiazolidinediones
- Q. Give some examples of genetics and response to Oral antidiabetics ?
- CYP2C9 genetic variants: The 8% of the white population carrying two loss-of-function variants in CYP2C9 are 3.4 times more likely to achieve HbA1c target due to reduced metabolism of sulfonylureas and increased serum concentrations.
- SLCO1B1 and CYP2C8 genotypes: These genotypes can alter liver uptake and metabolism of rosiglitazone, resulting in a glycemic response (HbA1c) variation of as much as 0.7%.
- Q. Tell me more about the relationship of Metformin to SLC2A2 gene variations
- SLC2A2 gene: Encodes GLUT2 transporter, responsible for facilitated glucose transport across cell membranes in liver, intestines, and kidneys.
- Noncoding rs8192675 variant C allele: Associated with greater response to metformin and reduced expression of SLC2A2 transporter.
- Improved glycemic response: In individuals with obesity, two copies of the C allele showed an absolute HbA1c reduction of ~1.55% (compared to a reduction of ~1.1% in those without the C allele).
- Equivalent effect: The SLC2A2 genotype effect is similar to a difference in metformin dose of 550 mg, or about half the average effect of starting a DPP4 inhibitor.
- Q. Give the Precision medicine or Precision diagnosis algorithm for MODY (Maturity onset of Diabetes of Young) ?
Cluster classification in Type 2 Diabetes and application of precision medicine for the same
- Q. Which were the 6 variables used in the Swedish cluster by Ahlaqvist et al to subclassify patient with diabetes mellitus ?
- Ahlqvist et al used the following 6 variables in the Swedish cluster to subclassify patients with diabetes mellitus:
- Age at diagnosis
- BMI
- HbA1c
- GADA (glutamic acid decarboxylase antibodies)
- HOMA-beta
- HOMA-IR
- Ahlqvist et al used the following 6 variables in the Swedish cluster to subclassify patients with diabetes mellitus:
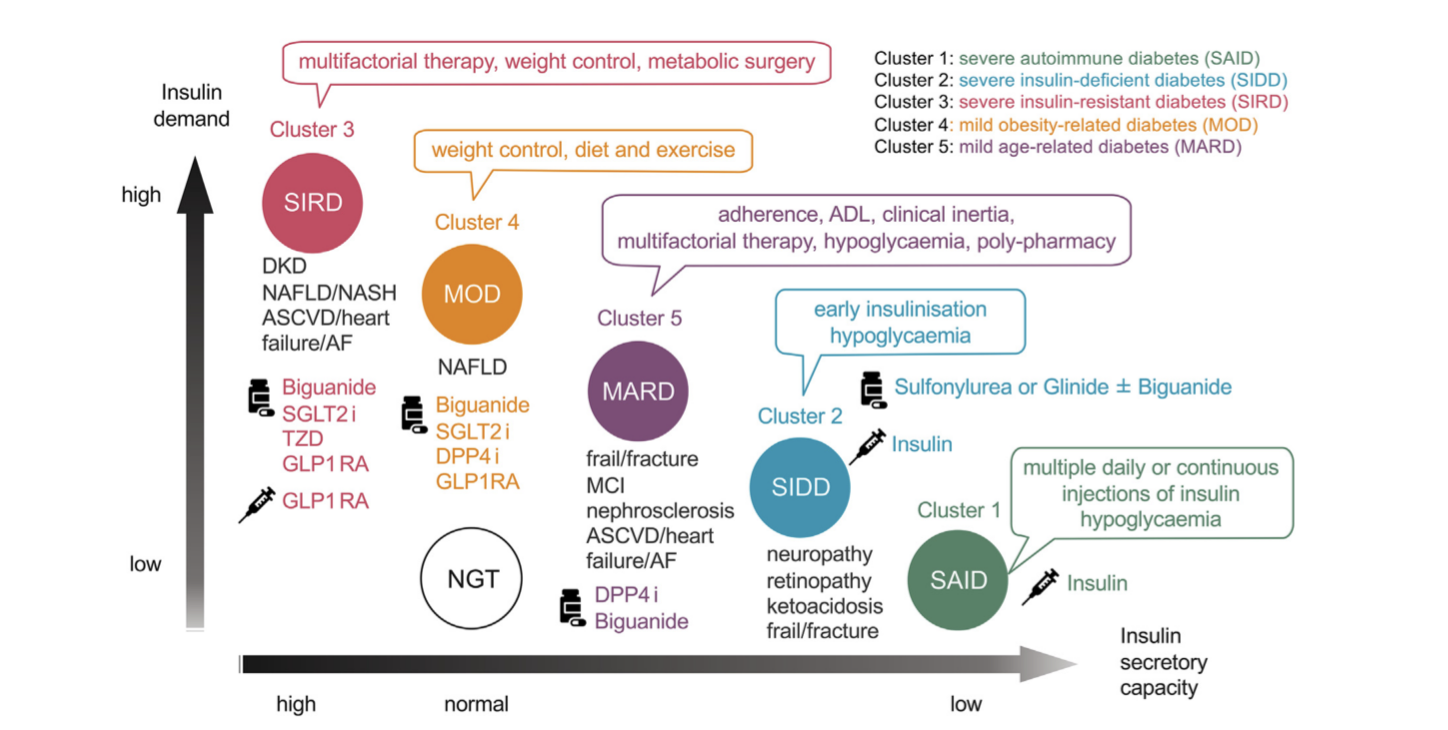
- Q. Which are the 5 clusters in the Swedish cluster ?
- Cluster 1: Severe autoimmune diabetes (SAID),
- Cluster 2: Severe insulin-deficient diabetes (SIDD),
- Cluster 3: Severe insulin-resistant diabetes (SIRD),
- Cluster 4: Mild obesity-related diabetes (MOD), and
- Cluster 5: Mild age-related diabetes (MARD).
- Q. What is a potential subclassification of Type 1 Diabetes ?
-
- Acute onset
-
- Slowly progressive (Previously called LADA)
-
- Fulminant
-
- Q. What is the alternative name suggested for LADA ?
- The alternative name suggested for LADA is SPIDDM.
- SPIDDM stands for slowly progressive type 1 insulin-dependent diabetes mellitus
- Q. What is the difference between Acute, Slowly progressive and fulminant type 1 diabetes ?
- Acute-onset type 1 diabetes (AT1DM) presents with hyperglycemic symptoms and an abolished insulin secretory capacity typically over several weeks to several months.
- Latent autoimmune diabetes in adults (LADA) or slowly progressive type 1 insulin-dependent diabetes mellitus (SPIDDM) is characterized by late age at onset, progressive beta-cell failure which is associated with an initial non-insulin-requiring state and an ultimate insulin-dependent state over several years, and persistent islet cell autoantibodies.
- Fulminant type 1 diabetes (FT1DM) is characterized by an extremely rapid process of beta-cell destruction and the progressions of hyperglycemia and ketoacidosis, showing no detectable insulin levels and severe hyperglycemia within the first week

- Q. True or false, the fulminant variant of Type 1 Diabetes have negative antibodies ?
- True
- Because the antibodies often come fast → damage and disappear rapidly
- Q. What are the three stages of type 1 diabetes ?
- The three stages of type 1 diabetes evolution are:
- Stage 1: autoantibodies plus normoglycemia.
- Stage 2: autoantibodies plus asymptomatic dysglycemia.
- Stage 3: autoantibodies plus symptomatic hyperglycemia.
- Also see Teplizumab
- The three stages of type 1 diabetes evolution are:
- Q. Give me a brief about the SAID cluster (Cluster 1) ?
- SAID cluster is defined by the presence of GADA and includes individuals with multiple autoantibodies, and it is acute-onset or LADA/SPIDDM
- It is associated with low or depleted insulin secretory capacity, low BMI, and poor glycemic control (high A1c level)
- SAID features the highest prevalence and incidence of diabetic retinopathy and a risk of fracture
- Regardless of age groups and rate of progression before symptomatic hyperglycemia, SAID is associated with a risk of ketoacidosis
- SAID nomenclature is in line with the staging of autoimmune T1DM to optimize the diagnosis and therapeutic strategy of autoimmune diabetes under the rubric of T1DM.
- Q. Which complications are maximum in the SAID cluster (Cluster 1) ?
- Diabetic retinopathy
- Fracture risk
- Diabetic ketoacidosis
- Q. How does SAID cluster (Cluster 1) differ from SIDD (Cluster 2)
- SAID - Has antibody positive
- SIDD - Has antibody negative
- Q. Are SIDD also ketosis prone ?
- Yes. They are
- Q. Give me a brief about SIDD (Cluster 2) ?
- SIDD (Severe Insulin-Deficient Diabetes) is one of the five clusters of adult-onset diabetes mellitus identified through cluster analysis.
- SIDD is characterized by severe insulin deficiency
- Patients in this cluster have a high risk of developing ketoacidosis and microvascular complications such as diabetic retinopathy and neuropathy.
- The therapeutic focus for SIDD is on insulin replacement therapy to address the severe insulin deficiency.
- Q. Give me a brief about SIRD (Cluster 3) ?
- SIRD (Cluster 3) refers to a cluster of adult-onset diabetes mellitus (T2DM) characterized by severe insulin resistance and hyperinsulinemia.
- It confers the highest risk of developing diabetic kidney disease, commonly in both Caucasians and non-Caucasians.
- SIRD may also carry the risk of cancer and dementia due to the association of insulin resistance and hyperinsulinemia with the onset and progression of these diseases.
- The frequency of SIRD is not consistent within Asians, as it was slightly lower in Japan but higher in India and China.
- Q. Which complications are higher in SIRD (Cluster 3) ?
- Diabetic kidney disease
- ASCVD
- Dementia
- Cancer
- Q. Tell me about MOD (Cluster 4) ?
- The characteristic phenotype of MOD includes mild obesity and younger age at diagnosis compared to other subtypes.
- Patients with MOD have a relatively preserved beta-cell function and moderate insulin resistance.
- MOD is associated with a lower risk of diabetic complications, such as retinopathy, diabetic kidney disease, neuropathy, and ketoacidosis, compared to other subtypes.
- Q. Finally, tell me about MARD (Cluster 5) ?
- MARD (Cluster 5) is characterized by elderly-onset diabetes with age-related decreases in insulin secretory capacity and insulin sensitivity.
- The suspected main causes of MARD are changes in body composition with decreased muscle mass and relatively increased fat mass.
- Glycemic control is good, and there were few microangiopathies.
- In elderly MARD individuals, attention should be paid to senile syndromes such as frailty syndrome, mild cognitive impairment, osteoporosis and fracture, and ASCVD. MARD is the largest cluster among Caucasians and Asians.
- Q. What are the parameters that should impact choice of medications in Type 2 Diabetes mellitus ?
-
- Age
-
- HBA1c target
-
- ASCVD
-
- Cost
-
- Side effect profile
-
- BMI
-
- Renal status
-
- Liver status
-
- hypoglycemia risk
-
- Patient preferences
-
- Q. What is the proposed treatment for SAID cluster (Cluster 1) ?
- Multiple dose insulin or insulin pump
- Q. Should patients with Latent autoimmune diabetes of Adulthood (LADA) be given insulin early on, even if they have preserved Beta-cells function ?
- Yes, patients with LADA should be given insulin early on, even if they have preserved beta-cell function. This is because LADA is a slowly progressive autoimmune disease that eventually leads to beta-cell destruction and insulin deficiency. Early insulin therapy has been shown to preserve beta-cell function and improve glycemic control in LADA patients.
- Q. What is the suggested treatment for SIDD (Cluster 2) ?
- Mild beta-cell dysfunction- Secreatgogues, DPP-IV inhibitors etc might work
- Severe beta-cell dysfunction - Insulin, often MDI
- Metformin monotherapy does not work in these cases
- Q. What is the treatment for SIRD (Cluster 3) ?
- Suggested medications:
- Metformin
- SGLT2i - known to reduce viceral and ectopic fat
- Pioglitazone
- GLP-1 receptor agonist
- Medications to avoid
- Sulphonylurea
- insulin
- Suggested medications:
- Q. What is the treatment for MOD (Cluster 4) ?
- First choice- metformin
- Others
- SGLT2i
- GLP-1 receptor agonist
- Medications to avoid
- Sulphonylurea
- Q. What is the treatment for MARD (Cluster 5) ?
- Metformin
- DPP-4 inhibitors
- Q. Summarize the treatment for various diabetes clusters
- SAID cluster (Cluster 1) - MDI (Multiple daily insulin)
- SIDD (Cluster 2) - Sulphonylurea , insulin
- SIRD (Cluster 3) - Metformin, SGLT2i, GLP1RA, Pioglitazone
- MOD (Cluster 4) - Metformin, SGLT2i, GLP1RA
- MARD (Cluster 5) - Metformin, DPP-4 inhibitors
- Q. What are the 5 steps to precision medicine as suggested by this article ?
-
- Estimate pathophysiology and Cluster
-
- Determine optimized HBA1c target
-
- Set optimal body weight targets
-
- Lifestyle measured
-
- Select class of antidiabetics based on above

-
- Q. What are the potential complications in each of the clusters as per the article ?
- SAID cluster (Cluster 1) and SIDD (Cluster 2)
- Diabetic ketoacidosis
- Hypoglycemia
- Retinopathy
- Neuropathy
- Fracture risk
- SIRD (Cluster 3)
- Diabetic Nephropathy
- ASCVD
- NASH/NAFLD
- Heart failure
- atrial fibrillation
- MOD (Cluster 4)
- NAFLD
- MARD (Cluster 5)
- Fracture
- Mild cognitive impairement
- Hypoglycemia
- ASCVD
- Heart failure
- atrial fibrillation
- SAID cluster (Cluster 1) and SIDD (Cluster 2)
- Q. Tell me something about Fetuin-A ?
- Fetuin-A is a protein that acts as an endogenous ligand of TLR4 (Toll-like receptor 4).
- It promotes lipid-induced insulin resistance.
- Fetuin-A has been shown to be involved in the development of non-alcoholic fatty liver disease (NAFLD) and its associated cardiometabolic consequences.
- It is considered as one of the hepatokines, which are proteins secreted by the liver that affect metabolism and insulin sensitivity.
- More details on Fetuin-A
- Fetuin-A is a novel hepatokine. The number of biologic roles attributed to fetuin-A has increased exponentially in the past decade.
- Fetuin-A is the endogenous ligand for Toll-like receptor-4 activation, for lipid-induced insulin resistance. Fetuin-A has inverse interaction with adiponectin. Increased fetuin-A is a risk factor for diabetes and fatty liver disease in normoglycemia and prediabetes
- Decreased fetuin-A predicts increased disease activity in obstructive lung disease, Crohn's disease, and ulcerative colitis. Both elevated and reduced fetuin-A may be linked with increased cardiovascular events.
- As a proinflammatory molecule, fetuin-A contributes to insulin resistance and is an important link between liver, adipose tissue, and muscles
- Fetuin-A is neuroprotective and plays an important antiinflammatory role in sepsis and autoimmune disorders
- Q. Regarding the MARD (Cluster 5) , which agent has the highest and the lowest risk of dementia ?
- Insulin - highest risk
- DPP-4 - lowest risk
References:
- Chung WK, Erion K, Florez JC, Hattersley AT, Hivert MF, Lee CG, McCarthy MI, Nolan JJ, Norris JM, Pearson ER, Philipson L, McElvaine AT, Cefalu WT, Rich SS, Franks PW. Precision Medicine in Diabetes: A Consensus Report From the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020 Jul;43(7):1617-1635. doi: 10.2337/dci20-0022. PMID: 32561617; PMCID: PMC7305007
- Tanabe H, Masuzaki H, Shimabukuro M. Novel strategies for glycaemic control and preventing diabetic complications applying the clustering-based classification of adult-onset diabetes mellitus: A perspective. Diabetes Research and Clinical Practice. 2021; 180:109067. DOI: 10.1016/j.diabres.2021.109067