- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Authors note
The recommendation given below is based on the evidence for in-hospital hyperglycemia management available before the COVID-19 pandemic onset, data generated from other centers during the pandemic, research of the author himself and experience of the author during the pandemic. Though backed by research, the below mentioned guideline should be treated mainly as "Expert opinion" and it is not suggested to be any official guideline on behalf of any organization. This is pure experience sharing.
Infographic
-
Q. Give an outline for in-patient management of diabetes in patients with COVID-19
- We will divide the management of COVID-19 in Diabetes into the following criteria
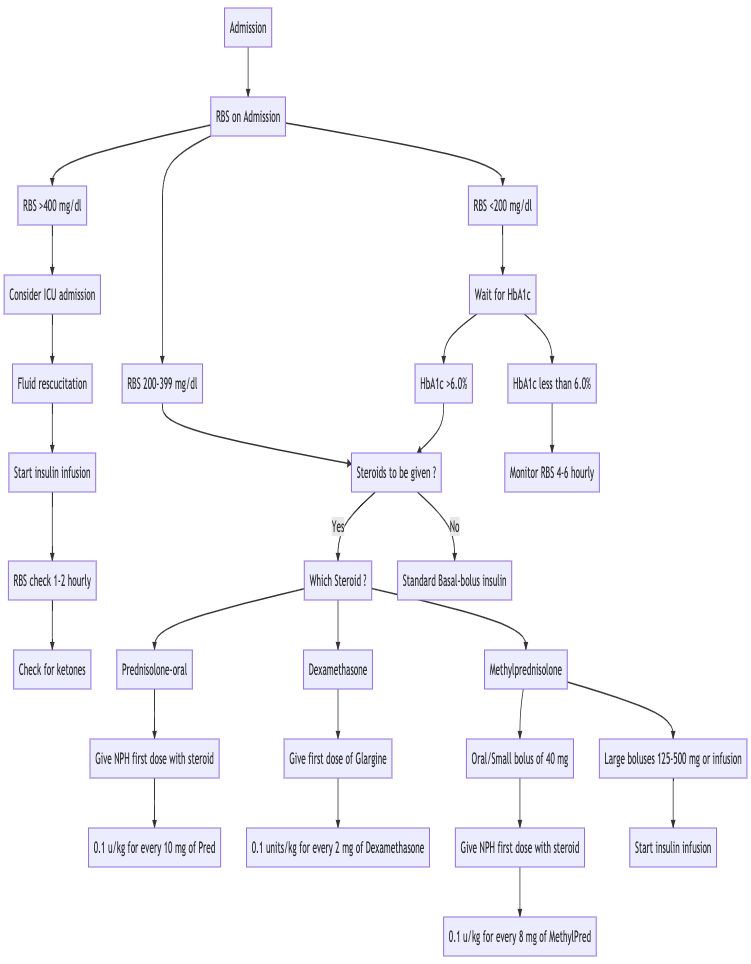
- a) Initial management (First-hour management)
- b) Continuation phase
- c) Discharge planning
- We will divide the management of COVID-19 in Diabetes into the following criteria
Initial management (First-hour management)
-
Q. Give the stepwise management of indoor patients with COVID-19 and Diabetes in the initial period (First-hour management)
-
(The recommendation to use various specific insulin with the specific steroid is based on the RCT by Lakhani et al [1]
Continuation phase
-
Q. Describe the management for a patient on Insulin infusion during the continuation period
- We typically prepare the insulin infusion rate as follows:
- 50 units of Regular human Insulin in 50 ml of Normal saline given via infusion pump.
- The starting rate is approximately the Random sugar on admission divided by 100 in ml/hr (Typographical error - thank Dr. Girish from Cochin for correction)
- For an example of the Random blood sugar on admission is 400 mg/dl- the infusion rare is set at 4 ml/hr
- The rate of infusion is adjusted based on available critical care protocol. If no in-house protocol is available, you can consider using Yale Protocol or Duke Protocol for the same. You can also consider using the app Insulin IP calc (https://play.google.com/store/apps/details?id=com.encodenet.insulin_ip_calc&hl=en_IN&gl=US) for adjusting the insulin infusion rare
- The random sugars are measured every 2 hourly, and the insulin infusion rate is adjusted accordingly
- The rate of fall of glucose is typically capped at 30-50 mg/dl per hour. If the rate of fall is faster, it is imperative to slow the insulin infusion and vice versa if the rate of fall is slower
- Additional basal Insulin may or may not be given if required. The insulin infusion acts as a basal of its own. However, basal Insulin is helpful in a limited resource set-up where the infusion can be tapered off over a period of time to reduce the burden on the hospital staff.
- Short-acting/rapid/ultra-rapid insulin may be given before meals in addition to the basal insulin/insulin infusion before meals if the patient is able to take orally as a bolus.
- In this group of patients, we typically target a random sugar value of 140-180 mg/d. [2]
- We typically prepare the insulin infusion rate as follows:
-
Q. We have limited resources, and we cannot spare a nursing staff to check Random sugars every 2 hours, what can we do?
- There is no simple solution to this, but here is a practical recommendation
- Start the infusion and check the rate of fall of glucose after 1 hour. Calculate how much time would it take to reach a target of 200 mg/dl depending on the rate of fall of the glucose
- When to recheck: (Current glucose - 200/)rate of fall
- Example
- For example, if the patient's initial glucose was 400 mg/dl. After 1 hour, it was 360 mg/dl, to the rate of fall is 40 mg/dl/hour
- Our target for this is 200 mg/dl; hence using the above formula, the patient would reach there after 4 hours- so order the next glucose check after 4 hours.
- Once the target of 200 mg/dl or below is achieved, give Basal Insulin calculated as follows:
- Calculate the Insulin given in the last 4 hours (Infusion + bolus if any)
- Extrapolate this to 24 hours. Let this value be X
- 80% of X would be the total insulin requirement (approximate). To this be Y
- 50% of Y would be the basal, which you would give stat
- Discontinue infusion 2 hours after giving the basal Insulin
- Recheck glucose 4 hours after stopping the infusion and then check sugars before meals and bedtime
- 50% of Y would be the total bolus dose. This divided by 3 would be the bolus doses to be given before meals (provided patient is taking orally)
- Additional correction bolus doses may be given based on the pre-meal glucose values
- For example
- In our above case, the patient achieved glucose of 200 mg/dl after 4 hours
- In the last 4 hours patient received 16 units of Insulin. Over 24 hours, this comes to 64 units - 80% of this would be around 50 units
- 25 units of Basal insulin glargine (1/2 of above) is given stat subcutaneous and the infusion is stopped after 2 hours. (The rate of infusion may be lowered)
- 25 units would be bolus total- to approximately 8 units before breakfast, lunch, and dinner of bolus, plus correctional doses depending on the glucose values before meals
- Start the infusion and check the rate of fall of glucose after 1 hour. Calculate how much time would it take to reach a target of 200 mg/dl depending on the rate of fall of the glucose
- There is no simple solution to this, but here is a practical recommendation
-
Q. How do you manage the continuation phase of patients on steroids with RBS of 200-399 mg/dl at the time of admission?
- Remember the first dose of Insulin has already been given with the steroids
- Now, the sugars are checked 4 times- before meals and bedtime
- Additional doses of Short-acting bolus insulin are given before meals. The following scale may be helpful, but it is better to use clinical judgment since the scale may not be applicable for all patients [3]
- <100 - nil
- 101-140 - 4 units
- 141-180 - 6 units
- 181-220 - 8 units
- 221-260- 10 units
- 261-300 - 12 units
- 301-340- 14 units
- 341-380- 16 units
- 381-420 - 18 units
- More than 420 - 20 units + consider starting infusion
- Additional doses of Insulin as described above may be added if additional steroid doses are given [4]
- Bolus / Oral MethylPred or Oral Prednisolone- give NPH
- Oral/IV dexamethasone - give Glargine
- Check the next day's morning fasting glucose [5]
- If Fasting glucose >140 mg/dl- consider adding fixed dose glargine in the evening in addition to the Insulin given with the steroids.
- Typical dose of glargine to start would be
- (FBS-40)/10
- Example
- If the patients fasting glucose is 160 mg/dl the next day
- Based on the above formula, we add 12 units of glargine subcutaneous at 7 pm.
- The dose of the glargine can be then adjusted based on the next day's morning fasting glucose value
- If the fasting glucose >140 mg/dl the next day- consider increasing the dose of the glargine by 2-4 units
In the last few weeks we have found that NPH given in the morning is also very useful even for patients on Dexamethasone. We have discssed this in the case given at the end
-
Q. Can I give oral antidiabetics during this continuation phase?
- The use of oral antidiabetics (OAD) in hospitalized patients is controversial and should be used with extreme caution
- However, the unique challenges in COVID-19 management poses a unique situation where the use of OAD can reduce the insulin dose requirement and reduce glycemic variability, provided it is used judiciously and with extreme care.
- Broadly, we suggest some gross recommendations on which OAD can be used and which should be avoided. Please note, this is based on expert opinion alone
- It is suggested to avoid OAD altogether in patients with critical illness and/or on ventilatory support
-
Q. Which OAD can be considered for use in non-critically ill patients with COVID-19 having extreme hyperglycemia?
- DPP-IV inhibitor
- Alpha-glucosidase inhibitors (AGI)
-
Q. What are the pros can con of the use of DPP-IV inhibitors in these groups of people?
- DPP-IV inhibitors are relatively safe in a broad set of conditions
- Several trials now exist for the safety of the use of DPP-IV in hospitalized patients [6]
- Amongst the DPP-IV inhibitors, linagliptin and teneligliptin do not require dose adjustment as per the eGFR. The other gliptins may require renal dose adjustment
- They are safe to use in a broad set of clinical conditions without any significant concern for safety
- They must be avoided in patients with a current or past history of pancreatitis
-
Q. What about AGI?
- Just like DPP-IV inhibitors, AGIs, especially acarbose, is safe and valuable in hospitalized patients
- They blunt the peak of the post-prandial sugars and are particularly useful in patients with steroid-induced hyperglycemia
- They must be avoided in patients having severe gastroparesis
-
Q. Which OAD are to be avoided?
- Sulphonylureas (SU)
- Metformin
- Thiazolidinediones (TZD)
- SGLT2 inhibitors
-
Q. Why should SU be avoided in these patients?
- Though SU can help in the rapid control of glycemia in certain patients; it is hazardous to use SU in patients with unstable glycemia when hospitalized, especially when they are on steroids
- The change in dose of steroids and/or clinical circumstance can make the patient vulnerable to develop hypoglycemia
- With longer-acting SU, the hypoglycemia may often be prolonged and potentially life-threatening
- It is best avoided in hospitalized patients
-
Q. What about metformin?
- Metformin is generally contraindicated in patients with severe hypoxia because of the potential risk of lactic acidosis
- Though lactic acidosis is very rare, the very nature of COVID-19 makes the patient vulnerable to the same.
- Hence in most circumstances, it is best to avoid metformin in hospitalized patients
-
Q. What about SGLT2 inhibitors?
- It is very dangerous to give SGLT2 inhibitors in hospitalized patients
- They can potentially trigger euglycemic ketosis in patients who are having relative or absolute insulin deficiency
- The risk of developing UTI in these patients is also high
- The risk of dehydration and hence potentially triggering risk of venous thrombosis should be kept in mind
- All-in-all it is best to avoid SGLT2 inhibitors in this group of patients
-
Q. What about Thiazolidinones (TZD)?
- Thiazolidinediones (TZD) have a slow onset of its action and hence not helpful in acute hyperglycemia situation
- They can cause fluid retention and hence best avoided in this circumstance
-
Q. What about the use of GLP1 receptor agonists?
- Use have found the use of GLP1 receptor agonists extremely fruitful inpatient with COVID-19 and hyperglycemia when used in selected patients
- They cut the peak of hyperglycemia much faster compared to other agents because of their higher relative potency without increasing the risk of hypoglycemia
- The only downside is that they can cause GI disturbances and must be avoided in patients with gastroparesis
- However, in our experience, the use of a small dose of GLP1 receptor agonist (like Liraglutide 0.6 mg) does not produce significant GI disturbances, and it is instrumental in blunting the peak, especially in steroid-induced hyperglycemia
- They are handy since they do not produce hypoglycemia
- Some trials for the use of Liraglutide use in hospitalized patients shown it to be safe and effective in this subset of patients. [7]
Sample prescription for patient in the ward with glucose values of 200-399 mg/dl
Patient on Multiple doses of Methylprednisolone or singl or multiple doses of Dexamethasone
When cost is NOT a constraint:
- inj LANTUS 24 units (as a starting dose) at 7 pm
- inj NPH 12 units before breakfast (ideally with the morning steroid dose)
- inj FIASP before meals (before breakfast, lunch and dinner) as per the glucose values
- inj VICTOZA 0.6 mg before lunch / T. SITAGLIPTIN (JANUVIA/ISTAVEL) 100 mg before lunch
- T. GLUCOBAY 50 mg 1-1-1 three times before meals
RBS check atleast 4 times
- Before breakfast
- Before lunch
- Before dinner
- Bedtime
inj FIASP given as per the glucose value
Dose of Glargine adjusted based on steroid dose and morning fasting glucose value
Dose of NPH adjusted as per the predinner glucose and the steroid given
For low resource settings:
- inj NPH 30 units (as a starting dose) at 7 pm
- inj NPH 12 units before breakfast (ideally with the morning steroid dose)
- inj Regular human insulin before meals (before breakfast, lunch and dinner) as per the glucose values
- DPP-IV inhibitors
- T. Voglibose 0.3 mg three times before meals
RBS check atleast 4 times
- Before breakfast
- Before lunch
- Before dinner
- Bedtime
inj Regular human insulin given as per the glucose value
Dose of evening NPH adjusted based on steroid dose and morning fasting glucose value
Dose of morning NPH adjusted as per the predinner glucose and the steroid given
Patient on morning Prednisolone / Methylprednisolone ONLY
When cost is NOT a constraint:
- inj NPH 12 units with the morning Prednisolone/Methylpred
- inj LANTUS 16 units at 7 pm (as initial dose when the fasting glucose value is >200 mg/dl) ==> be very careful of this dose as the glucose toxicity starts reducing else the patient will start developing morning hypoglycemia
-
- inj FIASP before meals (before breakfast, lunch and dinner) as per the glucose values
- inj VICTOZA 0.6 mg before lunch / / T. SITAGLIPTIN (JANUVIA/ISTAVEL) 100 mg before lunch
- T. GLUCOBAY 50 mg 1-1-1 three times before meals
RBS check atleast 4 times
- Before breakfast
- Before lunch
- Before dinner
- Bedtime
inj FIASP given as per the glucose value
Dose of Glargine adjusted based on steroid dose and morning fasting glucose value
Dose of NPH adjusted as per the predinner glucose and the steroid given
For low resource settings:
- inj NPH 12 units with the morning Prednisolone/Methylpred
- inj NPH 20 units at 7 pm (as initial dose when the fasting glucose value is >200 mg/dl) ==> be very careful of this dose as the glucose toxicity starts reducing else the patient will start developing morning hypoglycemia
-
- inj FIASP before meals (before breakfast, lunch and dinner) as per the glucose values
- inj Regular human insulin before meals (before breakfast, lunch and dinner) as per the glucose values
- DPP-IV inhibitors
- T. Voglibose 0.3 mg three times before meals
RBS check atleast 4 times
- Before breakfast
- Before lunch
- Before dinner
- Bedtime
inj Regular human insulin given as per the glucose value
Dose of evening NPH adjusted based on steroid dose and morning fasting glucose value
Dose of morning NPH adjusted as per the predinner glucose and the steroid given
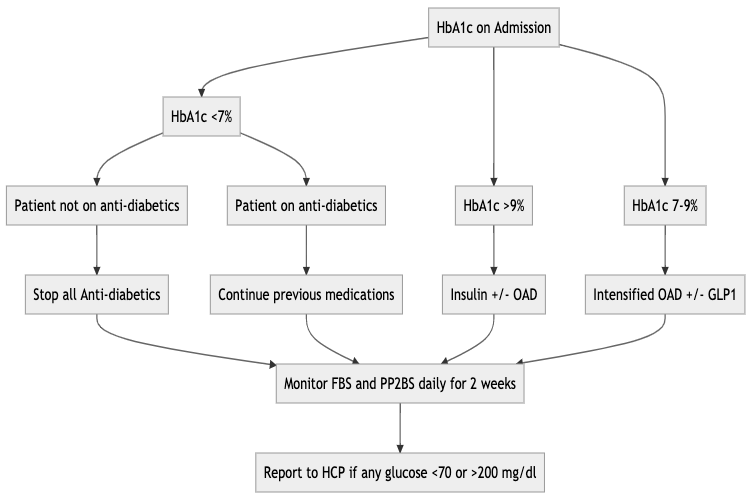
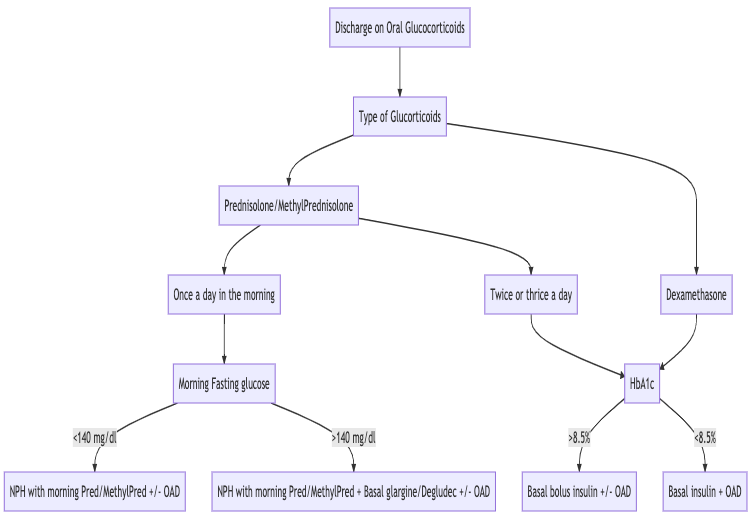
Discharge planning
-
Q. What should be kept in mind while planning to discharge the patient?
-
- Was the patient having pre-existing Diabetes or having steroid and/or COVID-19 induced hyperglycemia?
- If the patient was already on anti-diabetics before admission- consider as Pre-existing Diabetes
- If the HbA1c ≥6.5% before admission, consider having pre-existing Diabetes
-
- Are steroids to be continued at the time of discharge? If yes, what dose and duration?
- See the flow chart below
-
-
Q. What should be the protocol for management at the time of discharge if the steroids are to be discontinued at the time of discharge?
-
Q. What should be the protocol for management at the time of discharge if the steroids are to be continued?
-
Q. When should we typically ask the patient to follow up?
- We typically ask the patient to follow up 2 weeks post-discharge as the initial first follow-up
An example
A 65 year old male, with HbA1c with 8.5 is admitted with COVID19 with pulmonary involvement. On Admission his RBS was 465 mg/dl. He was to be started on Dexamethsone by the pulmonologist. (ketosis ruled out)
We started the patient on Insulin infusion with glucose check every 2 hours. Along with this we gave the first dose of glargine on the very day.
The next day we saw the patient in the ward, the morning glucose value was 185 mg/dl. The dose of glargine was adjusted, inj NPH was added in the morning. We added Acarbose three times a day before meals and Liraglutide 0.6 mg before lunch, along with short acting insulin FIASP (fasting acting aspart) before meals (dose adjusted as per the glucose value). Infusion was eventually discontinued the same day within a few hours after overlap with subcutenous insulin
Now as we go along, we would titrate the morning NPH dose based on the evening pre-dinner glucose values and the glargine based on the fasting glucose value.
On Day 3, the patient had excellent glycemic control. Now as the dose of steroid was reduced (or if the steroid was changed) the dose of glargine and NPH were adjusted as per the changes in the doses of the glucocorticoids.
Contrary to popular beliefs the Liraglutide and the OAD were very well tolerated. (However, all patients may not afford liraglutide considering the cost)
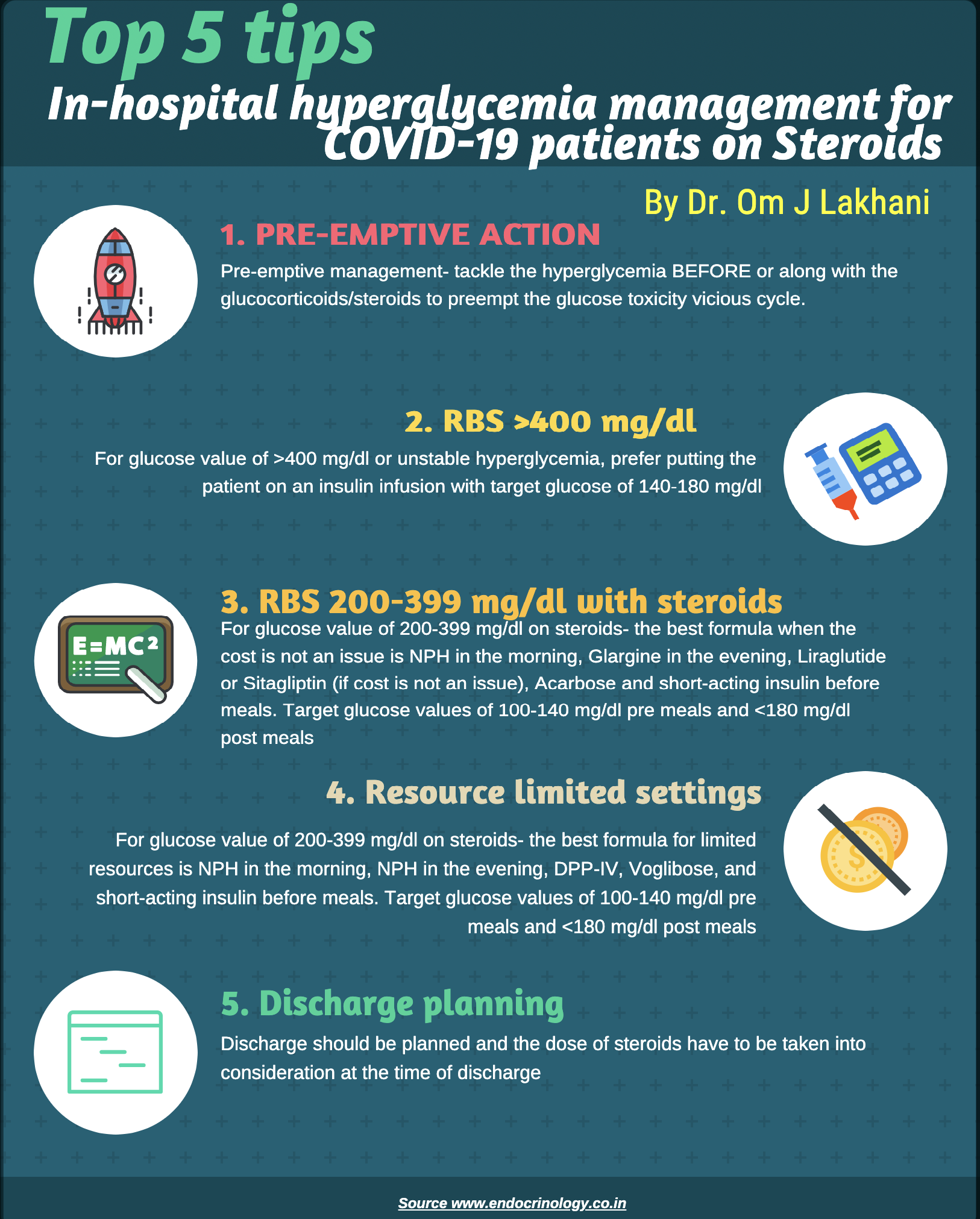
Take home messages
- Pre-emptive management- tackle the hyperglycemia BEFORE or along with the glucocorticoids/steroids to preempt the glucose toxicity vicious cycle.
- For glucose value of >400 mg/dl or unstable hyperglycemia, prefer putting the patient on an insulin infusion with target glucose of 140-180 mg/dl
- For glucose value of 200-399 mg/dl on steroids- the best formula when the cost is not an issue is NPH in the morning, Glargine in the evening, Liraglutide or Sitagliptin (if cost is not an issue), Acarbose and short-acting insulin before meals. Target glucose values of 100-140 mg/dl pre meals and <180 mg/dl post meals
- For glucose value of 200-399 mg/dl on steroids- the best formula for limited resources is NPH in the morning, NPH in the evening, DPP-IV, Voglibose, and short-acting insulin before meals. Target glucose values of 100-140 mg/dl pre meals and <180 mg/dl post meals
- Discharge should be planned and the dose of steroids have to be taken into consideration at the time of discharge
Important note
This is the first version of this document. You may checking for any update on the same by visiting the link ____.
If you find any error or if you have any suggestion on the topic, please feel free to share at dromlakhani@gmail.com
Please consider donating to "Notes in Endocrinology" to keep us going. Please visit our DONATION page to know more
Lakhani OJ, Kumar S, Tripathi S, Desai M, Seth C. Comparison of two protocols in the management of glucocorticoid-induced hyperglycemia among hospitalized patients. Indian journal of endocrinology and metabolism. 2017 Nov;21(6):836. ↩︎
Nice-Sugar Study Investigators. Intensive versus conventional glucose control in critically ill patients. New England Journal of Medicine. 2009 Mar 26;360(13):1283-97. ↩︎
Umpierrez GE, Hellman R, Korytkowski MT, Kosiborod M, Maynard GA, Montori VM, Seley JJ, Van den Berghe G. Management of hyperglycemia in hospitalized patients in non-critical care setting: an endocrine society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism. 2012 Jan 1;97(1):16-38. ↩︎
Lakhani OJ, Kumar S, Tripathi S, Desai M, Seth C. Comparison of two protocols in the management of glucocorticoid-induced hyperglycemia among hospitalized patients. Indian journal of endocrinology and metabolism. 2017 Nov;21(6):836. ↩︎
Lakhani OJ, Kumar S, Tripathi S, Desai MA, Seth C. Correlation between basal insulin glargine dose required in achieving target fasting blood glucose and various clinical and laboratory parameters in hospitalized noncritical patients. Indian journal of endocrinology and metabolism. 2018 Jul;22(4):469. ↩︎
Umpierrez GE, Gianchandani R, Smiley D, Jacobs S, Wesorick DH, Newton C, Farrokhi F, Peng L, Reyes D, Lathkar-Pradhan S, Pasquel F. Safety and efficacy of sitagliptin therapy for the inpatient management of general medicine and surgery patients with type 2 diabetes: a pilot, randomized, controlled study. Diabetes care. 2013 Nov 1;36(11):3430-5. ↩︎
Verma V, Kotwal N, Upreti V, Nakra M, Singh Y, Shankar KA, Nachankar A, Kumar KH. Liraglutide as an alternative to insulin for glycemic control in intensive care unit: a randomized, open-label, clinical study. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2017 Sep;21(9):568. ↩︎