-
Connected notes
-
Q. What percentage of hypoglycemia observed in the DCCT trial was nocturnal?
- 43%
-
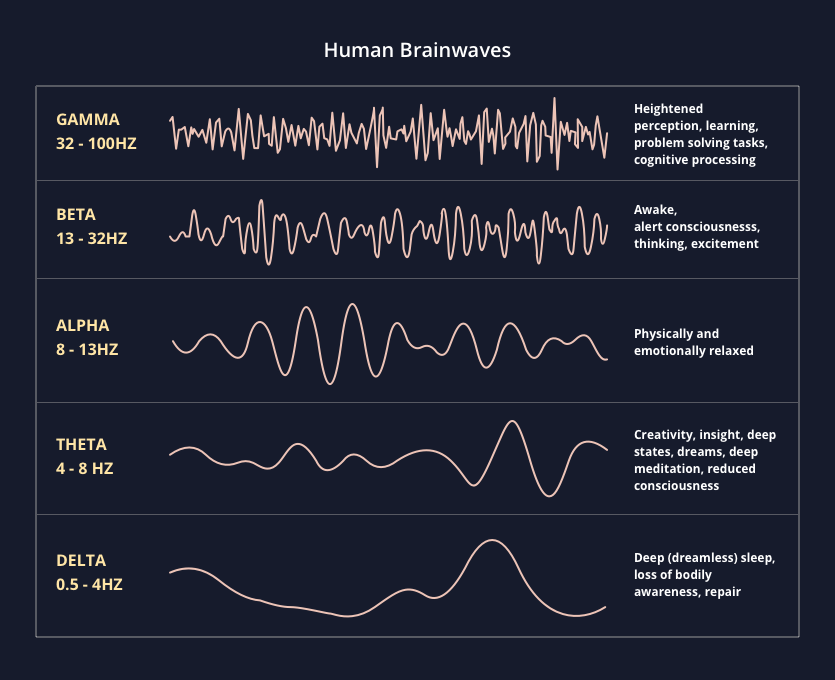
Q. What are the various types of brain waves?
-
Q. What happens to the brain waves during hypoglycemia in an awake state?
- there is a reduction in alpha waves but an increase in theta and delta waves
-
Q. What happens in hypoglycemia during sleep?
- In children- there are no changes in brain waves observed
- In adults- when glucose is <45 mg/dl
- There is a reduction of alpha waves
- Prominent changes in theta waves
-
Q. Does the brain have the same sensitivity to hypoglycemia during sleep, as when they are awake?
- yes
- The threshold for glucose values when brain waves changes occur suggests there is the same sensitivity for brain changes during sleep as it is during an awake state
- Hence brain retains inability to respond to hypoglycemia in sleep, atleast in adults
-
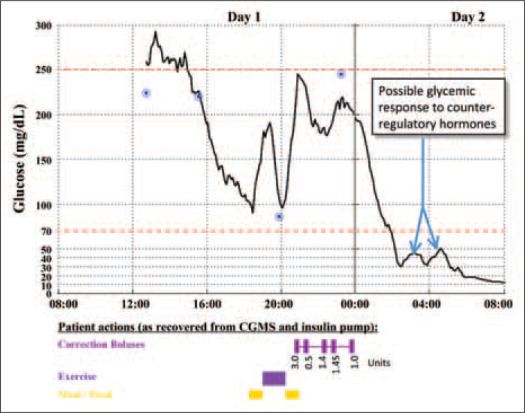
Q. But is the counter-regulatory response during sleep the same as during the awake state?
- No
- The counter-regulatory response to hypoglycemia is less profound during sleep than in an awake state
- The glucagon response is preserved in non-diabetics, but in certain patients with diabetes it is blunted (see below)
- The third line of defense, the sympathoadrenal response is reduced in people.
-
Q. Does the stage of the sleep also determine the response?
- Yes
- The counter-regulatory response is also dependent on the stage of the sleep cycle when hypoglycemia occurs.
-
Q. What is the clinical consequence on sleep quality in patients having nocturnal hypoglycemia?
- Adults with recurrent nocturnal hypoglycemia have poor sleep quality
-
Q. What percentage of nocturnal hypoglycemia are asymptomatic?
- A large proportion are asymptomatic
- 50% of adults and 78% of children are asymptomatic
- It may even be prolonged and last for as much as 6 hours
- A large proportion are asymptomatic
-
Q. What are the changes that occur to hepatic glucose production during sleep?
- During sleep hepatic glucose output reduces in response to reduce peripheral utilization of glucose
- this is mainly driven by continuous basal insulin secretion
-
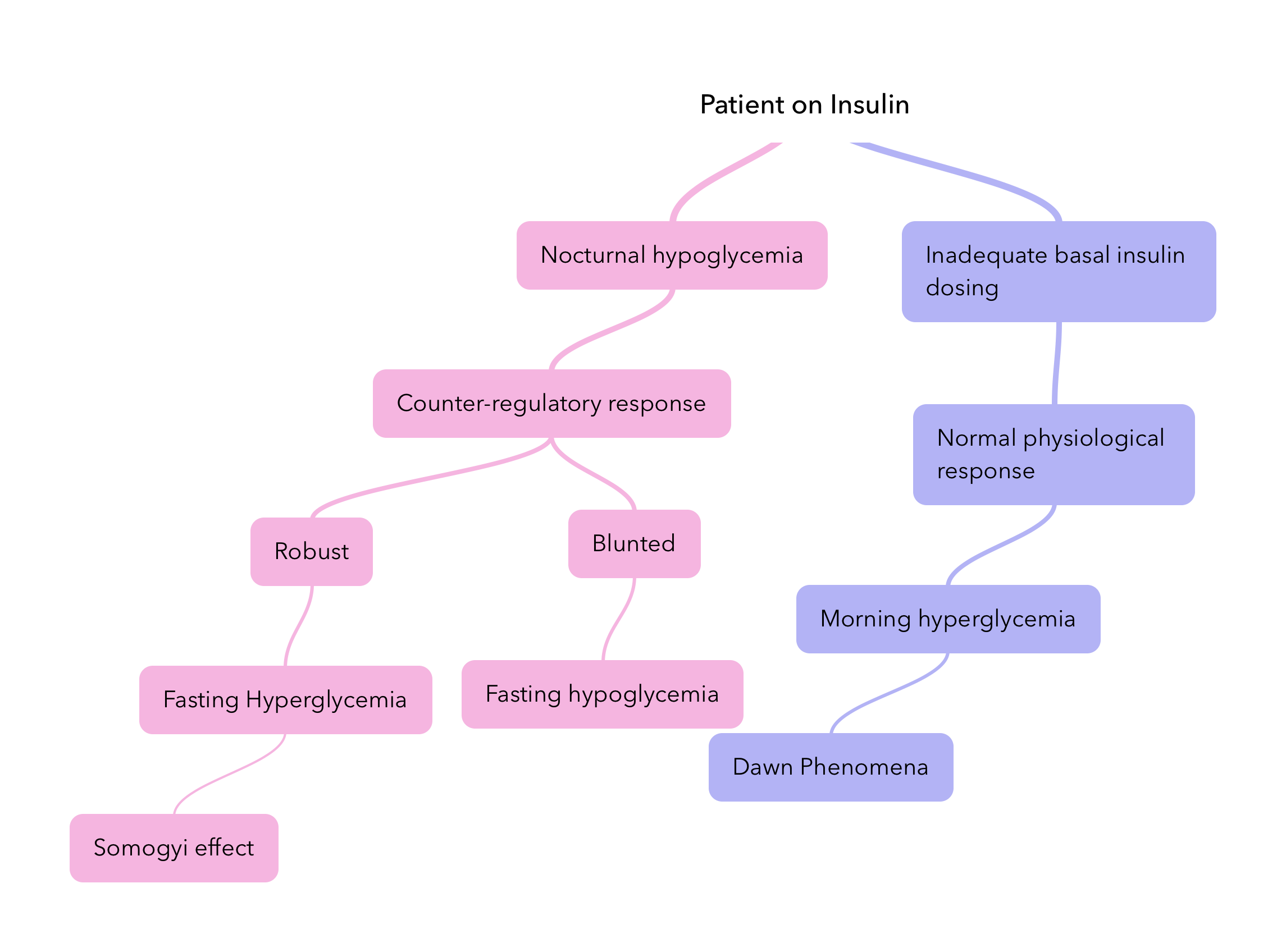
Q. It is true that type 1 and type 2 diabetes with beta-cell failure have reduced counter-regulatory hormones also?
- Yes
- In type 1 diabetes and those with beta-cell failure in type 2 diabetes also have blunted glucagon response
- This per se does not produce hypoglycemia but reduces their capacity to respond to hypoglycemia in case it develops
-
Q. What are the Somogyi effect and the Dawn phenomenon?
-
Q. Does the Somogyi effect exist in reality?
- Experimental evidence does show the existence of the Somogyi effect
- However, even during the period of NPH insulin use, it was rare
- The use of modern basal insulin nearly makes the phenomenon non-existent
-
Q. What is a good reliable test for predicting the risk of nocturnal hypoglycemia?
- The bedtime glucose value is a strong predictor of nocturnal hypoglycemia
- Bedtime glucose associated with nocturnal hypoglycemia
- <108 mg/dl in adults with type 1 diabetes
- <130 mg/dl in children with type 1 diabetes
- #Pearl:
- Bedtime glucose is a good predictor of hypoglycemia earlier in the night
- Fasting glucose a good predictor of early morning hypoglycemia
- FBS <99 mg/dl for a patient on basal-bolus insulin suggests early morning hypoglycemia may have occurred
-
Q. Which SMBG is useful for the diagnosis of nocturnal hypoglycemia?
- 3 am glucose reading
- Though this is impractical
- Hence CGM is useful for the diagnosis of nocturnal hypoglycemia
-
Q. Broadly, what are the symptoms of nocturnal hypoglycemia?
- Symptoms may be subtle and variable
- Poor sleep quality
- Vivid dreams and nightmares
- Morning headache
- Chronic fatigue
- Mood changes
- Night sweats and Wet bedsheets and bedclothes (because of sweat)
- Enuresis (in children)
- Restless behavior during sleep
- Symptoms may be subtle and variable
-
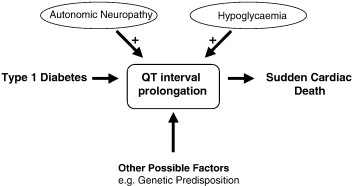
Q. Can it lead to mortality?
- Yes
- It can potentially trigger arrhythmia
- The "Dead-in-the-bed" syndrome
- Use of alcohol also contributes to the same in patients with diabetes
-
Q. Can convulsions occur due to nocturnal hypoglycemia?
- Yes
-
Q. What are the long terms issues with nocturnal hypoglycemia?
- Cognitive impairment
- hypoglycemia unawareness
-
Q. Can bedtime snacks reduce the risk of nocturnal hypoglycemia?
- Yes
- However, short-acting carbohydrates are not ideal for this purpose- they still make the patient vulnerable to hypoglycemia early in the morning
- Uncooked cornstarch is ideal for such an action
- Adding acarbose before dinner is also a useful way of preventing nocturnal hypoglycemia in both type 1 and type 2 diabetes
-
Q. What are the other ways of preventing nocturnal hypoglycemia?
-
- Using modern long-acting basal insulin analogs
- Glargine U300
- Insulin degludec
-
- Using rapidly acting insulin analogs before dinner
-
- Use of sensor-augmented insulin pumps
-
-
Q. Does giving glargine U100 in the morning reduce the risk of nocturnal hypoglycemia?
- Yes
- In some patients, this is seen
- This is probably because glargine U100 may not work for 24 hours in some patients- hence the effect of glargine wears off during nighttime
- However insulin glargine U300 solves this problem
Further reading:
- Allen KV, Frier BM. Nocturnal hypoglycemia: clinical manifestations and therapeutic strategies toward prevention. Endocr Pract. 2003 Nov-Dec;9(6):530-43. doi: 10.4158/EP.9.6.530. PMID: 14715482.