- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
- Q. What is the definition of NICTH (Non-Islet cell Tumor hypoglycemia) & IGF-2 related hypoglycemia?
- It denotes hypoglycemia caused by a tumor other than Insulinoma
- Q. Which tumors produce NICTH?
- Mesenchymal tumor (Fibrosarcoma)
- Vascular tumor- Hemingopericytoma
- Fibroma
- Hepatocellular carcinoma- most common cause
- Adrenocortical carcinoma- second most common
- Colorectal cacrinoma
- Multiple myeloma
- Carcinoid
- Lymphoma

- Q. What are the possible causes of NICTH?
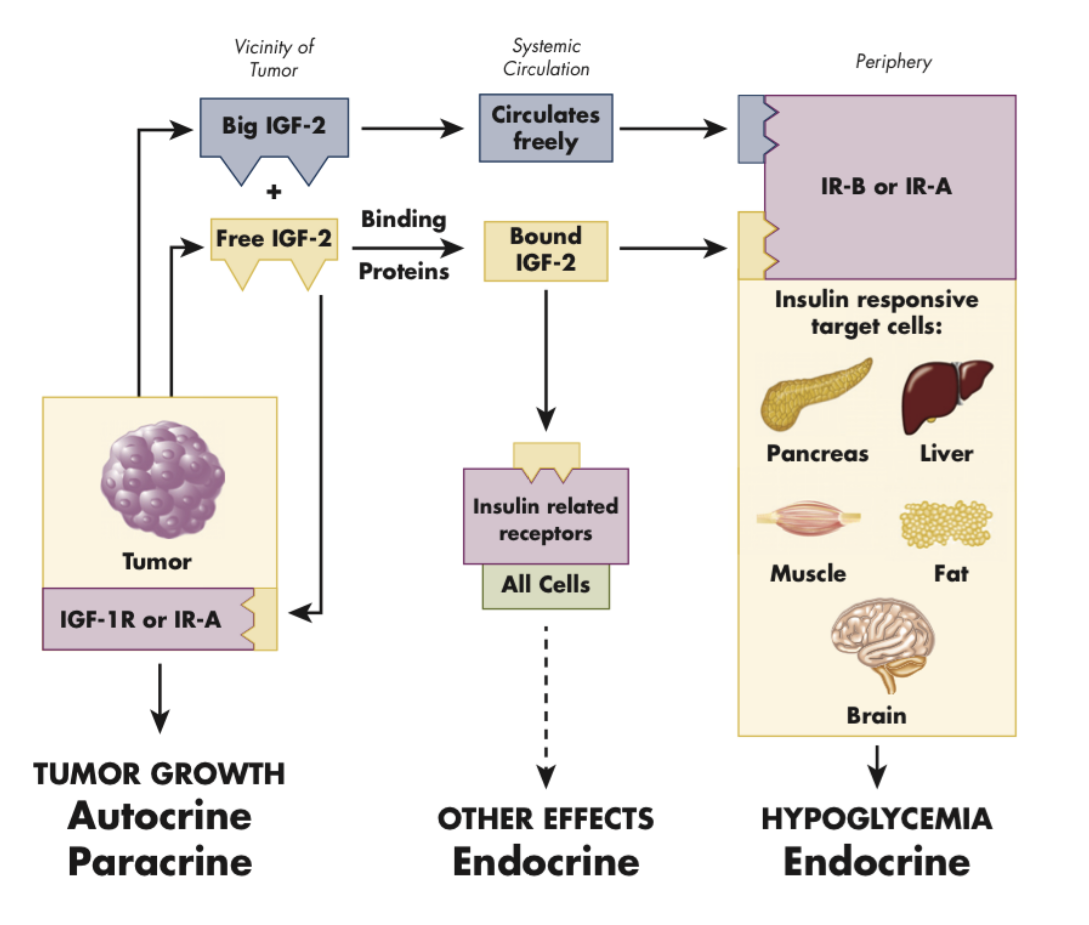
- Excess of Big IGF-2
- Extensive destruction of glucose by the liver
- Insulin antibodies
- Insulin receptor antibodies
- Ectopic Insulin or IGF-1 production
- Q. What is Big IGF-2?
- This is incompletely processed IGF-2
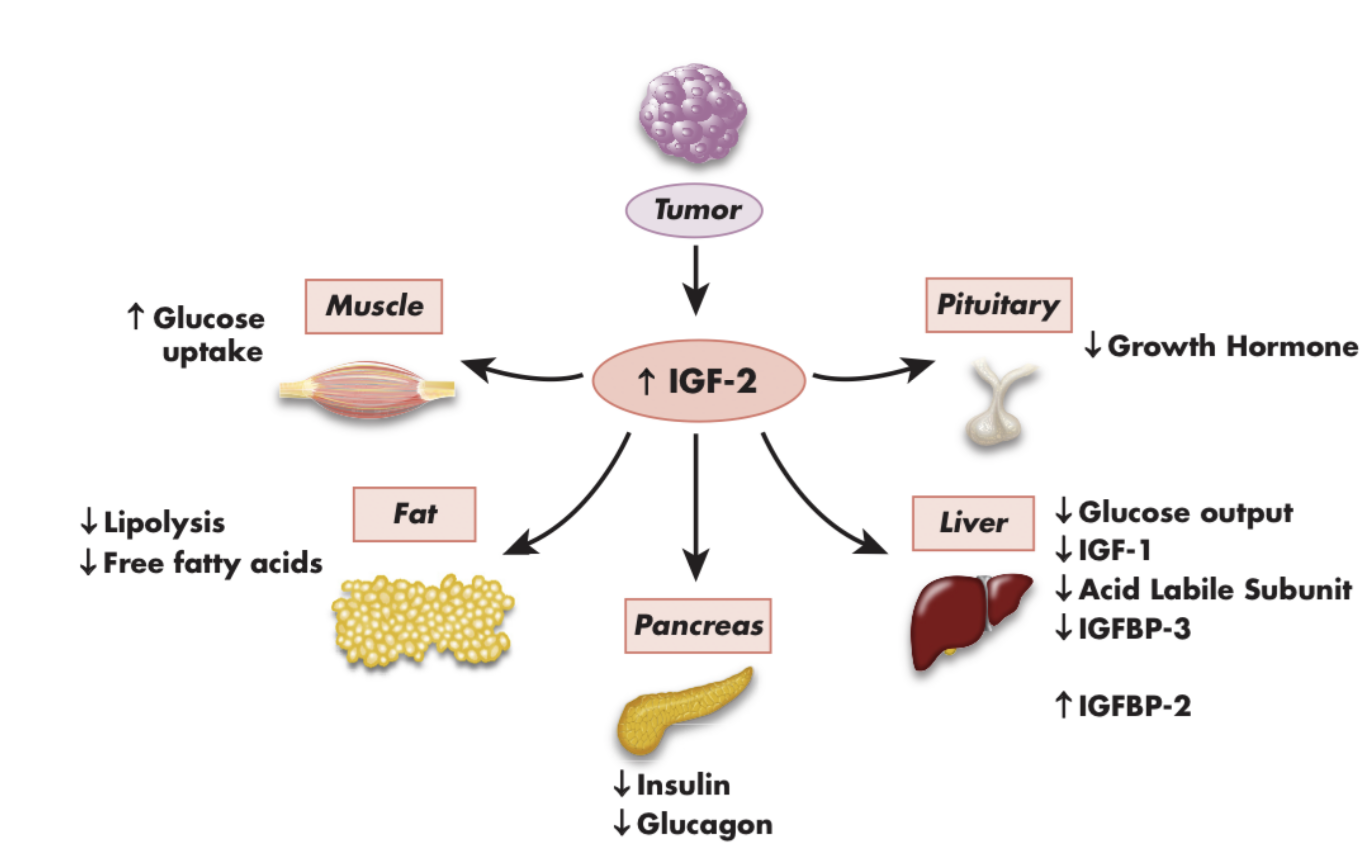
- Q. What are the consequences of IGF-2?
-
- Autocrine-Paracrine stimulation of the tumor
-
- Spontaneous hypoglycemia- mainly fasting hypoglycemia
-
- Acromegaloid features in some patients
-
- Q. What type of hypoglycemia is seen with NICTH?
- Fasting hypoglycemia
- Q. Does the diagnosis of tumor occur first or does hypoglycemia occur first?
- The tumor is generally diagnosed first before hypoglycemia occurs
- These are generally large tumors
- Q. Which is the most important tumor which is associated with NICTH (Non-Islet cell Tumor hypoglycemia) & IGF-2 related hypoglycemia?
- Hepatocellular carcinoma
- Adrenocortical carcinoma is a distant second
- Q. What is the most common clinical presentation of hypoglycemia in these patients?
- These patients present with neuroglycopenia symptoms mainly
- Loss of judgment and changes in behavior are some of the earliest signs of hypoglycemia in these patients
- Q. What is the biochemical picture in NICTH?
- Glucose – low
- C peptide- low
- Insulin- low
- Proinsulin- low
- BOHB- low
- Response to glucagon – present
- Q. What happens to the GH response in these patients?
- The GH response is blunted because of suppression by IGF-2
- Q. Which test is a part of biochemical tests in the critical sample- give a hint of possible IGF-2-related hypoglycemia?
- These patients have a picture of insulin-independent hypoglycemia- Insulin, C-peptide, and Proinsulin are all low
- The key differentiating factors are two folds:
- beta-hydroxybutyrate is low -
- If this was high- it would suggest a variation of normal or extreme starvation
- GH's response is blunted
- the absence of raise in GH levels
- beta-hydroxybutyrate is low -
- Q. Which other electrolyte imbalance is seen in these patients?
- Hypokalemia is often seen
- Q. Why do some of these patients develop postprandial hyperglycemia?
- This is because IGF-2 suppresses the pancreatic beta-cell function
- Hence some of these patients may have fasting hypoglycemia but postmeal hyperglycemia
- Q. Summarize the physiology of IGF-2
- Q. Which are specific tests done for diagnosis of NICTH?
- Big IGF-2 measurement
- IGF-2 IGF1 ratio
- Q. Which tumors produce insulin autoimmune syndrome?
- Multiple myeloma
- Hodgkin’s lymphoma
- Q. What is the management of NICTH?
- Removal of the tumor
- Glucocorticoids – reduce IGF-2
- Q. What are the conditions in which hypoglycemia and Acromegaloid features coexist?
-
- IGF-2 related hypoglycemia
-
- MEN1 syndrome
-
- Q. What is "Rhinophyma"? This is a feature of which possible endocrine condition?
- Rhinophyma is a condition characterized by the thickening of the skin of the nose, resulting in a bulbous, red appearance
- This may be seen in Acromegaly

- Q. What are the conditions that lead to "pseudohypoglycemia"?
- In patients with Leukemia or Polycythemia- may have pseudohypoglyemia
- This is because of the increased RBC consumption the glucose leading to low glucose reading in the lab
- Q. Within what period in a 72-hour fast test do patients with Insulinoma manifest the features of hypoglycemia?
- Hypoglycemia is manifested within 24-36 hours of a 72-hour-fast test in patients with Insulinoma
- Q. What is a good clinical way of judging hypoglycemia symptoms during a 72-hour fast test?
- Asking the patient to perform serial 7 subtraction test regularly is a good way of assessing for developing hypoglycemia
- Q. What happens to IGF-2 levels in NICTH (Non-Islet cell Tumor hypoglycemia) & IGF-2-related hypoglycemia ?
- IGF-2 levels may be elevated or normal
- If they are elevated - it confirms the diagnosis
- but normal value - may not rule it out
- Q. Which other test is useful in this situation?
- The molar ratio of IGF-2:IGF-1 is useful
- Ratio 10:1 is diagnostic of this condition
- Upto 3:1 ratio is normal
- Q. In which other condition is the IGF-2:IGF-1 ratio significantly elevated?
- Sepsis
- Severe cachexia
- Q. What happens to the IGFBP levels?
- IGFBP1 and IGFBP2 are elevated
- IGFBP3 is reduced
- Q. Summarize the impact of IGF-2 on liver products.
- Reduced glucose
- Reduced IGF-1
- Reduced ALS (acid labile subunit)
- Reduced IGFBP3
- Increased IGFBP2
- Q. Which other IGF-2-like component can be measured if IGF-2 is normal?
- Pro-IGF-2 can be measured
- There is an assay developed for the same
- Q. Can non-islet cell tumors produce some other components which can cause hypoglycemia?
- Yes
- Rare cases of IGF-1 and Insulin-producing tumors have been reported
- Q. Summarize the biochemical diagnosis of NICTH (Non-Islet cell Tumor hypoglycemia) & IGF-2 related hypoglycemia
- Q. Which organ produces IGF-2 in normal circumstances?
- It is produced by the liver
- Q. What is the timing of hypoglycemia seen in NICTH (Non-Islet cell Tumor hypoglycemia) & IGF-2 related hypoglycemia?
- It is mainly fasting hypoglycemia
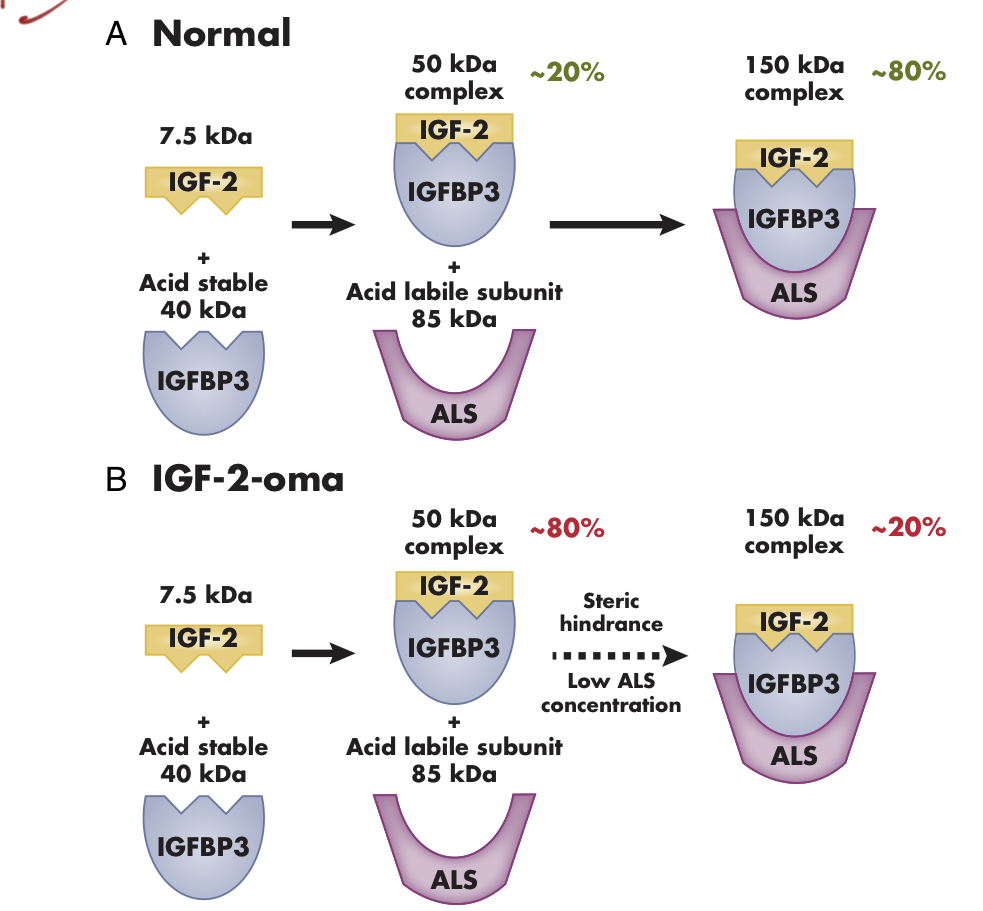
- Q. What is the difference in IGF-2-related complexes in normal patients versus those having NICTH (Non-Islet cell Tumor hypoglycemia) & IGF-2-related hypoglycemia?
- In Normal people 80% of the IGF2 is in form of a complex of IGF-2-IGFBP3-ALS. This is a 150 kDa ternary complex
- In NICTH (Non-Islet cell Tumor hypoglycemia) & IGF-2 related hypoglycemia - 80% of the complex is in form of IGF-2 with IGFBP3. This is a smaller 50 KDA binary complex
- This is formed because of suppression of ALS production by IGF-2
- Q. Can you tell me the sequence of conversion from Prepro IGF2 complex to IGF2?
- See the picture below
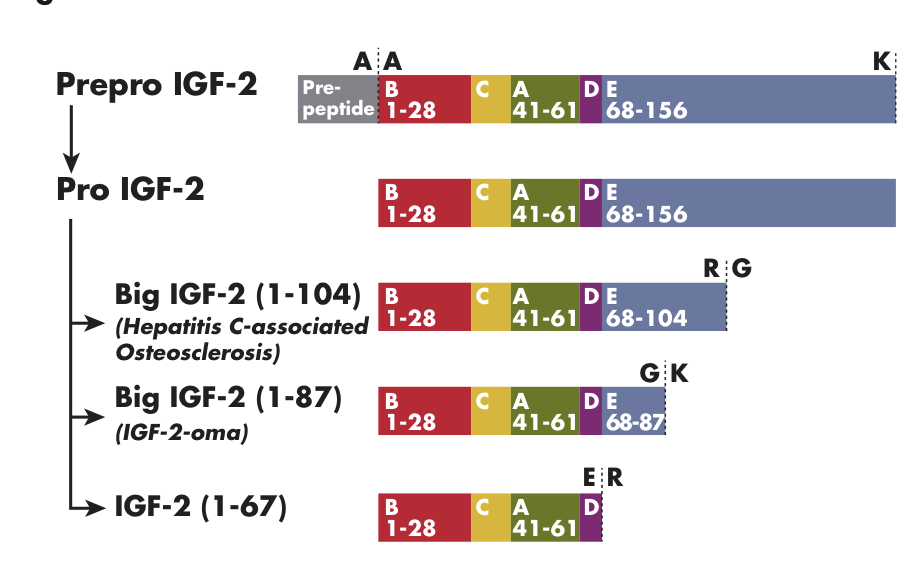
- Q. Of the above, which component primarily causes hypoglycemia?
- The interaction of the Big IGF2 (1-87) with the insulin receptor is mainly responsible for the hypoglycemia seen in this condition
- Q. Which other endocrine disorder is seen because of IGF-2?
- Big IGF-2 produces Hepatitis-C associated osteosclerosis
- Q. Do patients with Hepatitis-C associated osteosclerosis also have hypoglycemia?
- Interestingly, no
- Patients with this condition do not have hypoglycemia while patients with IGF-2-related hypoglycemia do not have osteosclerosis!
- This is because both are caused by a distinct isoform of Big-IGF2
- Q. What is the treatment for this condition?
- Treatment is directed towards two things:
-
- Treatment of the underlying tumor
- Resection of the underlying tumor often resolves the symptoms
- In some cases where the tumor may not be completely resectable, debulking is also helpful
-
- Management of hypoglycemia
- Glucocorticoids are the first line of therapy geared towards correcting hypoglycemia in this condition and are found to be very useful
- Interestingly, growth hormone therapy is the second line of therapy in this condition (despite the theoretical risk of tumor progression)
- It is also interesting to note that Somatostatin analogs are NOT useful in this condition
-
- Treatment is directed towards two things:
- Q. How does growth hormone help in this condition?
- Growth hormone increases the production of IGFBP3 and ALS leading to increase binding of the Free IGF2 and its removal from the circulation
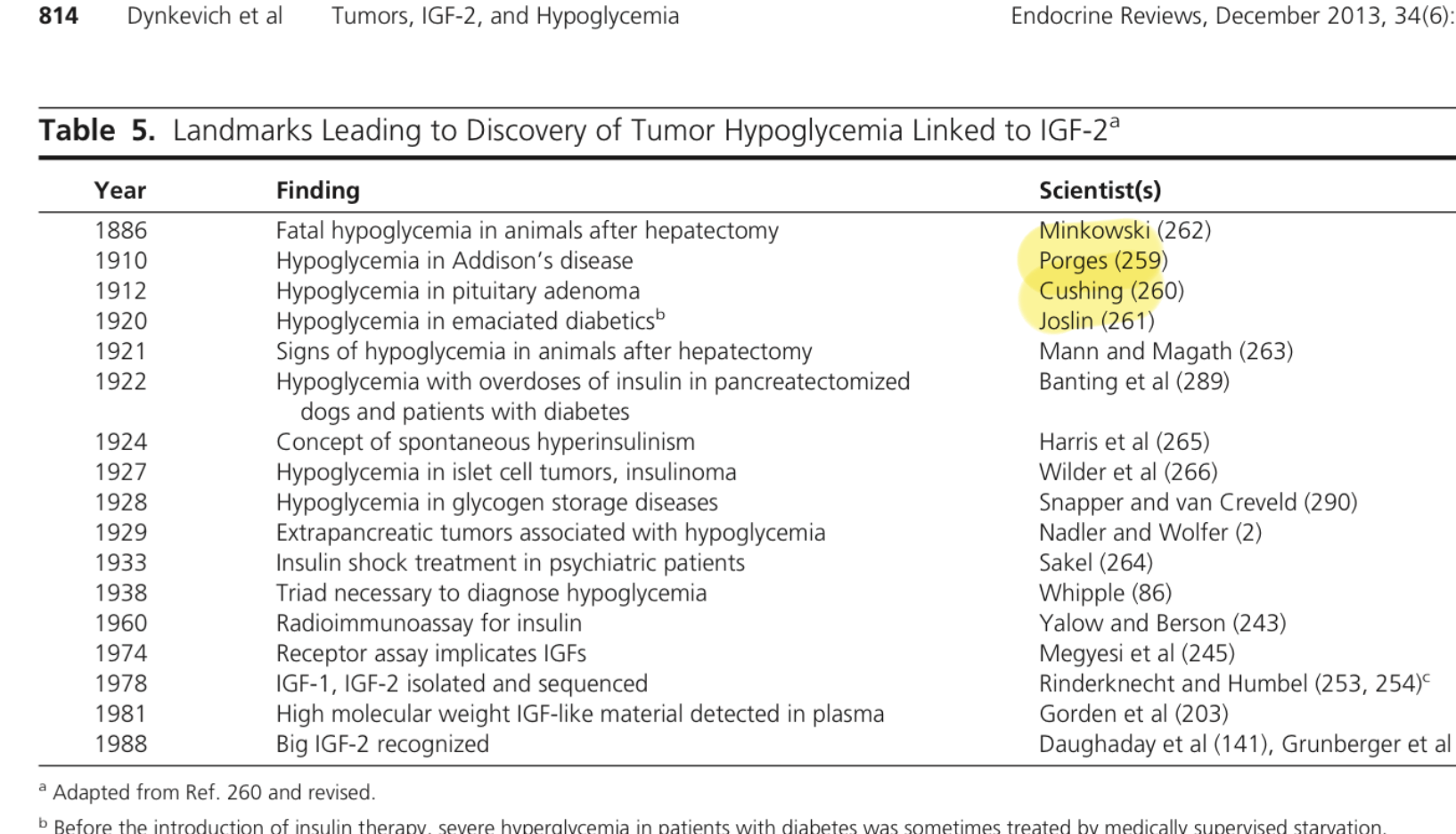
- Q. Can you give some landmarks in the discovery of hypoglycemia and IGF2-related disease?
- Q. Who was the first person to give the concept of hypoglycemia?
- The concept of Hypoglycemia was first understood from the work of Minkowski and von Mering who demonstrated fatality in animals after hepatectomy
- They also demonstrated that the pancreas was the source of antidiabetic agent (insulin) that later led to the discovery of insulin
- Q. How was hypoglycemia discovered in humans?
- Hypoglycemia was first demonstrated in humans having Addison's disease by Porges, in patients operated from the pituitary tumor by Cushing, and in emaciated diabetics by Joslin
- Q. In which condition was hypoglycemia used as a form of therapy?
- Insulin shock therapy was a form of treatment for patients with schizophrenia
- Typically 100-150 units of insulin were used to produce severe hypoglycemia
- This treatment was later replaced
Reference:
Dynkevich Y, Rother KI, Whitford I, Qureshi S, Galiveeti S, Szulc AL, Danoff A, Breen TL, Kaviani N, Shanik MH, LeRoith D. Tumors, IGF-2, and hypoglycemia: insights from the clinic, the laboratory, and the historical archive. Endocrine Reviews. 2013 Dec 1;34(6):798-826.