- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
- Q. What are the two types of autoimmune Hypoglycemia?
-
- Insulin autoimmune syndrome (Hirata's disease)
- Also called Hirata's disease
-
- Type B Insulin resistance
- Antibody against the insulin receptor
-
- Q. What are the definition and diagnostic criteria for Insulin autoimmune syndrome (Hirata's disease)?
- All of the following criteria must be present
- (I) hyperinsulinemic Hypoglycemia ;
- (II) elevated Insulin autoantibody (IAA) titers;
- (III) no prior exposure to exogenous insulin ;
- (IV) no pathological abnormalities of the pancreatic islets.
- Recently however many cases have been observed in which the patient has had exposure to insulin. Hence point III is not considered redundant
- All of the following criteria must be present
- Q. Which other autoimmune disease is Insulin autoimmune syndrome (Hirata's disease) most closely linked with?
- Graves' disease
- It could be because of
-
- Common autoimmune source
-
- Induced by the use of antithyroid drugs
-
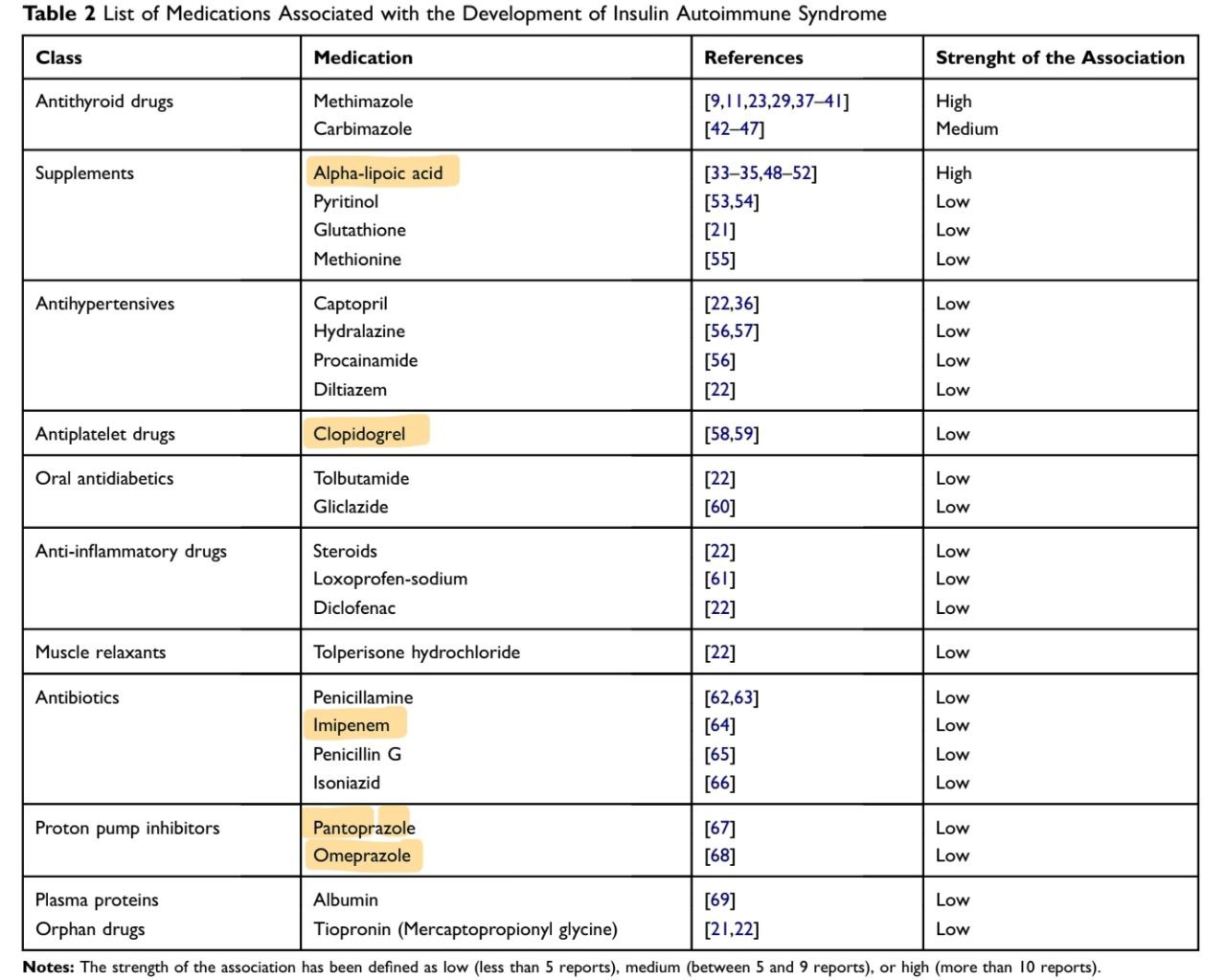
- Q. Which commonly used drugs have been linked with Insulin autoimmune syndrome (Hirata's disease)?
-
- antithyroid drugs - Carbimazole, Methimazole
-
- Alpha lipoic acid
-
- Clopidogrel
-
- Steroids
-
- Diclofenac
-
- Imipenem
-
- Isoniazid
-
- Pantoprazole
-
- Omeprazole
-
- Of these methimazole and alpha lipoic acid have the strongest link to the disease
- Q. Which HLA has a strong link with the development of Insulin autoimmune syndrome (Hirata's disease)?
- HLA DRB1*0406
- This is more common in Asians hence the disease is more common in Asians
- Q. How many weeks after starting the offending medication does the disease develop?
- It typically develops 4-6 weeks after starting the offending medication
- Q. Apart from medications, which other triggers have been identified?
-
- Viral infections
-
- Hematological diseases
-
- Q. Which viruses are known to be triggers?
-
- Hepatitis C
-
- Measles
-
- Mumps
-
- Coxsackie B
-
- Varicella zoster
-
- Rubella
-
- Q. Which hematological disorders have been linked?
- Multiple myeloma
- Monoclonal gammopathy
- Q. What type of hypersensitivity is Insulin autoimmune syndrome (Hirata's disease)?
- it is Type VII hypersensitivity
- It is a novel category of hypersensitivity
- Q. Which is the key pathogenic antibody causing this disease?
- Insulin autoantibody (IAA)
- This is an IgG antibody
- Q. Does the mere presence of IAA produce the disease?
- No
- Low titers of the antibody in circulation do not produce the disease
- Q. What are the clinical phases of Insulin autoimmune syndrome (Hirata's disease)?
- Initially, the antibodies bind to the insulin leading to a transient reduction in insulin levels and hence transient postprandial hyperglycemia
- After this, the insulin dissociates from the antibody irrespective of the glucose levels leading to the development of Hypoglycemia
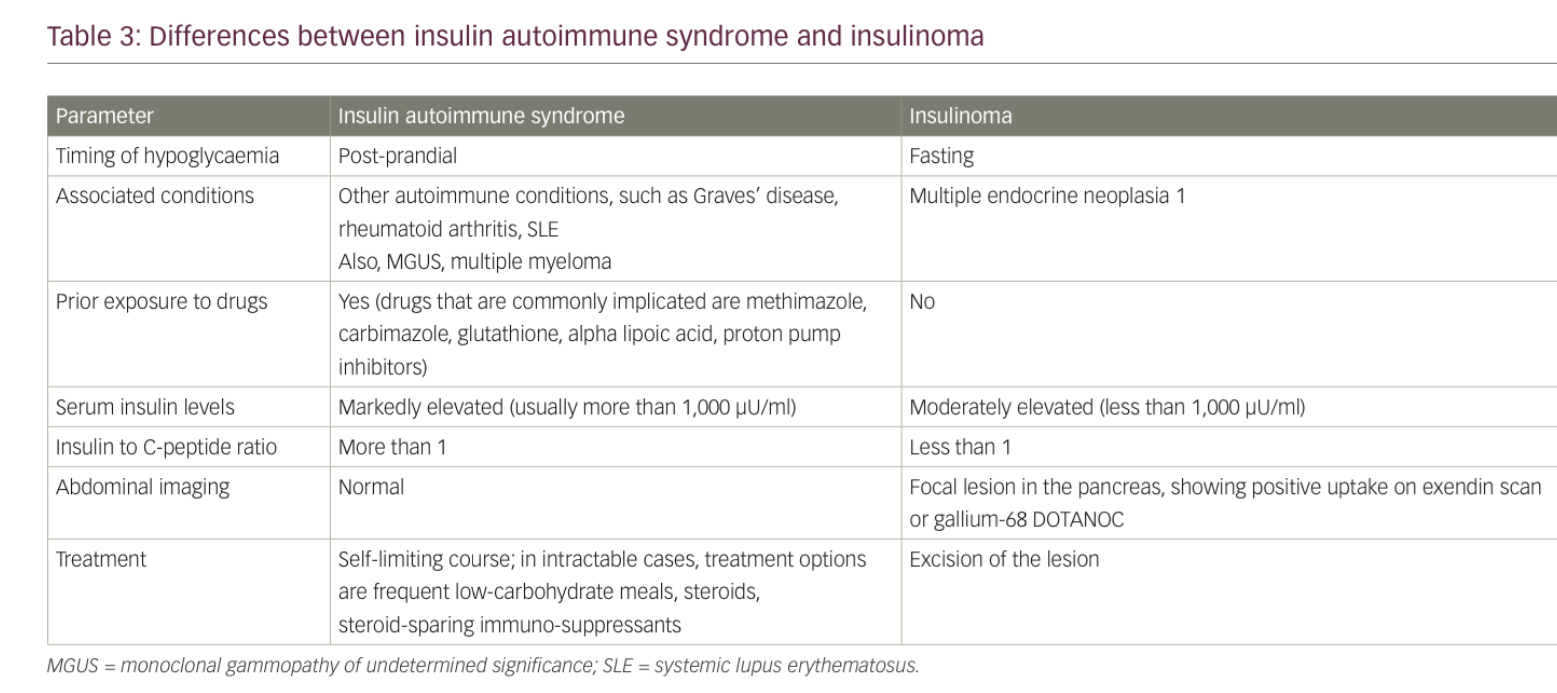
- Q. How does one distinguish between Insulinoma and Insulin autoimmune syndrome (Hirata's disease)?
-
- Clinically
- Insulin autoimmune syndrome produces mainly post-prandial Hypoglycemia. It can also produce fasting and exercise-induced Hypoglycemia
- Insulinoma- mainly produces fasting Hypoglycemia
-
- Insulin: C-peptide ratio
- Convert insulin to pmol/l
- Conver C-peptide to pmol/l using units lab
- Insulin: C-peptide ratio calculated
- Less than 1 → suggestive of Insulinoma
- More than 1 → suggestive of Insulin autoimmune syndrome (Hirata's disease)
-
- Q. Why does the insulin: C-peptide ratio show what it shows?
- Insulin in circulation has a short half-life compared to C-peptide
- In Insulinoma there is a release of C-peptide and insulin both in large quantities released in equal concentration. C-peptide having a higher half-life is often found more easily in circulation
- In Insulin autoimmune syndrome (Hirata's disease) the C-peptide is released at its rate while the insulin is stuck to the antibody. Hence in these cases, insulin levels tend to be disproportionately more than C-peptide
- Q. Name two conditions in which insulin levels tend to be disproportionate compared to C-peptide levels.
- Insulin autoimmune syndrome (Hirata's disease)
- Exogenous insulin use
- Q. What is the problem with the measurement of insulin autoantibodies?
- Here only the IgG subclass of antibody is detected in the commercial assay
- Hence we may have false negative values
- Q. What should be done in case of false negative Insulin autoantibodies with high suspicion of the disease?
- Precipitation of the serum with PEG is done followed by recovery of the insulin from the supernatant
- In patients with Insulin autoimmune syndrome (Hirata's disease)
- After PEG precipitation- the bound insulin levels are higher than free insulin levels
- In normal people- free insulin is higher than bound insulin
- Q. What are the clinical features of patients having antibodies to insulin receptors?
- Here there is initially Hyperglycemia along with extreme insulin resistance
- the antibodies may be both blocking and stimulating
- in case blocking antibodies remain- they mainly lead to hyperglycemia and Insulin resistance
- In case of stimulating antibody present- they start developing hypoglycemia
- Q. Which tumors are associated with these insulin autoimmune syndromes?
- Antibody against insulin seen in multiple myeloma
- Antibody against insulin receptor sen in Hodgkin lymphoma
- Q. What is the treatment for this condition?
- Most cases are self-resolving
- It is because if the antigen is withdrawn- the antibody slowly withdraws over a while
- Generally within 3-6 months
- Q. What are the other treatment options?
- Small frequent meals with low carbohydrate content
- Acarbose
- Glucocorticoids
- Diazoxide
- Octreotide
- Partial pancreatectomy
- Plasmapheresis
- Other immunosuppressants
- Azathioprine
- Cyclophosphamide
- Mycophenolate
- Rituximab
- References:
- Boro H, Gupta U, Singh C, Malhotra R, Khadgawat R. Insulin Autoimmune Syndrome - A Case Series. Eur Endocrinol. 2020 Oct;16(2):168-171. doi: 10.17925/EE.2020.16.2.168. Epub 2020 Oct 6. PMID: 33117451; PMCID: PMC7572167.
- Cappellani D, Macchia E, Falorni A, Marchetti P. Insulin Autoimmune Syndrome (Hirata Disease): A Comprehensive Review Fifty Years After Its First Description. Diabetes Metab Syndr Obes. 2020 Apr 1;13:963-978. doi: 10.2147/DMSO.S219438. PMID: 32308449; PMCID: PMC7136665.