- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
- Video lecture
Connected notes:
-
Q. What are the symptoms of hypoglycemia?
- Based on the Adrenergic system
- Palpitations
- Tremors
- Anxiety
- Based on the Cholinergic system
- Hunger
- Excessive sweating
- Paraesthesia
- Based on the Central nervous system
- Seizures
- Confusion
- Abnormal behavior
- Loss of consciousness
- Fatigue
- Based on the Adrenergic system
-
Q. What is the difference between venous and arterial Blood glucose values?
- Venous glucose is 20-30 mg/dl lower than arterial blood level in the fasting state
- In postprandial – venous and arterial are the same
- Whole blood is 10% lower than Plasma glucose
-
Q. Why does hypoglycemia cause "Dead in bed syndrome"?
- Hypoglycemia may cause
- QT prolongation
- Increase QT dispersion
- Increase the risk of arrhythmia
- Nocturnal hypoglycemia can cause arrhythmia in sleep dead in bed syndrome
- Hypoglycemia may cause
-
Q. What is the incidence of hypoglycemia in type 1 diabetics?
- 1 episode per week
- 1 severe hypoglycemia episode per year
-
Q. What are the various categories of hypoglycemia in diabetics according to ADA?
- Level 1 - Glucose between 54 - 70 mg/dl
- Level 2- <54 mg/dl
- Level 3- Any Hypoglycemia requiring assistance/ admission or altered sensorium etc
-
Q. What is Probably symptomatic hypoglycemia?
- Probably symptomatic hypoglycemia- symptoms present by BG not determined
-
Q. What is relative hypoglycemia?
- Relative hypoglycemia- symptoms of hypoglycemia but BG >70 mg/dl
-
Q. What are the risk factors for hypoglycemia in diabetics?
- Insulin – carbohydrate mismatch
- Use of Sulphonylurea
- Renal failure
- Celiac disease
- Liver failure
- Exercise
- Hypoglycemic unawareness / HAAF
- Long-standing diabetes
- Use of alcohol
- Improved insulin sensitivity due to weight loss
-
Q. Which Oral antidiabetics produces the highest risk of hypoglycemia?
- Glibenclamide
Hypoglycemia-associated autonomic failure
-
Q. Which patients develop Hypoglycemia associated with autonomic failure (HAAF)?
- Patients with diabetes with insulin deficiency
- Long-standing Type 2 diabetes
- Type 1 diabetes
- Patients with diabetes with insulin deficiency
-
Q. What exactly happens in HAAF?
- There is a loss of sympathoadrenal response to hypoglycemia
-
Q. What is the mechanism of HAAF?
-
- Systemic mediator hypothesis
- Hypoglycemia release some systemic mediator like Cortisol → which blunts response to subsequent hypoglycemia
-
- Brain fuel hypothesis
- Hypoglycemia increases GLUT1 induction in the brain → normal glucose uptake in the brain despite low BG → hence the brain (hypothalamus) sympathoadrenal response does not occur
- However, PET studies have refuted this hypothesis
-
- Brain metabolism hypothesis
- Hypoglycemia alters glucose metabolism in the brain → no response to hypoglycemia
-
- Cerebral network hypothesis
- Dorsal midline thalamus inhibits Hypothalamus
- Hypoglycemia→ activates dorsal midline thalamus
-
-
Q. Is HAAF associated with autonomic neuropathy that occurs in diabetics?
- No
- It is a distinct syndrome NOT associated with autonomic neuropathy in diabetics
- Autonomic neuropathy in diabetics also produces a similar picture but is a chronic process
-
Q. What are the types of HAAF?
- Sleep-related HAAF- diabetics are less aware of hypoglycemia during sleep unlike non-diabetics
- Exercise-related HAAF nocturnal hypoglycemia occurs 6-8 hours after exercise
- Antecedent HAAF → Previous hypoglycemia producing less response in subsequent hypoglycemia
-
Q. How is HAAF treated?
- It is treated by strict avoidance of hypoglycemia for 2-3 weeks corrects HAAF
Prevention of hypoglycemia in patients with diabetes
- Q. What are the three questions with regards to hypoglycemia that must be asked of a patient with diabetes in each visit?
-
- Any recorded episodes of hypoglycemia
-
- Any symptoms suggestive of hypoglycemia
-
- Episodes of hypoglycemia in which assistance of another individual was required (level 3 hypoglycemia)
-
- Q. What are the broad outlines for preventing hypoglycemia in patients with diabetes?
-
- Frequent SMBG
-
- Patient Education
-
- Rational treatment
-
- Individualized HBA1c targets
-
- Identifying patients at higher risk
-
- Diagnosis of Hypoglycemic unawareness and Autonomic neuropathy
-
- Q. Does technology help to reduce hypoglycemia?
- Yes
- [[CGM and [[Sensor augmented insulin pump help to reduce the risk and severity of hypoglycemia
- Q. Does the use of [[Insulin pump (CSII) itself reduce the risk of hypoglycemia ?
- No
- The usual pumps do not reduce the risk of hypoglycemia
- [[Sensor augmented insulin pump reduce the risk of hypoglycemia
- Q. What are the changes to the insulin that can be made to reduce hypoglycemia?
- Use of newer basal insulin
- Use of rapid-acting insulin analogs
- Q. What is done for patients with [[hypoglycemia unawareness ?
- 2-3 weeks of strict avoidance of hypoglycemia is helpful to restore awareness
- Keep more lenient HBA1c goals in these patients
- Q. How much carbohydrate can be consumed by patients to prevent exercise-induced hypoglycemia?
- 1 gram/kg/hour of carbohydrate intake
- Q. What is an option for patients with severe hypoglycemia with ESRD?
- Pancreatic transplantation with kidney transplantation is a good option for these patients
#update 18-Jan-2023 - Source: Hypoglycemia in Diabetes guidelines by Endocrine society
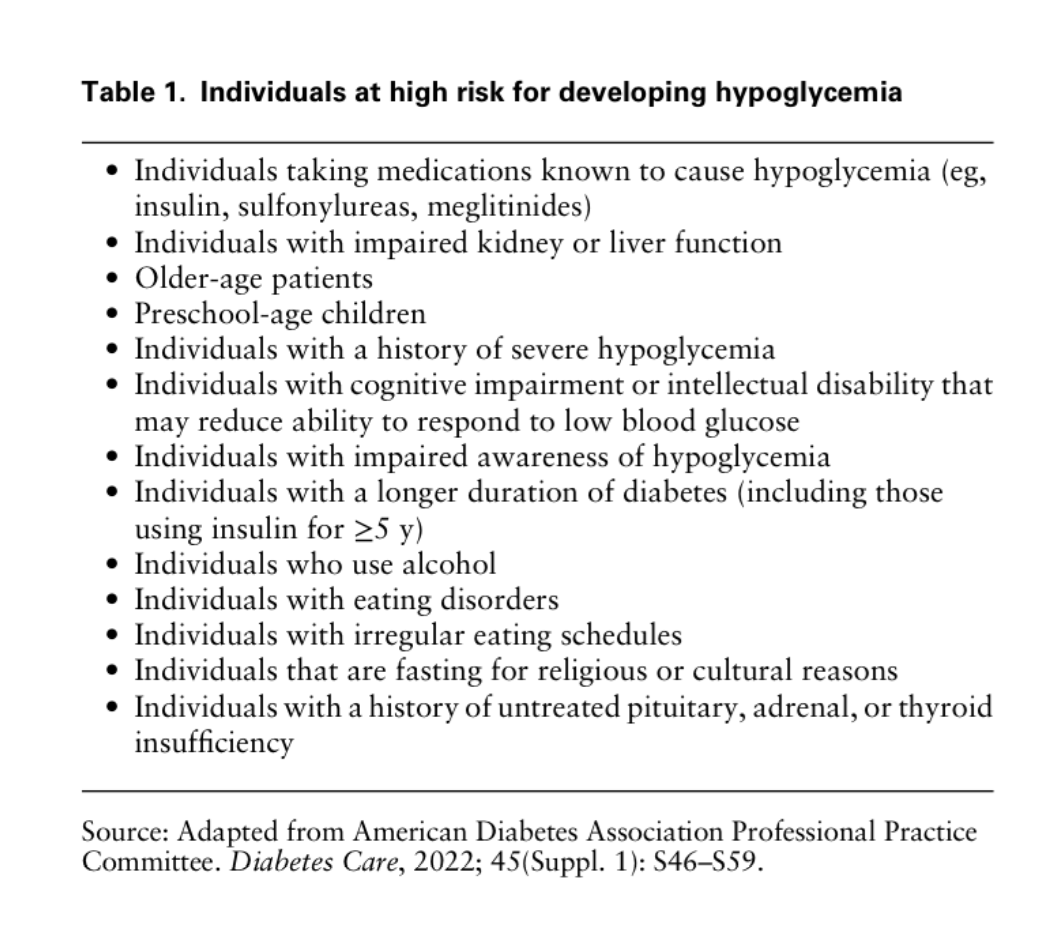
- Q. Enlist the risk factors for Hypoglycemia in patients with diabetes as given by the guidelines ?
- Q. What is ADIPs ?
- Algorithm driven insulin pumps
- 1/ Algorithm-driven insulin pumps, also known as "smart pumps" or "artificial pancreas systems", use mathematical algorithms to adjust insulin delivery in real-time.
- 2/ These pumps include a continuous glucose monitor (CGM) that measures glucose levels and a pump that delivers insulin.
- 3/ The algorithm uses the glucose data from the CGM to calculate the appropriate insulin dose and adjust the pump accordingly.
- 4/ Examples of algorithm-driven insulin pumps include Medtronic MiniMed 670G, 780G and Tandem t:slim X2 insulin pump.
- 5/ These pumps are designed to reduce the burden of diabetes management by automatically adjusting insulin delivery and can help reduce the risk of hypoglycemia and hyperglycemia, and improve overall diabetes control.
- 6/ Overall, Algorithm-driven insulin pumps are becoming increasingly popular among people with diabetes, as they can provide a more effective and efficient way to manage the disease.
- Q. For patients with type 1 diabetes- should SMBG be used regularly or should CGM be used regularly ?
- The new guidelines suggests the use of CGM rather than SMBG in patients with Type 1 Diabetes
- SMBG can be used to confirm the abnormal glucose readings from CGM
- Q. What about pumps ?
- The guidelines recommend the use of ADIPs for patients with type 1 diabetes to reduce the burden of hypoglycemia
- Q. Can we use CGM for Hospital hyperglycemia ?
- Yes
- Current guidelines recommend the use of CGM in selected patients for Hospital hyperglycemia to prevent hypoglycemia episodes
- This is provided that extremes of glucose values are cross-checked with glucometers
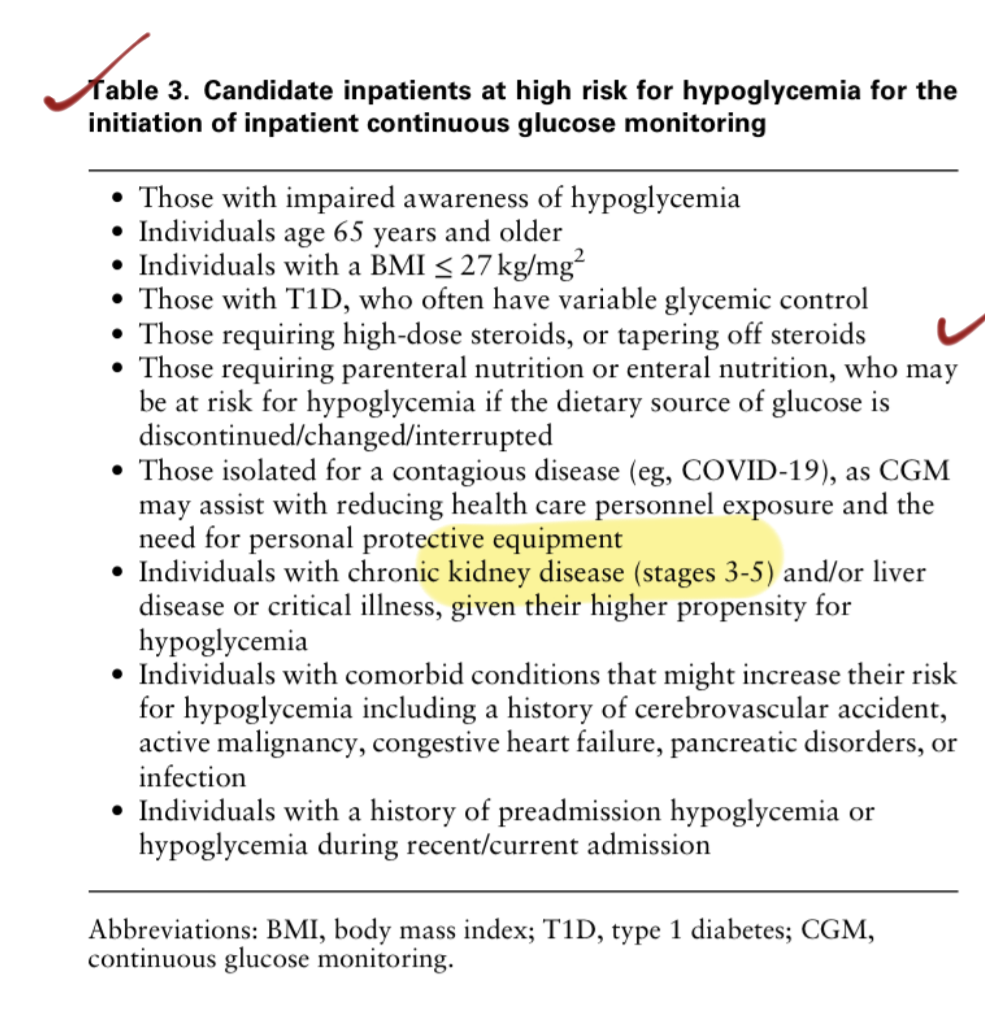
- Q. In which patients is CGM recommended for Hospital hyperglycemia ?
- Q. In which hospitalized patient can you expect inaccurate reading with CGM ?
- Extensive skin infection
- Hypoperfusion
- Hypovolumeia
- Medications
- Inotrope use
- Those on acetaminophen > 4 gram/day
- Dopamine
- Vitamin C
- Heparin
- Hydroxyurea
Reference: McCall AL, Lieb DC, Gianchandani R, MacMaster H, Maynard GA, Murad MH, Seaquist E, Wolfsdorf JI, Wright RF, Wiercioch W. Management of Individuals With Diabetes at High Risk for Hypoglycemia: An Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology & Metabolism. 2022 Dec 7.