- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
- Video lecture
Connected notes:
- Hypoglycemia in patients with diabetes mellitus
- Insulin autoimmune syndrome
- NICTH (Non Islet cell Tumor hypoglycemia) & IGF-2 related hypoglycemia
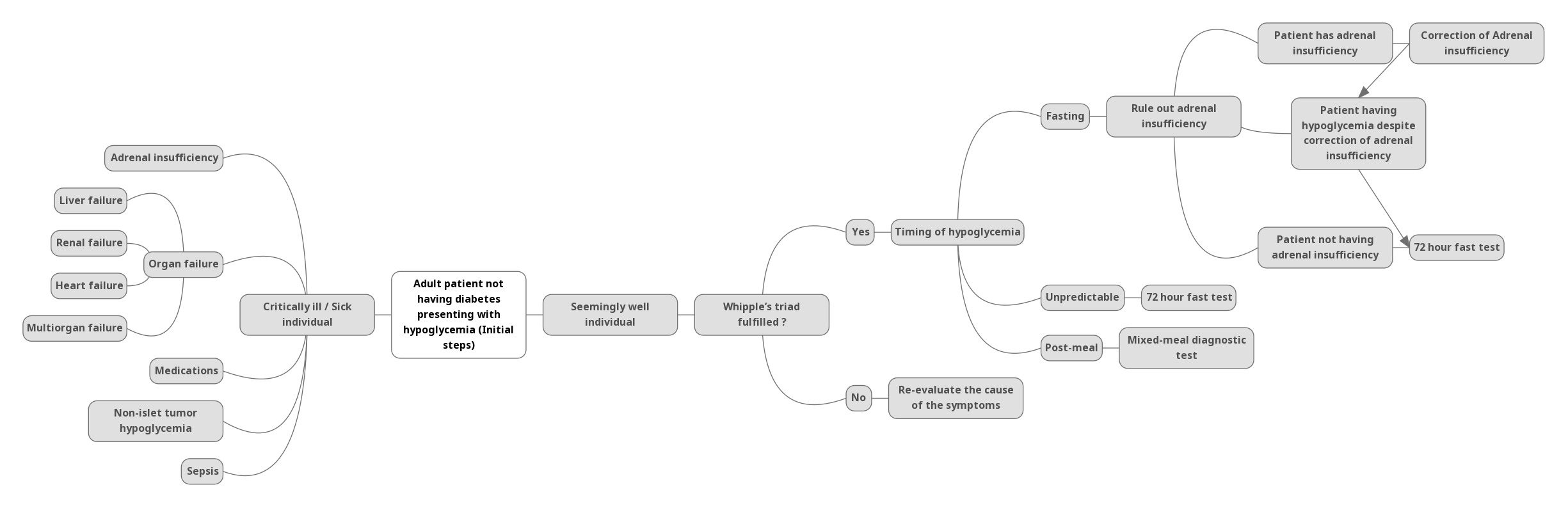
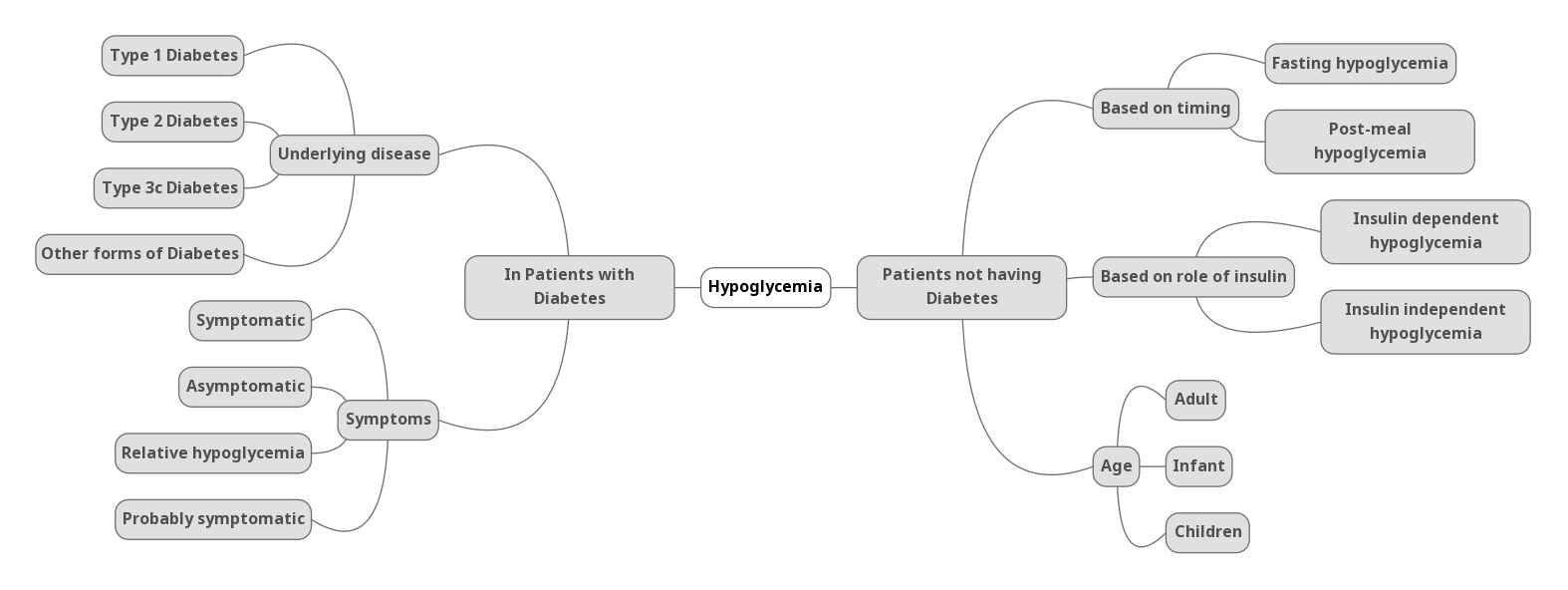
- Q. Summarize the approach to hypoglycemia in patients not having diabetes.
- Q. What are the various classifications for Hypoglycemia in non-diabetics?
- Fasting vs postprandial
- Insulin mediated vs non-insulin mediated
- Hypoglycemia in ill patient vs seemingly well patient
-
Q. Enlist the causes of hypoglycemia in a non-diabetic individual.
-
- Hypoglycemia in seemingly well individual
- Exogenous use of Insulin/sulphonylurea
- Insulinoma
- Insulin autoimmune syndrome
- NIPHS - non-insulinoma pancreatogogus hyperinsulinemia syndrome
- Post-bariatric hypoglycemia
- Hypoglycemia in ill or seemingly unwell individual
- Medications- insulin, alcohol, etc
- Critical illness
- Liver failure
- Renal failure
- NICTH- Non-islet cell tumor
- Adrenal insufficiency
- Panhypopituitarism
- Hypoglycemia in seemingly well individual
- Q. Which drugs other than antidiabetics cause hypoglycemia?
- Alcohol
- IGF1 (Increlex)
- Quinolone
- Quinine
- Pentamidine
- ACEI
- Beta-blockers
- Q. How does alcohol produce hypoglycemia?
- Alcohol inhibits gluconeogenesis
- Q. What is the cause of hypoglycemia in NICTH (Non-islet cell tumor hypoglycemia)?
- It is due to IGF-II
- They are mainly mesenchymal tumors
- Q. What is pseudo hypoglycemia?
- When a fluoride bulb is not used for the transport of blood sample
- BG is utilized by the cells @ 10-20 mg/dl per hour
- Q. is hypoglycemia common in patients with liver disease?
- No. Not all individuals
- It occurs only when there is rapid and fulminant liver damage like toxic hepatitis
- Diagnostic approach to hypoglycemia in non-diabetic individuals
- Q. What test is done for patients having fasting hypoglycemia and what is done for post-prandial hypoglycemia?
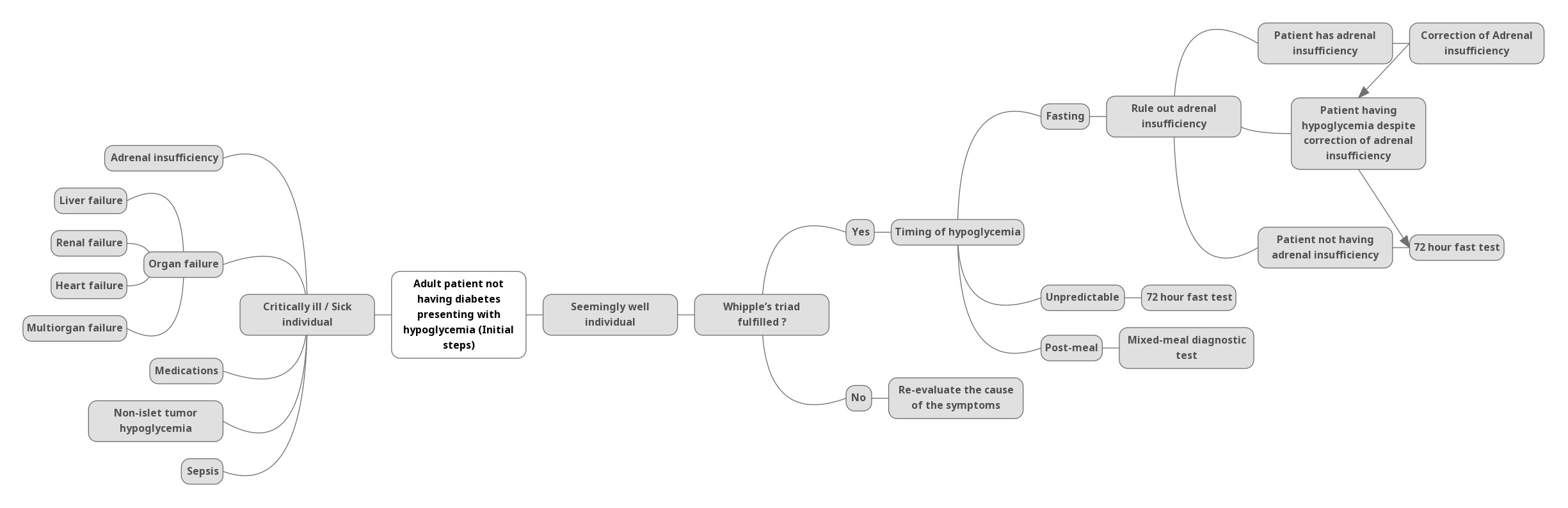
- Fasting hypoglycemia – 72-hour fast test
- Postprandial hypoglycemia- Mixed meal diagnostic test
- Q. What are mixed meal diagnostic tests and mixed meal tolerance tests?
- Mixed meal diagnostic test- for postprandial hypoglycemia
- Mixed meal tolerance test- due to seeing C peptide response to meal to different type 1 and type 2 diabetes or evaluated endogenous glucose production in diabetes
- Q. When is hypoglycemia considered fasting and when is it postprandial?
- <5 hours after a meal – postprandial
- More than 5 hours after meal- fasting
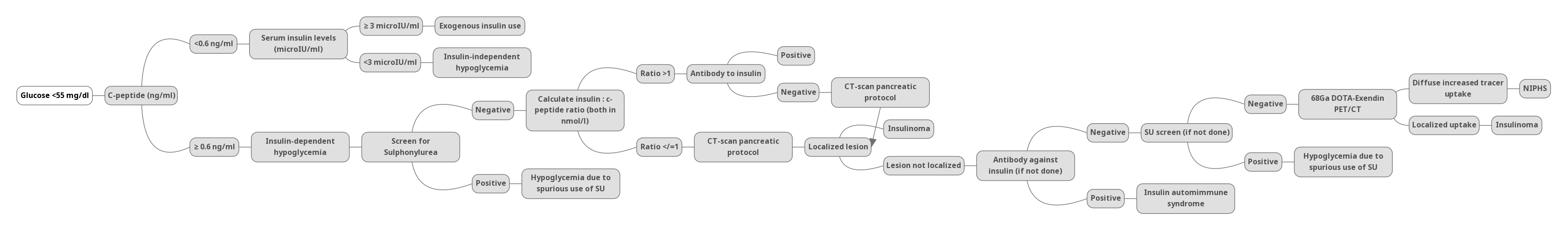
- Q. At what glucose cutoff are tests for C-peptide etc performed on the sample?
- When BG concentration <60 mg/dl –samples are analyzed
- BG <55 mg/dl for interpretation of reports
- Q. What tests are done once hypoglycemia is achieved?
- Plasma glucose
- C peptide
- Insulin
- Proinsulin
- Beta-hydroxybutyrate
- Sulphonylurea / Meglitinide screen
- Insulin autoantibody (no need for fasting)
- Q. Describe the protocol for the Mixed meal diagnostic test.
- Baseline sample as described above
- Take a regular meal or the meal that causes hypoglycemia
- Blood was collected every 30 min for 5 hours and check PG
- Once PH <60 mg/dl- do the additional tests
- If symptoms of hypoglycemia develop midway – then take additional samples at that time
- Q. Describe the 72-hour fast test.
- Discontinue all nonessential meds
- Patient can take liquids during the test – must not have calorie or caffeine
- Collect samples every 6 hrly till BG <60 mg/dl then every 1-2 hourly
- Analyze samples that have BG <60 mg/dl only
- Q. When is fast ended?
- Symptoms of hypoglycemia develop
- BG <55 mg/dl with Whipple’s trial established
- BG<45 mg/dl – with or without Whipple’s triad
- 72 hours have passed
- Q. What is done at the end of the fast?
- Give 1 mg of glucagon IV
- Then take samples for glucose at 10,20 and 30 min
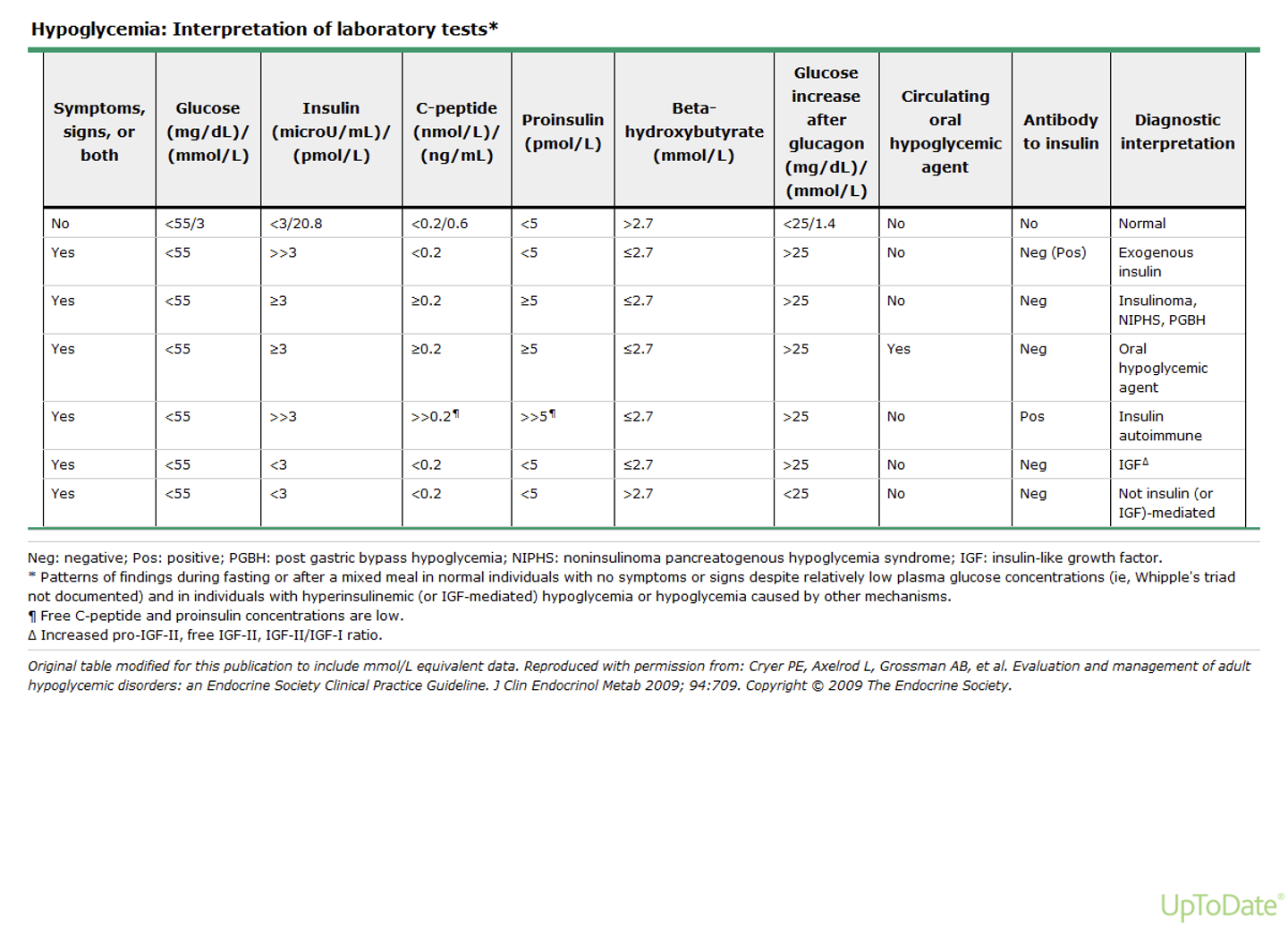
- **Interpretation of the data **
-
Q. Give the summary for interpretation of the results.
-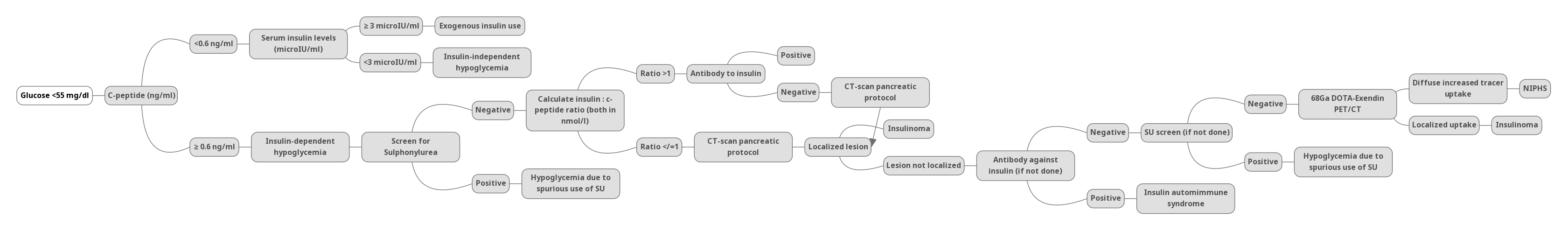
- Q. What is a normal response?
- When Glucose <55 mg/dl
- C peptide <0.6 ng/ml
- Insulin <3 uU/ml
- Proinsulin - <5 pmol/l
- BOHB - >2.7 mmol/l (since insulin is suppressed, ketones are formed)
- Glucose increase to glucagon - <25 mg/dl (glycogen stores are depleted, hence there is no immediate response to glucagon )
- When Glucose <55 mg/dl
- Q. What happens in case of Hyperinsulinemic hypoglycemia?
- When Glucose <55 mg/dl
- C peptide >0.6 ng/ml
- Insulin >3 uU/ml
- Proinsulin - >5 pmol/l
- BOHB - <2.7 mmol/l (since insulin is not suppressed, ketones are not formed)
- Glucose increase to glucagon - >25 mg/dl (glycogen stores are not depleted because of insulin, hence there is no quick response to glucagon )
- When Glucose <55 mg/dl
- Q. What happens in case of Exogenous insulin use?
- When Glucose <55 mg/dl
- C peptide <0.6 ng/ml
- Insulin >3 uU/ml
- Proinsulin - <5 pmol/l
- BOHB - <2.7 mmol/l (since insulin is not suppressed, ketones are not formed)
- Glucose increase to glucagon - >25 mg/dl (glycogen stores are not depleted because of insulin, hence there is no quick response to glucagon )
- When Glucose <55 mg/dl
- Q. What happens in the case of NICTH? (Due to IGF-II)
- When Glucose <55 mg/dl
- C peptide <0.6 ng/ml
- Insulin <3 uU/ml
- Proinsulin - <5 pmol/l
- BOHB - <2.7 mmol/l (IGF-2 acts like insulin)
- Glucose increase to glucagon - >25 mg/dl
- When Glucose <55 mg/dl
- Q. Summarize the response in all conditions.
- **Localization of Insulinoma **
- Q. What are the tests for localization in case of a suspected insulinoma?
-
- CT pancreatic protocol
-
- Endoscopic ultrasound
-
- PET scan- Gallium DOTANOC PET or Exendin scan
-
- Selective arterial calcium stimulation test
-
- Q. Give the interpretation of the Selective arterial calcium stimulation test.
- More than 2 fold increase in insulin in any artery territory is a positive response
- If there is an increase in response in all arteries- suggestive of a Diffuse process of NIPHS
- If there is increased uptake in one artery alone- s/o of Insulinoma
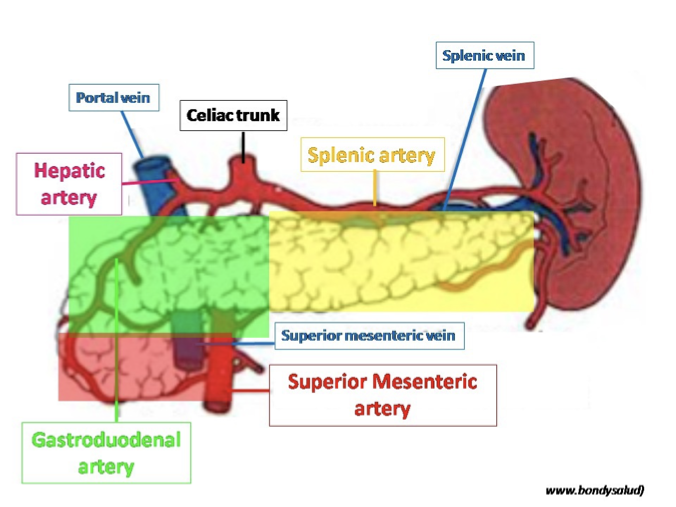
- Q. Response in which artery suggests what location of an insulinoma?
- Gastroduodenal – Head of the pancreas
- Superior mesenteric artery- Body of pancreas
- Splenic artery- tail of the pancreas
- Postprandial Hypoglycemia
- Q. What is the definition of Postprandial hypoglycemia?
- Hypoglycemia within 4-5 hrs of meal
- Q. What are the causes of Postprandial hypoglycemia?
- NIPHS (Noninsulinoma pancreatogenous hypoglycemia syndrome)
- Insulin autoimmune syndrome
- Post gastric bypass
- Post-bariatric surgery
- Insulinoma
- Hereditary fructose intolerance
- Factitious hypoglycemia
- Mild early type 2 diabetes
- Early Post pancreatic transplant
- Large amount of alcohol with simple carbs- Gin and Tonic syndrome
- Q. What is post prandial syndrome ?
- Post-prandial syndrome was previously called reactive hypoglycemia
- It is anxiety, perspiration, or palpitation after a meal
- It is blood glucose <50 mg/dl on extended OGTT but symptoms not correlating with the drop in blood sugar
- Only those patients with PPS fulfilling Whipple’s triad may be subjected to further evaluation
- Q. How is post-prandial syndrome treated?
- With reassurance
- Small frequent meals with high fiber content
- Acarbose may help
- Q. What is the investigation of choice for Postprandial hypoglycemia?
- It is a mixed meal diagnostic test
- Q. Give the protocol for the mixed meal diagnostic test
- Draw blood before giving a meal
- Then give the normal meal which the patient takes every day or the meal that specifically causes hypoglycemia (avoid using glucose or liquid meals- conflicting results)
- Collect blood samples every 30 min for 5 hrs
- If a patient develops symptoms then collect additional blood samples before giving carbohydrate
- All samples labeled and sent to the lab
- First check glucose in the lab- further tests are to be done only if glucose in the sample is <55 mg/dl
- Additional tests are :
- Insulin
- C peptide
- Additional tests are :
- If Whipple’s triad is established then also test for
- Insulin antibodies
- SU/ Meglitinide
- Q. What is alimentary hypoglycemia?
- It is a form of a post-prandial syndrome rather than true post-prandial hypoglycemia in patients who have undergone upper GI surgery
- Q. What is dumping syndrome?
- This also occurs in patients who have undergone GI surgery
- It is the feeling of fainting after a meal
- Because of undigested food in the intestine- there is an increase osmotic shift of fluid into the GI tract
- This leads to a reduction of circulating volume
- This occurs 15-30 min after a meal and is not associated with hypoglycemia
- Insulin autoimmune syndrome- See separate notes - click on the link
-
NIPHS (NON-INSULINOMA PANCREATOGENOUS HYPOGLYCEMIA SYNDROME)
-
Q. What type of hypoglycemia is seen with NIPHS?
- Mainly postprandial hypoglycemia
-
Q. What are the histological changes seen in NIPHS?
- The histological changes are called NESIDOBLASTOSIS
- The beta cell hypertrophies and has enlarged hyperchromatic nuclei
-
Q. What are the biochemical changes in NIPHS?
- They are similar to Insulinoma ie when BG <55 mg/dl there is
- Insulin > 3 mIU/ml
- C peptide > 0.6 ng/dl
- Beta-hydroxybutyrate < 2.7 mmol/l
- Glucose increases by >25 mg/dl after glucagon
- They are similar to Insulinoma ie when BG <55 mg/dl there is
-
Q. What are the DD of Nesidoblatosis ?
- NIPHS
- Nesdioblastosis in neonates and infants
- Prolonged use of Sulphonylureas
- Non-tumor cells in insulinoma
- Post roux en Y gastric bypass
-
Q. How is NIPHS localized?
- NIPHS is a diffuse process so not localized
- However, you need to rule out insulinoma hence localization studies may be required
- Absence of insulinoma may SUGGEST NIPHS, however it is difficult to distinguish in such a scenario
- The best approach would be to do selective arterial calcium stimulation
- In Insulinoma- there would be a response to a single artery, in NIPHS there would response in multiple arteries
- NIPHS is a diffuse process so not localized
-
Q. What is the treatment of NIPHS?
- In mild to moderate cases
- Small frequent meals
- Acarbose / Octreotide
- In severe cases
- Partial or subtotal pancreatectomy
- Region for resection dictated by Selective arterial calcium stimulation
- In mild to moderate cases
- NICTH (Non Islet cell Tumor hypoglycemia) & IGF-2 related hypoglycemia - See separate notes. Click on the link
- Insulinoma
- Q. Insulinoma is commonly malignant, True or false?
- False
- It is mainly benign
- Malignancy is rare
- Q. What is the demographic of a patient having an insulinoma
- Mean age- 48 years
- M > F
- Q. Is the Octerotide scan or DOTA scan a good idea for Insulinoma?
- No
- Often does not pick up insulinoma since they often lack SSTR2 receptor
- Q. What is the new functional scan for localization of Insulinoma?
- GLP-1 scintigraphy
- ⁶⁸Ga-DOTA-Exendin-4 PET/CT is often used for this purpose
- Q. What will you suspect if there is recurrence or persistence of symptoms post-op in case of an insulinoma?
- MEN1 syndrome
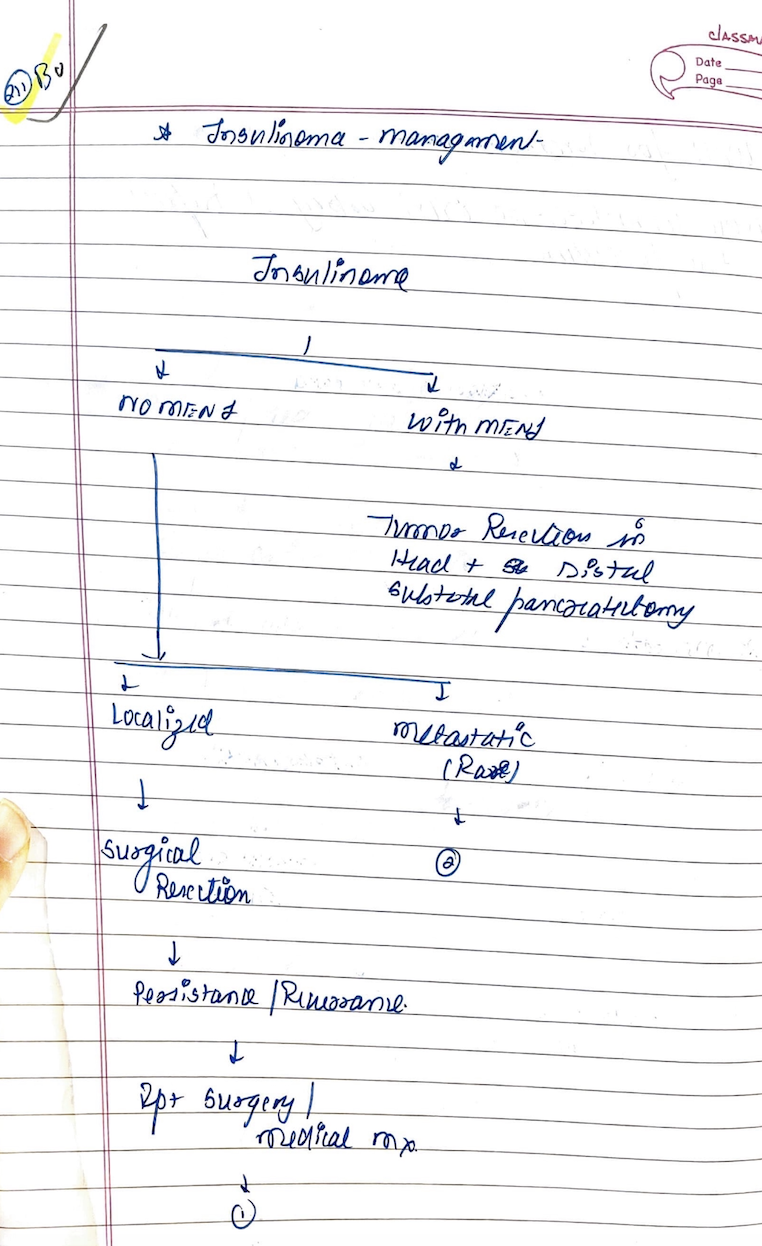
- Q. What is the surgery done for Insulinoma in MEN1 syndrome?
- Resection of any visible tumor in the head of the pancreas + distal subtotal pancreatectomy
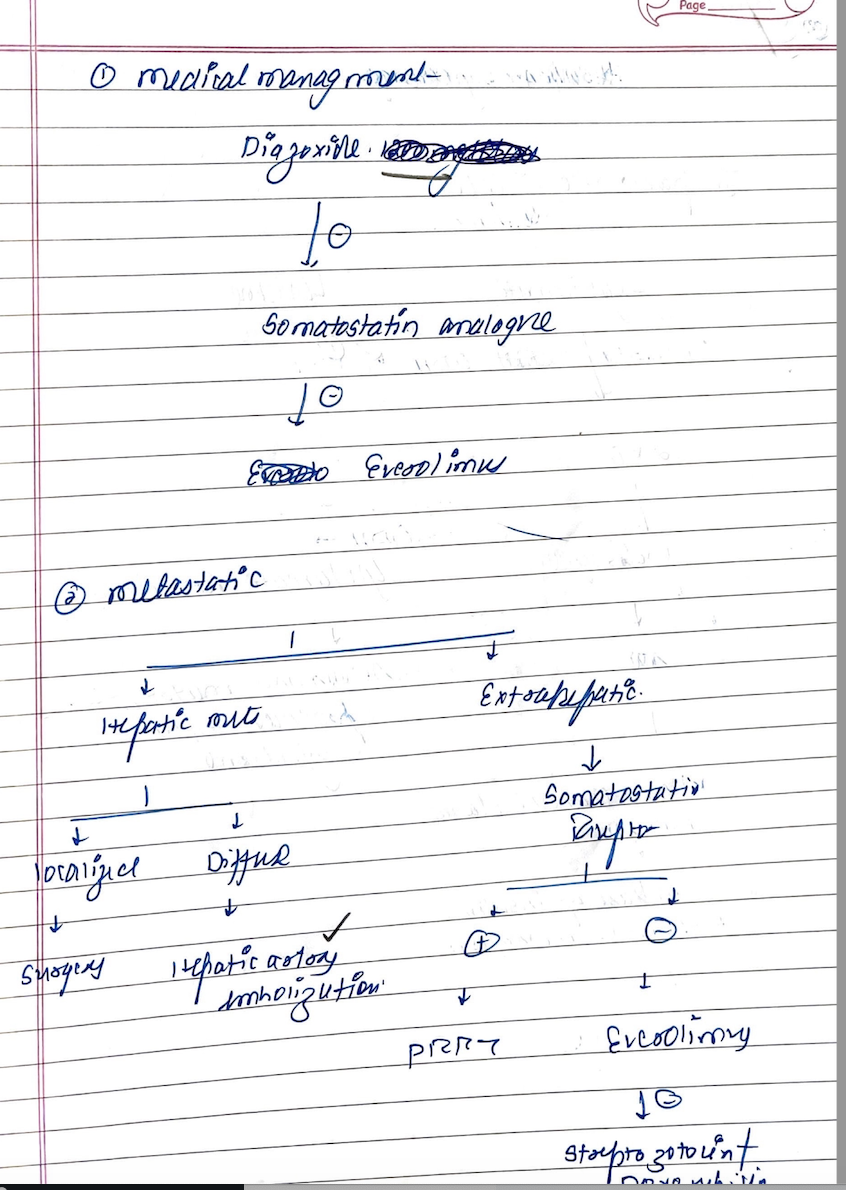
- Q. Summarize the management of insulinoma in Non-MEN1 cases.
- Q. What is the principle of hepatic artery embolization?
- Liver has a dual blood supply
- Normal liver tissue blood supply from the portal vein
- Metastasis → blood supply from hepatic artery
- Hence embolization of hepatic artery – cuts off supply to mets but maintains supply to hepatocytes
- #Updates Date April 10th, 2021
- Q. Which antiviral drug has been known to produce Hypoglycemia in patients not having diabetes?
- Oseltamivir has been known to produce Hypoglycemia in people not having diabetes, especially in the elderly
- This has been reported in the article by Kimberlin et al
- Ref: Kimberlin DW, Escude J, Gantner J, Ott J, Dronet M, Stewart TA, Jester P, Redden DT, Chapman W, Hammond R. Targeted antiviral prophylaxis with oseltamivir in a summer camp setting. Archives of pediatrics & adolescent medicine. 2010 Apr 5;164(4):323-7.
- Q. Which antiviral drug has been known to produce Hypoglycemia in patients not having diabetes?
- Exendin scan
- Q. What is the Exendin scan ?
- This is the PET scan done using Gallium-68 DOTA-Exendin-4 Positron Emission Tomography-Computed Tomography
- Q. What is the sensitivity of the current conventional imaging techniques for preop localization of Insulinoma?
- CT- 65-70%
- MRI- 55-65%
- Endoscopic ultrasound- 75-80%
- Q. What is the gold standard for preop localization of Insulinoma?
- Selective arterial calcium stimulation test
- Q. What is the basis for the Exendin scan?
- Insulinoma tends to have a high density of GLP-1 receptor
- This is detected with an Exendin scan
- Q. What is the correlation between the Exendin scan can Gallium DOTANOC scan?
- GLP1 receptors have high density in 95% of insulinoma
- Gallium DOTANOC picks up the SSTR2 receptor which is present in 70% of insulinoma
- Hence Exendin is more sensitive than DOTANOC for insulinoma
- However, in cases of Exendin negative- DOTANOC can be positive
- Q. Can Exendin scan have a false positive?
- This is very rare
- Q. What about the false negative?
- This is possible
-
- Insulinoma may have have no GLP1 receptor
- In this case, sometimes they may have SSTR2
- Hence Gallium DOTANOC can make a diagnosis
-
- Renal uptake can cause false negative
- Intense physiological renal uptake can cause reconstruction artifact which can cause false negative in the adjacent insulinoma in the tail of the pancreas
- Q. What is the common side effect during an Exendin scan?
- Exendin scan cause produce Hypoglycemia - some patients may have nausea and vomiting because of the same
- Q. If an insulinoma has already been detected by another imaging technique- what PET scan would you do to confirm the same?
- In this case, DOTANOC is preferred over Exendin because of the following reasons:
-
- If there is distant mets or poorly differentiated lesion- DOTANOC is more likely to pick up the diagnosis than exendin
-
- If required this can be used as a therapeutic agent (theranostic therapy) compared to Exendin which is not suitable as a theranostic agent