- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
Related video lectures
-
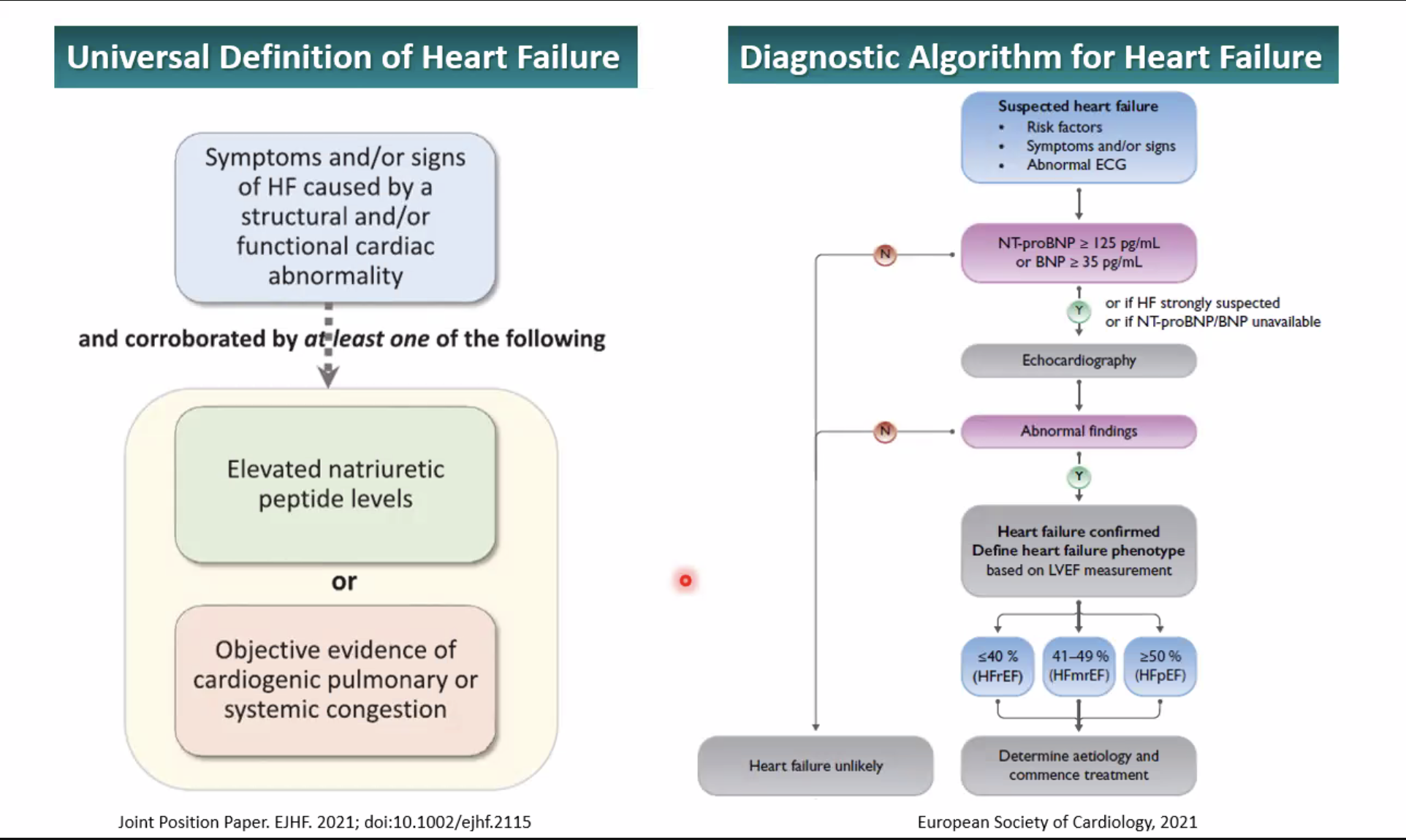
Q. What is the current definition and diagnostic algorithm for Heart failure ?
-
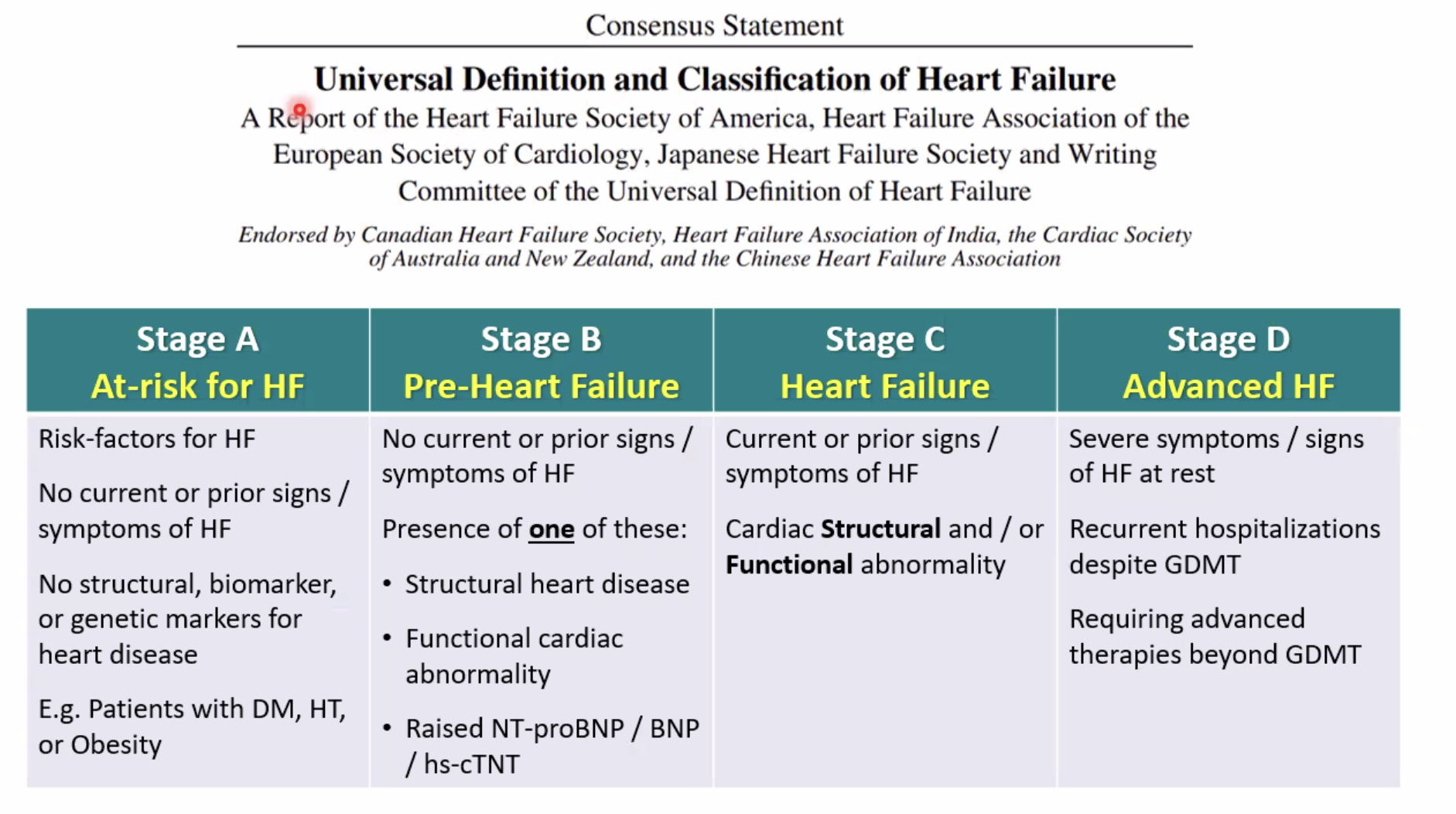
Q. What is the current staging recommended for Heart failure ?
-
Q. What percentage of patients with diabetes have LV diastolic dysfunction ?
- 46%
-
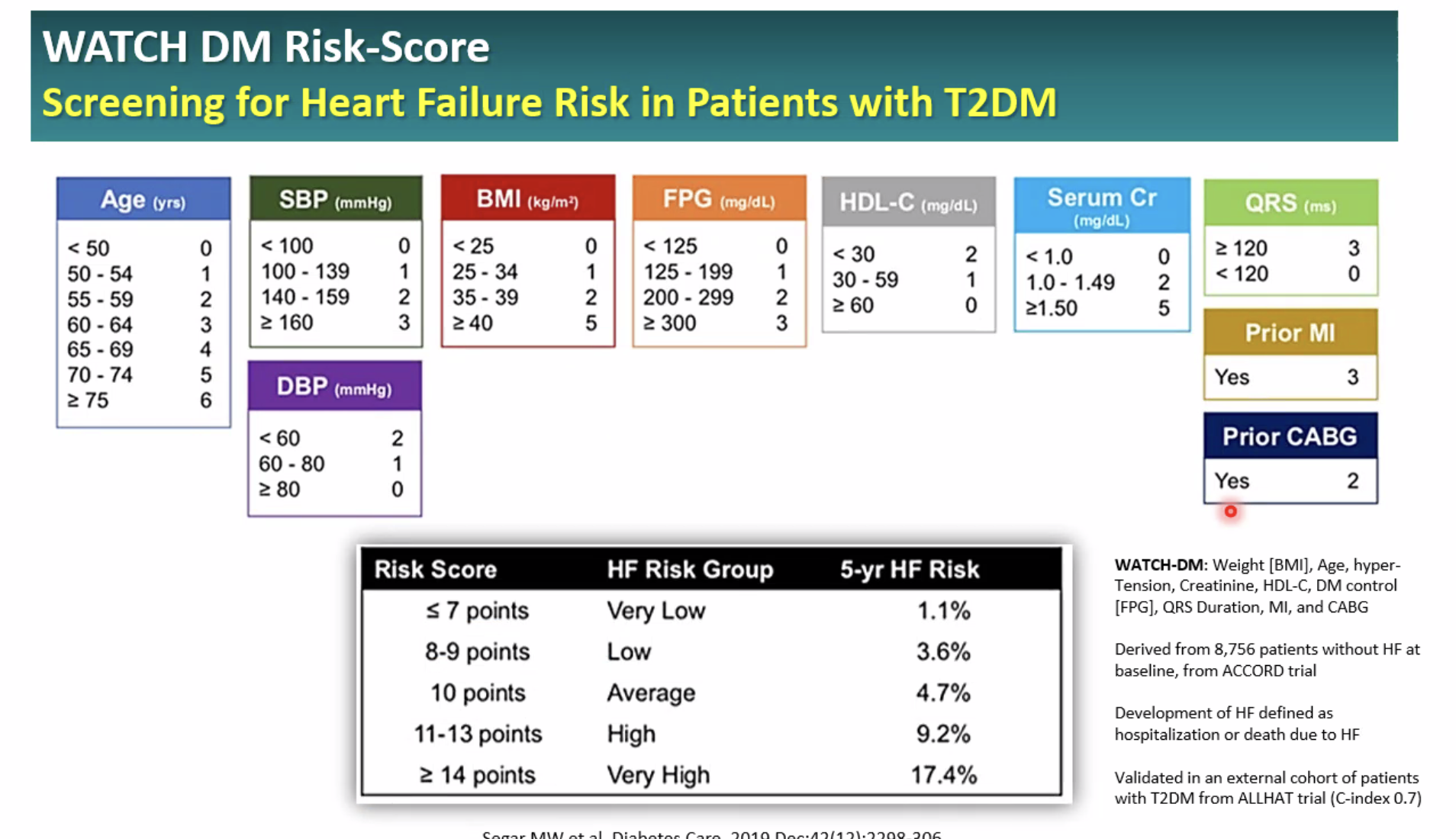
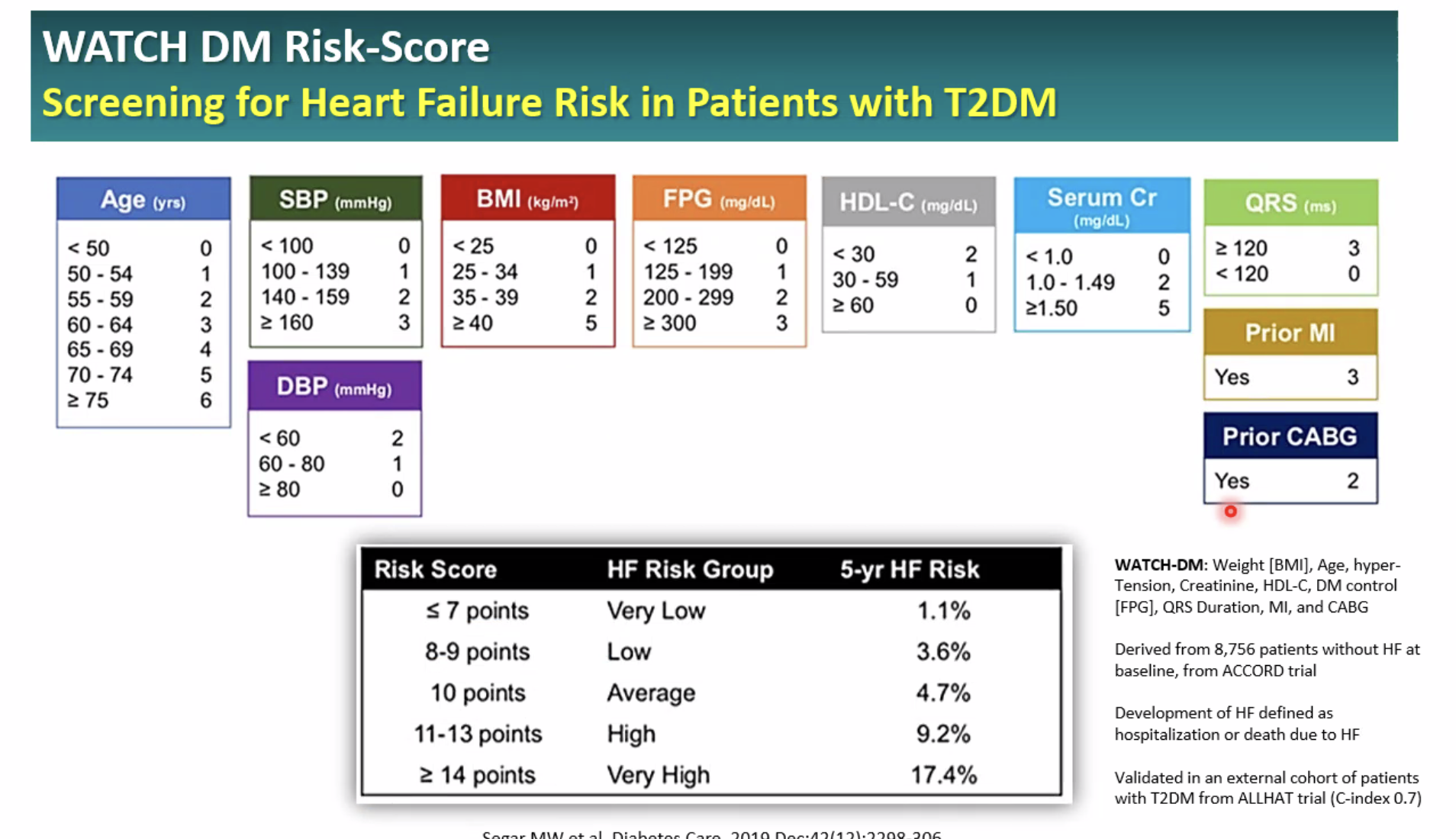
Q. What is the WATCH-DM score ?
- This is score used for looking for patients with diabetes with risk for Heart failure
-
Q. What are the current guidelines for using Natriuretic peptide measurement in heart failure ?
- NP should always be used in conjunction with all other clinical information
- Obese patients have lower NP levels, necessitating lower cut-off levels (by =50%)
- For patients with dyspnoea, NP testing has very high diagnostic accuracy
- NP testing has high prognostic accuracy for HF events, in patients with stable HF
- In patients with CV risk factors, screening with NP testing may help allow targeted measures to prevent development of HF
- BNP and NT-proBNP have comparable diagnostic and prognostic accuracy
-
Q. What is the current definition and diagnostic algorithm for Heart failure ?
-
Q. What is the current staging recommended for Heart failure ?
-
Q. What are the causes of heart failure due to diabetes ?
-
- CAD
- Uncontrolled diabetes
- Uncontrolled Hypertension
- Obesity
- Insulin resistance
-
- Diabetic cardiomyopathy
- Obesity
- Insulin resistance
- Uncontrolled diabetes
-
- Other causes of heart failure
-
-
Q. What percentage of patients with diabetes have LV diastolic dysfunction ?
- 46%
-
Q. What is the WATCH-DM score ?
- This is score used for looking for patients with diabetes with risk for Heart failure
-
Q. What is diabetic cardiomyopathy ?
- It is heart failure in patients with diabetes independent of CAD
-
Q. Who was the first to describe diabetic cardiomyopathy ?
- Rubber et al
-
Q. Define diabetic cardiomyopathy ?
- DCM is defined as the specific cardiac dysfunction and damage present in diabetic patients, which is characterized by myocardial dilatation, hypertrophy, and decreased left ventricular (LV) systolic and diastolic functions, and which is independent of the coexistence of ischemic heart disease, MI, or hypertension
-
Q. How common is heart failure in patients with diabetes ?
- According to Framingham heart study heat failure is 3.8 times more common in males and 5.5 times more common in females with diabetes than non diabetics
-
Q. Is there a link between glycemic control and heart failure ?
- For every 1 % increase in HbA1c there is 8% increase in heart failure
-
Q. What is the cause for edema due to TZD ?
- PPAR gamma increases sodium reabsorption via epithelial sodium channel- which causes edema
-
Q. What are the AHA guidelines on the use of pioglitazone in heart failure ?
- NYHA grade I and II- use maximum of 15 mg
- III and IV- contraindicated
-
Q. What is the impact of ACEI and ARB on heart failure and diabetes ?
- It reduces risk of hospitalization due to heart failure
-
Q. What is the characteristic pathological change in a patient with diabetic cardiomyopathy ?
- PAS-positive material in the myocardial interstitium
-
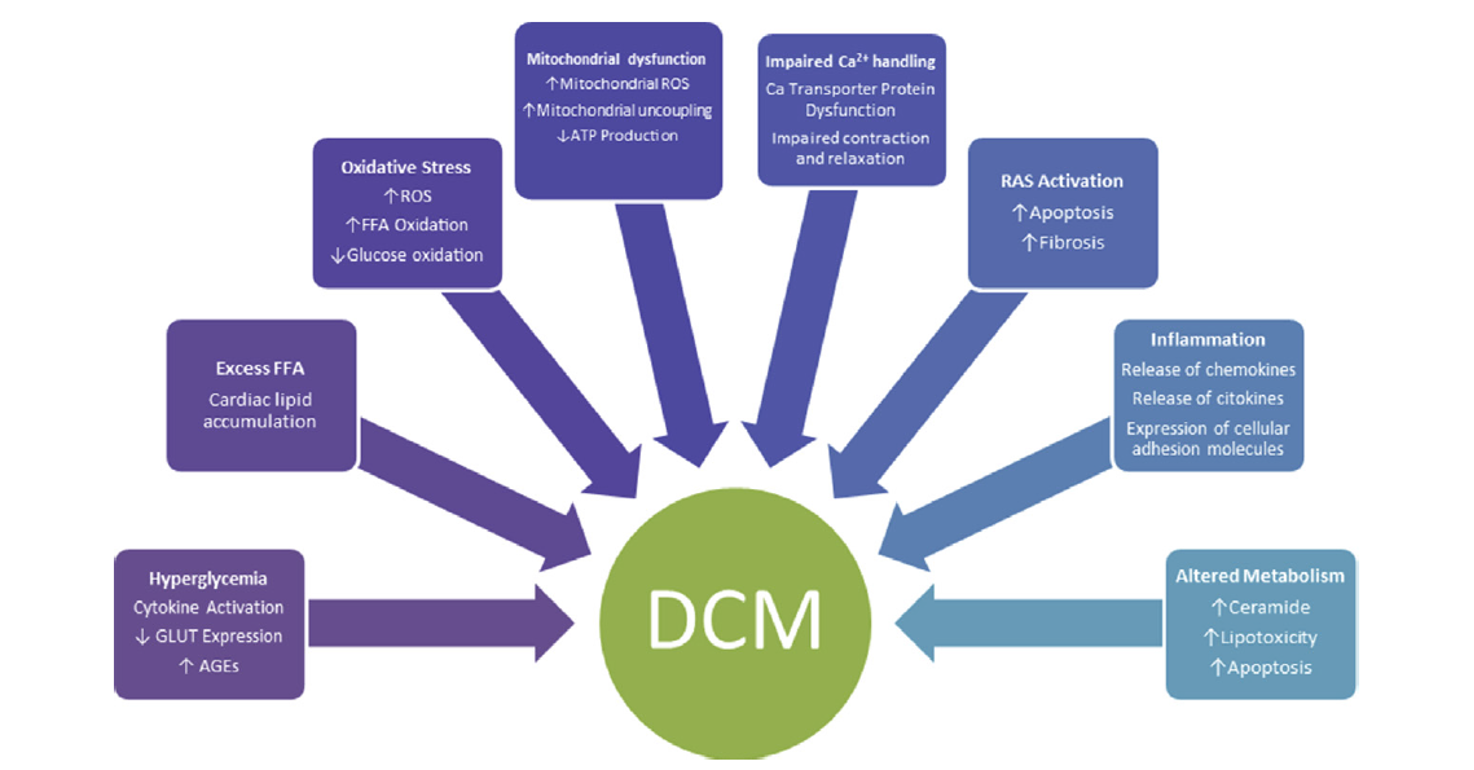
Q. What are the pathological mechanisms for diabetic cardiomyopathy ?
- Increase AGE in the heart tissue- increase thickness
- Endothelial dysfunction
- Autonomic dysfunction
- Intramyocardial microangiopathy
- Myocardial fibrosis
- Diabetic cardiomyopathy
-
Q. What is the impact of RAS system in DCM ?
- RAS system is activated in diabetics → increased endothelial apoptosis
- Increase angiotensin II receptors on the heart
-
Q. How common is cardiac autonomic neuropathy (CAN) in diabetics ?
- It is present in 20% of diabetics
-
Q. What is the clinical feature of CAN ?
- Increase resting heart rate is the most common clinical feature
-
Q. Does CAN impact DCM ?
- Resting tachycardia may impact LV systolic function and hence may be one of the reasons for DCM
-
Q. Why is there increase myocardial fibrosis in diabetics ?
- Glucose linking with Collagen → Glycated collagen → AGE → cross-link with collagen → increased myocardial fibrosis
-
Q. Summarize the pathogenesis of DCM ?
-
Q. What are the histopathological changes seen in DCM ?
- Increase myocardial thickness
- Capillary endothelial changes
- Thickening of capillary basement membrane
- Increase PAS-positive material
-
Q. What are the stages of diabetic cardiomyopathy ?
- Stage 1- Diastolic dysfunction alone without any other cardiac involvement
- Stage 2- Systolic + Diastolic involvement
- Stage 3- Systolic /Diastolic involvement in background of other cardiac-related issues like uncontrolled hypertension, microvascular disease , infection or inflammation
- Stage 4- Systolic/diastolic with CAD
-
Q. What is the hallmark of Diabetic cardiomyopathy on Echocardiography ?
- Cardiac hypertrophy and diastolic dysfunction
-
Q. How common is diastolic dysfunction in diabetics ?
- 75% of diabetics have dystolic dysfunction
-
Q. Which newer echo technique is useful for diagnosis DCM ?
- Total ejection isolvoluemic index (TEI) is useful for diagnosis of Diabetic cardiomyopathy
- Cardiovascular autonomic neuropathy
-
Q. What are the clinical features of CAN ?
- Postural hypotension
- Silent ischemia and infarction
- Resting tachycardia
- POTS- Postural orthostatic tachycardia syndrome
- Exercise intolerance
- Increased mortality
- Intraoperative CV instability
-
Q. What happens to sympathetic and parasympathetic tones in diabetics ?
- Sympathetic tone reduces at day time- postural hypotension
- Parasympathetic tone reduces at night time- failure of night-time dip of blood pressure
-
Q. What are the tests to detect parasympathetic tone ?
- Heart rate variability with respiration
- Heart rate variability with Valsalva
- 30:15 ratio
-
Q. Describe HR variability with respiration ?
- Measure ECG continuously
- Ask patient for deep inspiration and expiration during ECG monitoring
- Measure the shortest RR interval during inspiration and longest in expiration
- Convert it to Beats per minute
- Difference >15 BPM- normal, <10 abnormal
- Pearl
- Normally HR increases in inspiration
-
Q. Describe the 30:15 ratio ?
- Continuous ECG monitor
- Ask patient to stand up from supine
- Measure the shortest RR interval at 15 beat and longest at 30 beat
- Take ratio of this
- More than 1.04 normal
- <1.0- abnormal
-
Q. Describe HR variability with vaslva ?
- Continuous ECG monitor
- Ask patient to blow against sphygmomanometer at 40 mm Hg for 15 s
- Then release and continue monitoring ECG fo 30 s
- Take the longest RR on release / Shortest RR during vaslva
- Ratio >1.2- normal
- <1.0- abnormal
-
Q. Describe the tests for the sympathetic system ?
- Postural hypotension test
- BP Response to handgrip
- Postural hypotension- measure BP in supine after 5 min of rest- measure BP in standing after 5 min
- SBP >20 mm Hg and DBP >10 mm Hg – s/o of Postural hypotension
- Handgrip
- Ask patient to squeeze inflated BP cuff
- Measure DBP before and after
- Difference >16 mm Hg- normal , <10 mm Hg- Abnormal
- Postural hypotension test
-
Q. Describe the non pharmacological techniques for CAN ?
- Get up from bed slowly
- Cross leg while standing
- Change posture slowly
- Elevate head end of bed by 30 degree while sleeping
-
Q. which are drugs used in treatment of CAN ?
- Fludrocortisone
- Midodrine
- Pindolol
- Fluoxetine
- Desmopressin
-
Q. How common is QT prolongation and what is it’s importance ?
- QT prolongation seen in 16% cases
- Risk of arrhythmia
-
Q. What are direct tests for CAN ?
- I123 MING
- C11 hydroxyepiderine scintigraphy
-
Q. Do patients with DM have increased Heart attack during morning time ?
- No
- There is a loss of circadian rhythm
-
Q. What is the importance of QT dispersion ?
- QT dispersion can be means of quantifying CAN
- It is longest QT interval – shortest QT interval
- The longer the difference- worse the CAN and prognosis
-
Q. What are the current guidelines for using Natriuretic peptide measurement in heart failure ?
- NP should always be used in conjunction with all other clinical information
- Obese patients have lower NP levels, necessitating lower cut-off levels (by =50%)
- For patients with dyspnoea, NP testing has very high diagnostic accuracy
- NP testing has high prognostic accuracy for HF events, in patients with stable HF
- In patients with CV risk factors, screening with NP testing may help allow targeted measures to prevent development of HF
- BNP and NT-proBNP have comparable diagnostic and prognostic accuracy
-
Q. Does NTproBNP play a major role in the prognosis of patients with diabetes and HFrEF?
- Yes it does
- In patients with Chronic heart failure, these peptides give important prognostic information
- "Every 100 pg/mL increase in plasma BNP was associated with a 35 percent increase in the relative risk of death"
- It is a better predictor of death as compared to LVEF measurement of NYHA grading
- If the levels are high despite treatment- that again is a predictor or death and prognosis
- Subaalysis of COPERNICUS Trial concludes :
- NT-proBNP was consistently associated with increased risk for all-cause mortality and for all-cause mortality or hospitalization for heart failure in patients with severe congestive heart failure, even in those who were clinically euvolemic
- An article titled The prognostic value of troponin T and N-terminal pro B-type natriuretic peptide, alone and in combination, in heart failure patients with and without diabetes which is a sub-analysis of the PARADIGM-HF trial says:
- "Thus, patients with diabetes, an elevated TnT and a NT-proBNP level in the highest tertile (9% of all patients) had an absolute risk of cardiovascular death or heart failure hospitalization of 265 per 1000 person-years, compared to a rate of 42 per 1000 person-years in those without diabetes, a TnT < 18 ng/L and a NT-proBNP in the lowest tertile (16% of all patients)"
-
Management of heart failure in Diabetes
-
Q. Is there are role of exercise in patients with Heart failure and diabetes ?
- Yes
- Exercise improves functional capacity of these patients
-
Q. Which are the various pharmacological agents for use in patients with HFrEF with Diabetes ?
-
- ACER/ARB
-
- Beta-blockers
-
- Diuretics
-
- MR antagonist
-
- SGLT2i
-
- Ivabradine
-
- Hydralazine
-
-
Q. Which beta-blocker is preferred in patients with Diabetes ?
- Carvedilol
- It has favorable effect on glycemic control
-
Q. Between Spironolactone and Eplerenone which should be preferred in patients with diabetes ?
- Trials have shown slight increase of HbA1c in patients on spironolactone as compared to Eplerenone
-
Q. What drugs are useful in patients with HFpEF ?
- Mineralocorticoid receptor antagonist
- SGLT2i
Role of SGLT2i in patients with Diabetes mellitus and heart failure
- Q. How do SGLT2i show benefit in Heart failure ?
- POTENTIAL MECHANISMS
-
- Stimulation of natriuresis
-
- Stimulation of osmotic diuresis
-
- Cardiomyocyte Na+/H exchanger inhibition
-
- Increased myocardial energetics (via altered myocardial substrate metabolism)
-
- Reduction in left ventricular mass
-
- Improved systolic and diastolic function
-
- Improved cardiac filling conditions secondary to reductions in preload and afterload
-
- Increased circulating proangiogenic progenitor cells
-
- Increased erythropoietin
-
- Improved endothelial function
-
- Reduction in myocardial CaM kinase II activity
-
- Improved myocardial autophagy
-
- Inhibition of cardiac fibrosis
-
- Increased cardiac output, HR, O2 consumption, coronary blood flow mediated by increased levels of circulating glucagon

-
- POTENTIAL MECHANISMS
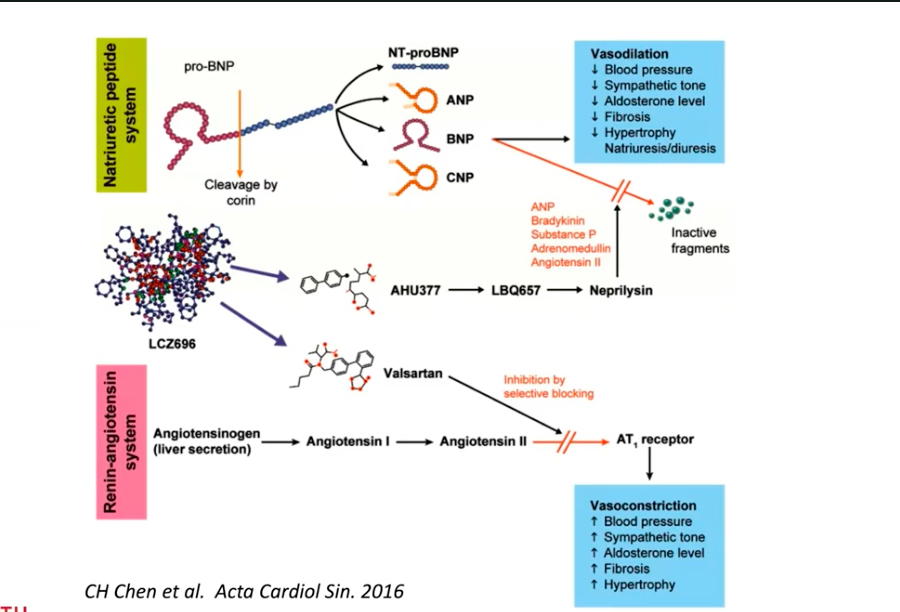
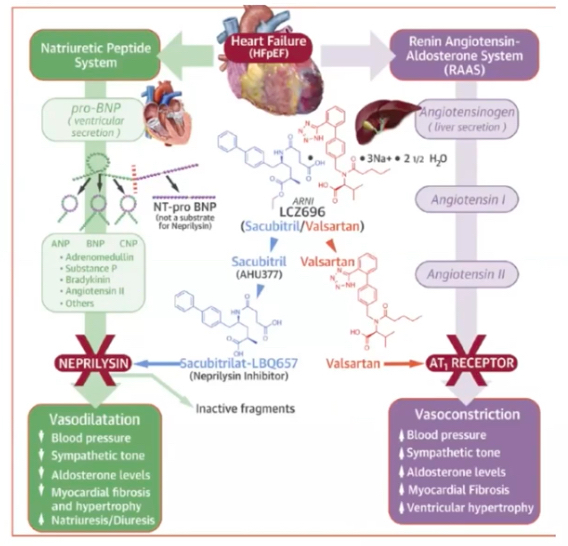
Role of ARNI in patients with diabetes and heart failure (SACUBITRIL/VALSARTAN)
-
Q. What is the evidence of the benefit of SACUBITRIL/VALSARTAN for diabetes control ?
- In the PARADIGM-HF trial at one year follow-up SACUBITRIL/VALSARTAN group had lower HbA1c by 13% and at 2 years , 17 % . Overall 14% lower HbA1c
-
Q. Does SACUBITRIL/VALSARTAN reduce the NT-pro-BNP levels ?
- Yes
- Study by Packer et al has shown that there is 25% reduction in NT-proBNP level with sacubitril/valsartan compared to enalapril in patients with diabetes and HFrEF
-
Q. What is the impact of SACUBITRIL/VALSARTAN on glycaemic
control and use of insulin in patients with diabetes and HFrEF?- ^[1] is an enzyme which cleaves many peptides^^
- ^^One of the peptides it cleaves is GLP-1^^
- ^^Hence neprilysin inhibiton can also increase of GLP1 leading to its beneficial effects just like DPP-4 inhibitors ^^
- ^^also it increases Bradykinin which also reduces Insulin resistance ^^
- ^^increases Adiponectin and hence cause weight loss^^
- ^^It can increase Angiotensin II which can have negative connotations hence it is advised to combine with ARB^^
- ^^it can increase the levels of IAPP, which can cause beta-cell depletion over time^^
- ^^Hence long term benefits on glycemic control are not known^^
-
Q. Can BNP be used as a biomarker in patients on treatment with ARNI / SACUBITRIL/VALSARTAN ?
- No
- But NT-pro-BNP can be used
-
Q. How Does ARNI work in Heart failure
-
-
Q. With SGLT2i showing promise in HF patients, is there any evidence for use of SGLT2i and ARNI together in HFrEF patients?
- This question is comprehensively answered by a study by Muthiah Vaduganathan et al published in The Lancet in 2020
- In this study, they did a subanalysis of patients receiving all 3 disease-modifying agents- MRA, ARNI, SGLT2 versus conventional therapy of ARB/ACEI and beta-blockers from three largest recent trials EMPHASIS-HF (n=2737), PARADIGM-HF (n=8399), and DAPA-HF (n=4744).
- The study found incremental benefit of in the form of reduction in heart failure admission and reduction in death due to heart failure
- There was also significant survival benefit
- Treatment with comprehensive disease-modifying pharmacological therapy was estimated to afford
- Admission free interval
- 2·7 additional years (for an 80-year-old)
- 8·3 additional years (for a 55-year-old) free from cardiovascular death or first hospital admission for heart failure
- Survival benefit
- 1·4 additional years (for an 80-year-old)
- 6·3 additional years (for a 55-year-old) of survival compared with conventional therapy.
- Admission free interval
- Treatment with comprehensive disease-modifying pharmacological therapy was estimated to afford
20-Jun-2023 UPDATES
- Q. Does glycemic control improve the outcome for heart failure in patients with type 2 diabetes ?
- This is an area of debate
- Per se glycemic control alone does not improve outcomes in heart failure
- Intensive glycemic control has no significant impact on the risk of heart failure in type 2 diabetic patients, as evidenced by a meta-analysis of 37,229 patients (Castagno et al., 2011).
- The relationship between glycemic control and heart failure was studied in 83,021 patients with type 2 diabetes, and no strong association was found (Lind et al., 2012).
- ACCORD, ADVANCE, and VA diabetes trials also suggest that intensive glycemic control does not significantly prevent cardiovascular events (American Diabetes Association, American College of Cardiology Foundation, American Heart Association, 2009).
- However, EMPA-REG OUTCOME trial showed that empagliflozin, an SGLT2 inhibitor, improved cardiovascular outcomes and reduced mortality in type 2 diabetes patients, indicating that specific glucose-lowering medications might have a positive impact on heart failure outcomes (Zinman et al., 2015).
- Q. True or false, diabetes leads to heart failure and heart failure leads to diabetes ?
- True: Diabetes can lead to heart failure. Patients with diabetes have a higher risk of developing heart failure due to factors such as insulin resistance, hyperglycemia, and increased inflammation (Seferović et al., 2018; Cavender et al., 2015).
- True: Heart failure can lead to diabetes. Heart failure is associated with an increased risk of developing diabetes, possibly due to factors such as impaired glucose metabolism, increased insulin resistance, and neurohormonal activation (Guglin et al., 2014).
- Q. How does cardiac sympathetic activation in diabetes patients with autonomic neuropathy contribute to heart failure ?
- Cardiac sympathetic system activation: In diabetes, the sympathetic nervous system (SNS) is often overactivated, leading to increased catecholamine release and reduced norepinephrine reuptake (Vinik et al., 2003; Maser et al., 2000).
- Myocardial dysfunction: Overactivation of the SNS contributes to myocardial dysfunction, including impaired contractility, relaxation, and diastolic filling (Boudina et al., 2007).
- Increased heart rate: SNS overactivation results in an increased heart rate, which can further exacerbate heart failure by increasing myocardial oxygen demand and reducing diastolic filling time (Boudina et al., 2007).
- Cardiac remodeling: Chronic SNS activation promotes cardiac remodeling, including myocardial hypertrophy, fibrosis, and apoptosis, which can lead to heart failure (Cohn et al., 2000).
- Arrhythmias: SNS overactivation increases the risk of arrhythmias, which can worsen heart failure and increase the risk of sudden cardiac death (Zipes et al., 1998).
- RAAS activation: SNS overactivation also stimulates the renin-angiotensin-aldosterone system (RAAS), leading to vasoconstriction, sodium retention, and fluid overload, further contributing to heart failure (Cohn et al., 2000).
- Q. With diagrams, explain the pathophysiology of Diabetic cardiomyopathy
[neprilysin|neprilysin] ↩︎