- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
-
Q. What are the characteristic features of the lipoprotein components of Diabetic Dyslipidemia ?
- Small Dense LDL-C
- Increased triglyceride
- Reduced HDL
- Increased VLDL produced by the liver
-
Q. What are the characteristics of LDL particle in diabetes mellitus ?
- The LDL particles tend to be
- Small
- Dense
- More Triglyceride rich
- More prone to oxidation
- Glycated LDL
- Increased Hepatic LDL
- The LDL particles tend to be
-
Q. Why does the glycation in LDL create a problem ?
- Because of the glycation of the LDL particle, the particle is NOT recognized by the LDL receptors
- This increases the half-life of the LDL particles in circulation
-
Q. Describe the pathogenesis of Diabetic Dyslipidemia ?
- See the video
-
Q. Does Weight loss improve lipid profile ?
- Yes
- Weight loss does lead to improvement in lipid profile
- Weight Loss and Serum Lipids in Overweight and Obese Adults: A Systematic Review and Meta-Analysis
- Lifestyle interventions (diet, exercise, or both), pharmacotherapy, and bariatric surgery were associated with reduced triglyceride (TG) and low-density lipoprotein cholesterol (LDL-C-C) concentrations and increased high-density lipoprotein cholesterol (HDL-C) at 6 and 12 months Lifestyle measures
- Following lifestyle interventions, per 1 kg of weight lost, TGs were reduced by –4.0 mg/dL (95% CI, –5.24 to –2.77 mg/dL), LDL-C was reduced by –1.28 mg/dL (95% CI, –2.19 to –0.37 mg/dL), and HDL-C increased by 0.46 mg/dL
- Low-carbohydrate diet resulted in reductions in TGs and increases in HDL-C, whereas low-fat diets resulted in reductions in TGs and LDL-C and increases in HDL-C
- Weight loss in adults is associated with statistically significant changes in serum lipids. The reported magnitude of improvement can help in setting expectations, inform shared decision making, and facilitate counseling.
- I^^n Short- Weight loss DOES lead to change in lipid profile including improvement in LDL levels ^^ #ClinicalPearl
-
Q. What is the impact of SGLT2i on the lipid profile and Diabetic Dyslipidemia ? #ClinicalPearl
- SGLT2i - Increased LDL-C
- Reduces triglyceride
- Reference
- Mechanism of increased LDL and decreased triglycerides with SGLT2 inhibition
- Sodium-glucose cotransporter 2 (SGLT2) inhibition in humans leads to increased levels of LDL cholesterol and decreased levels of plasma triglyceride
- Mechanism of increased LDL and decreased triglycerides with SGLT2 inhibition
-
Q. What are the dietary recommendations for a patient with diabetic dyslipidemia ?
- Mediterranean diet
- Dietary Approaches to Stop Hypertension (DASH) eating pattern
- reducing saturated and trans fat intake
- increasing plant stanols/sterols
- increasing n-3 fatty acids
- increasing viscous fiber (such as in oats, legumes, and citrus) intake
-
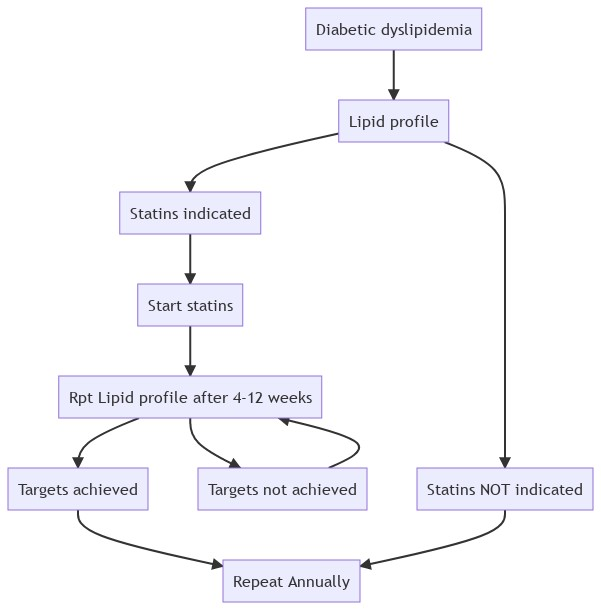
Q. How frequently should a lipid profile be done in a patient with diabetes ?
- At the time of initial diagnosis / evaluation
- Every 5 years for patients <40 years of age
-
Q. How frequently should lipid profile be done in patients on treatment with statins for diabetic dyslipidemia ?
-
-
Primary prevention
-
Q. What do the ADA guidelines have to say about the use of statins in patients living with diabetes for primary prevention ?
- All patients with diabetes who are more than 40 years of age must receive at least moderate-intensity statin therapy for primary prevention
- Some patients may need high intensity statin therapy
-
Q. What is the definition of moderate intensity and high intensity statins ?
- Moderate intensity - Reduces LDL by 30-50% from baseline
- Atorvastatin 10-20 mg
- Rosuvastatin 5-10 mg
- Simvastatin 20-40 mg
- Pravastatin 40-80 mg
- Lovastatin 40 mg
- Fluvastatin XL 80 mg
- Pitavastatin 1-4 mg
- High intensity - Reduces LDL by more than 50% from baseline
- Atorvastatin 40-80 mg
- Rosuvastatin 20-40 mg
- Moderate intensity - Reduces LDL by 30-50% from baseline
-
Q. Should patients with diabetes more than 75 years of age be given statins ?
- Most clinical trials have excluded this group of individuals.
- Hence the data available with us is NOT sufficient
- However, extending the benefits from the lower age group, it is reasonable to conclude that these group of patients would benefit from statin therapy
- Moderate-intensity statin therapy is recommended in patients with diabetes who are 75 years or older as per the ADA guidelines
-
Q. What about those less than 40 years of age ?
- For primary prevention in this group the data is limited
- However, it is reasonable to consider that amongst this group if there is high cardiovascular risk, statin therapy must be started
-
Q. Do very low doses of statins also have benefit ?
- Yes
- There is evidence to suggest that even low and suboptimal statin doses have some clinical benefit
- Daily and intermittent rosuvastatin 5 mg therapy in statin-intolerant patients: an observational study - PubMed
- In this retrospective observational multicentre study, rosuvastatin 5 mg was found to be safe and biochemically effective either as daily or intermittent therapy in patients intolerant to other conventional statin regimens.
-
Q. How much risk reduction of cardiovascular disease is seen in patients with Diabetic Dyslipidemia for every 39 mg/dl or 1 mmol/l reduction of LDL ?
- 9% reduction in All-cause mortality
- 13% reduction in vascular mortality
- This is from the Cholesterol Treatment Trialists' (CTT) Collaborators
-
Q. What were the results of the Cholesterol Treatment Trialists' (CTT) Collaborators meta-analysis ?
- This is a meta-analysis of 27 trials of more than 100,000 patients followed up for about 5 years
- The main conclusion of this study was that even in patients with perceived low baseline risk, the benefit of statin therapy was similar to patients with high baseline risk
- These were the results from the trial
- Reduction of LDL cholesterol with a statin reduced the risk of major vascular events (RR 0·79, 95% CI 0·77-0·81, per 1·0 mmol/L reduction), largely irrespective of age, sex, baseline LDL cholesterol or previous vascular disease, and of vascular and all-cause mortality.
- ^^The proportional reduction in major vascular events was at least as big in the two lowest risk categories as in the higher risk categories (RR per 1·0 mmol/L reduction from lowest to highest risk^^: 0·62 [99% CI 0·47-0·81], 0·69 [99% CI 0·60-0·79], 0·79 [99% CI 0·74-0·85], 0·81 [99% CI 0·77-0·86], and 0·79 [99% CI 0·74-0·84]; trend p=0·04), which reflected significant reductions in these two lowest risk categories in major coronary events (RR 0·57, 99% CI 0·36-0·89, p=0·0012, and 0·61, 99% CI 0·50-0·74, p<0·0001) and in coronary revascularisations (RR 0·52, 99% CI 0·35-0·75, and 0·63, 99% CI 0·51-0·79; both p<0·0001).
- For stroke, the reduction in risk in participants with 5-year risk of major vascular events lower than 10% (RR per 1·0 mmol/L LDL cholesterol reduction 0·76, 99% CI 0·61-0·95, p=0·0012) was also similar to that seen in higher-risk categories (trend p=0·3).
- In participants without a history of vascular disease, statins reduced the risks of vascular (RR per 1·0 mmol/L LDL cholesterol reduction 0·85, 95% CI 0·77-0·95) and all-cause mortality (RR 0·91, 95% CI 0·85-0·97), and the proportional reductions were similar by baseline risk.
- There was no evidence that reduction of LDL cholesterol with a statin increased cancer incidence (RR per 1·0 mmol/L LDL cholesterol reduction 1·00, 95% CI 0·96-1·04), cancer mortality (RR 0·99, 95% CI 0·93-1·06), or other non-vascular mortality.
-
Q. What does the 4S Trial for simvastatin have to say about the use of statins for Diabetic Dyslipidemia ?
- Cholesterol Lowering With Simvastatin Improves Prognosis of Diabetic Patients With Coronary Heart Disease: A subgroup analysis of the Scandinavian Simvastatin Survival Study (4S) | Diabetes Care
- Over the 5.4-year median follow-up period, simvastatin treatment produced mean changes in serum lipids in diabetic patients similar to those observed in nondiabetic patients.
- The relative risks (RRs) of main endpoints in simvastatin-treated diabetic patients were as follows: total mortality 0.57 (95% CI, 0.30–1.08; P = 0.087), major CHD events 0.45 (95% CI, 0.27–0.74; P = 0.002), and any atherosclerotic event 0.63 (95% CI, 0.43–0.92; P = 0.018).
- The corresponding RRs in nondiabetic patients were the following: 0.71 (95% CI, 0.58–0.87; P = 0.001), 0.68 (95% CI, 0.60–0.77; P < 0.0001), and 0.74 (95% CI, 0.68–0.82; P < 0.0001).
- CONCLUSIONS The results strongly suggest that cholesterol-lowering with simvastatin improves the prognosis of diabetic patients with CHD.
- The absolute clinical benefit achieved by cholesterol-lowering may be greater in diabetic than in nondiabetic patients with CHD because diabetic patients have a higher absolute risk of recurrent CHD events and other atherosclerotic events.
- Cholesterol Lowering With Simvastatin Improves Prognosis of Diabetic Patients With Coronary Heart Disease: A subgroup analysis of the Scandinavian Simvastatin Survival Study (4S) | Diabetes Care
-
Q. What were the conclusion from the MRC/BHF Heart Protection Study of cholesterol ?
- MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial - PubMed
- The present study provides direct evidence that cholesterol-lowering therapy is beneficial for people with diabetes even if they do not already have manifest coronary disease or high cholesterol concentrations.
- Allocation to 40 mg simvastatin daily reduced the rate of first major vascular events by about a quarter in a wide range of diabetic patients studied. After making allowance for non-compliance, actual use of this statin regimen would probably reduce these rates by about a third.
- For example, among the type of diabetic patient studied without occlusive arterial disease, 5 years of treatment would be expected to prevent about 45 people per 1000 from having at least one major vascular event (and, among these 45 people, to prevent about 70 first or subsequent events during this treatment period).
- Statin therapy should now be considered routinely for all diabetic patients at sufficiently high risk of major vascular events, irrespective of their initial cholesterol concentrations.
- MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial - PubMed
-
Q. What were the results from the CARE trial ?
- Cardiovascular Events and Their Reduction With Pravastatin in Diabetic and Glucose-Intolerant Myocardial Infarction Survivors With Average Cholesterol Levels | Circulation
- Pravastatin treatment reduced the absolute risk of coronary events for the diabetic and nondiabetic patients by 8.1% and 5.2% and the relative risk by 25% (P=0.05) and 23% (P<0.001), respectively.
- Pravastatin reduced the relative risk for revascularization procedures by 32% (P=0.04) in the diabetic patients.
- In the 3553 patients who were not diagnosed as diabetic, 342 had impaired fasting glucose at entry defined by the American Diabetes Association as 110 to 125 mg/dL.
- These nondiabetic patients with impaired fasting glucose had a higher rate of recurrent coronary events than those with normal fasting glucose (eg, 13% versus 10% for nonfatal MI). Recurrence rates tended to be lower in the pravastatin compared with the placebo group (eg, –50%, P=0.05 for nonfatal MI).
- Cardiovascular Events and Their Reduction With Pravastatin in Diabetic and Glucose-Intolerant Myocardial Infarction Survivors With Average Cholesterol Levels | Circulation
-
Secondary prevention
-
Q. What is the ADA recommendation for statin use in diabetes mellitus patients with pre-existing CAD ?
- ADA recommends high intensity statin to all these patients
-
Q. Where does the evidence of the same emerge from ?
- The evidence comes from Cholesterol Treatment Trialists' (CTT) Collaborators meta-analaysis
- In this trial intensive statin use was more preventive then moderate statin dose
-
Q. Is there any other independent study that compares intensive statin therapy versus moderate dose in patients post CAD ?
- Yes
- This data comes from Cannon et al from the TIMI study group
- In this they compared 40 mg of pravastatin daily (standard therapy) with 80 mg of atorvastatin daily (intensive therapy)
- This was the conclusion
- Intensive versus moderate lipid lowering with statins after acute coronary syndromes - PubMed
- ^^Among patients who have recently had an acute coronary syndrome, an intensive lipid-lowering statin regimen provides greater protection against death or major cardiovascular events than does a standard regimen.^^
- These findings indicate that such patients benefit from early and continued lowering of LDL cholesterol to levels substantially below current target levels.
- Intensive versus moderate lipid lowering with statins after acute coronary syndromes - PubMed
-
Q. Has adding non-statin agent to statin in these group of patients have any help ?
- Yes
- Several trials over the years have shown incremental benefit of adding non-statin therapy to further lower the LDL
- The lower the LDL, less the cardiovascular risk
-
Q. Where does the evidence for ezetimibe come from ?
- This comes from the IMPROVE-IT trial
- Here the Simvastatin was compared to Simvastatin + Ezetimibe
- the mean LDL at the start of the trial was 94 mg/dl
- On treatment the Ezetimibe group the LDL reduced to 53 while it reduced to 70 in the other arm
- There was 2% absolute risk reduction in the event rate in the ezetimibe group
- NNT = 50 patients for 7 years to prevent 1 event
- There was no difference in CV mortality, but there was difference in event rate
-
Q. Is there a subgroup analysis of patients living with diabetes in the IMPROVE-IT trial ?
- Yes
- About 27% of the participants in the trial had diabetes mellitus
- In this group there was 5% absolute and 14% relative risk reduction in the ezetimibe group
-
Q. What trial evaluated the use of PCSK9 inhibitors in the prevention of Cardiovascular disease ?
- The FOURIER Trial
- This trial was done for patients with baseline LDL of 70 already on statins
- This compared the use of evolocumab versus placebo
- the mean duration of follow-up was 2.2 years
- The results were suggested about 15% relative risk reduction of the primary endpoints of cardiovascular death, myocardial infarction, stroke, hospitalization for unstable angina, or coronary revascularization and 20% relative risk reduction of secondary en points which were cardiovascular death, myocardial infarction, or stroke
- Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease - PubMed
- Relative to placebo, evolocumab treatment significantly reduced the risk of the primary end point (1344 patients [9.8%] vs. 1563 patients [11.3%]; hazard ratio, 0.85; 95% confidence interval [CI], 0.79 to 0.92; P<0.001) and the key secondary end point (816 [5.9%] vs. 1013 [7.4%]; hazard ratio, 0.80; 95% CI, 0.73 to 0.88; P<0.001).
- The results were consistent across key subgroups, including the subgroup of patients in the lowest quartile for baseline LDL cholesterol levels (median, 74 mg per deciliter [1.9 mmol per liter]).
- Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease - PubMed
- Similar results were obtained from the ODYSSEY OUTCOMES trial which used Alirocumab
-
Treatment of other lipoprotein fractions and targets
-
Q. What does the guidelines say with regards to treatment of hypertriglyceridemia ?
- Fasting triglyceride
- More than 1000 mg/dl - Treat
- 500-1000 mg/dl - consider treatment
- 150-499 mg/dl
- Rule out secondary causes
- Lifestyle intervention
- Avoid medications that may increase triglyceride levels
- Fasting triglyceride
-
Q. Discuss the results of the REDUCE-IT trial ?
-
Q. What was the dose of Icosapent Ethyl used in this trial ?
- 2 gram twice a day
-
Q. Is there any benefit of combination of statins with fenofibrate ?
- This combination is not very popular now because of the increased risk of complications associated with the same namely
- Rhabdomyolysis
- Transaminitis
- Myositis
- In one sub-group it may reduce cardiovascular risk namely
- Men
- TG > 204 mg/dl
- HDL <34 mg/dl
- This combination is not very popular now because of the increased risk of complications associated with the same namely
-
Q. What is the impact of fenofibrate of the risk of developing CKD ?
- In a recent study published in JCEM, the use of fenofibrate was shown to reduce the need for dialysis and provides CV protection in patients with advanced CKD
- Fenofibrate Delays the Need for Dialysis and Reduces Cardiovascular Risk Among Patients With Advanced CKD | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic
- Fenofibrate provides limited cardiovascular (CV) benefits in the general population; however, little is known about its benefit among advanced chronic kidney disease (CKD) patients.
- The fenofibrate and statin groups exhibited a lower risk of CV death (fenofibrate vs nonuser: hazard ratio [HR]: 0.84; 95% CI, 0.75-0.94; statins vs nonuser: HR: 0.94; 95% CI, 0.90-0.97) compared with the nonuser group.
- ^^The fenofibrate group further exhibited the lowest incidence of permanent dialysis ^^
- Furthermore, the combined administration of fenofibrate and high-intensity statins exhibited a lower risk of major adverse cardiac and cerebrovascular events.
- ^^For patients with advanced CKD, continuing fenofibrate may provide a protective effect on CV outcomes equal to that of statins, and it may further delay the need for permanent dialysis^^