- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
- Q. What are the three main aspects of management of Diabetic neuropathy ?
- Glycemic control
- Foot care
- Treatment of pain
- **Glycemic control **
- Q. Does glycemic control IMPROVE diabetic neuropathy?
- This is an area of debate
- Many studies including DCCT have shown objective improvement in glycemic control including improvement in VPT and NCV
- At present, however, it is believed that once established, diabetic neuropathy cannot be reversed and only progression can be halted by good glycemic control
- Q. What type of neuropathy can be corrected with glycemic control alone?
- Acute painful diabetic neuropathy and rapidly reversible hyperglycemic neuropathy – can be corrected with glycemic control alone
- However, in some cases, rapid improvement in glycemic control can lead to "insulin neuritis"
- Hence stable glycemia is the aim not under or overtreatment
- **Foot care **
- Q. What are the components of foot care for diabetics?
- Daily inspection of feet by patients
- Physician inspection on regular visits
- **Management of painful diabetic neuropathy **
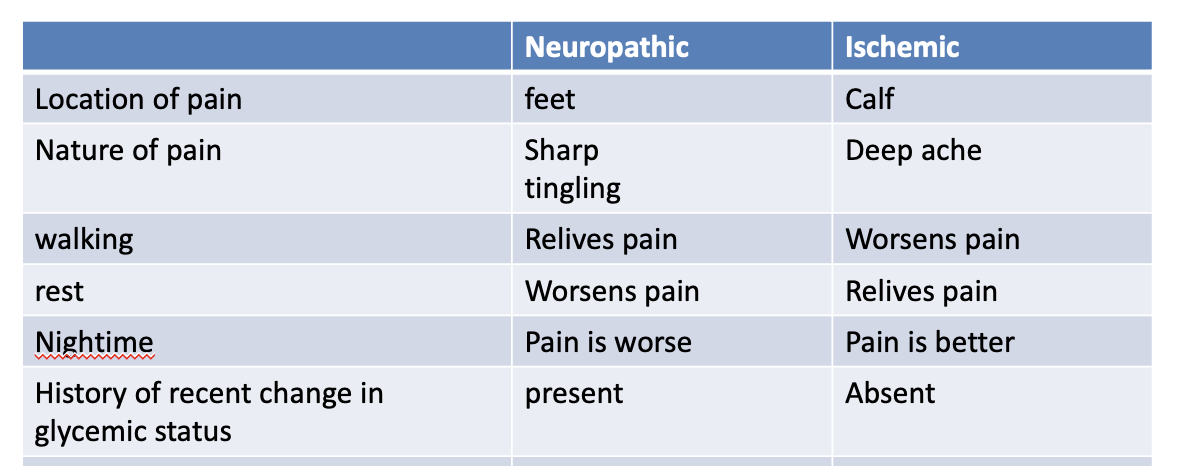
- Q. What are the points of difference between neuropathic pain from ischemic pain in diabetics?
- Q. Does the painful neuropathy spontaneously resolve?
- In 55% of cases the pain resolves in 12 months
- This is especially true if there is a recent change in glycemic status and there is a history of painful acute sensory neuropathy which is generally self-resolving
- #Pearl
- Nerve may discharge spontaneously when it is either being damaged or being repaired
- Q. Does the pain disappear always a good sign?
- Disappearance of pain can mean either there is improvement in the nerve function or deterioration
- It is not always a good thing
- **Pain control **
- Q. Enlist the drugs used in the management of Painful diabetic neuropathy.
- Antidepressants
- Amitriptyline
- Duloxetine
- Venlafaxine
- Desipramine
- Anticonvulsants
- Pregabalin
- Gabapentin
- Valproate
- Others
- Isorbidade dinitrate spray
- Capsaicin cream
- Alpha lipoic acid
- TENS- transcutaneous electric nerve stimulation
- Antidepressants
- Q. Which are the three first-line agents in painful diabetic neuropathy?
- SNRI- duloxetine, and venlafaxine
- TCA- Amitryptiline , nortyptiline and desipramine
- Gabapentinoid antiseizure medications - pregabalin , gabapentin
- Q. Of the above which is the best medication?
- No medication is better than other
- Hence the choice should depend on comorbidities, side effect profile, and patient preferences
- **Antidepressants **
- Q. Are antidepressants effective?
- Yes
- They have been proven in clinical trials
- Effect is generally seen in 6 weeks and the dose required is less than the dose typically used in depression
- Q. What are the common side effects of amitriptyline and duloxetine?
- Amitriptyline – Dry mouth
- Duloxetine – constipation
- Q. What is the typical dose of amitriptyline used?
- Starting dose of 10-25 mg
- Can give up to 100 mg/day
- Given at bedtime
- Q. In which patients do you need to be careful while prescribing TCA?
- Patient with a history of heart disease
- Q. Which is the least cardiotoxic TCA?
- Doxepin
- Q. Which TCA has fewer anticholinergic side effects?
- Nortriptyline
- #Pearl
- Also be careful of using amitryptiline in elderly males – as they can have urinary retention if they have a prostate problem. In patients with prostate issue, Amitryptiline can be replaced by nortriptyline
- Q. What is the action of Duloxetine?
- It is a combination of SNRI and SSRI
- Q. What is the important side effect of duloxetine in diabetics?
- It can cause a mild increase in blood glucose
- Q. What is the typical dose of Duloextine used?
- Typically used in a dose of 60 mg
- Starting dose of 20-30 mg - escalate up to 120 mg
- Must be taken on a full stomach
- Q. Why is the drug not given on empty stomach?
- It can cause nausea as an important side effect
- Q. Can it be combined with other SNRI?
- No
- But it can be combined with pregabalin
- Q. In which related condition, it must be avoided?
- Avoid patients having restless leg syndrome since it can exacerbate the problem in such patients
- **Anticonvulsants **
- Q. What is the mechanism of action of Pregabalin?
- Inhibits presynaptic release of excitatory neurotransmitters
- Q. What is a common but important side effect of Pregabalin?
- Weight gain
- Typically about 7% of weight gain is seen
- Does not impact diabetes control
- Q. How do you dose pregabalin ?
- Typical starting dose is 75-150 mg/day
- Generally given in 2-3 divided doses
- Most trials use a starting dose of 150 mg/day
- Every 3-7 days, 75 mg dose can be increased to upto 300 mg/day
- For other indications up to 600 mg/day is given, but for neuropathy 300 mg/day is generally sufficient
- Q. Is it a habit-forming drug?
- Yes
- Q. Is gabapentin useful in painful diabetic neuropathy?
- Yes. However, some trials have shown mixed results
- Trials have shown it is not effective as placebo
- It is typically given in a dose of 300-600mg TID
- Q. Which other anticonvulsants can be used?
- Valproate and carbamazepine are effective but generally not used because of better drugs are available
- **Other drugs **
- Q. What is the mechanism of action of Capsascian cream?
- It causes local depletion of substance P
- Q. How and when is it used?
- It is available as 0.075% cream
- It is applied topically 4 times a day
- Generally used if anticonvulsants and antiepileptics don’t work
- Q. What is the logic of using alpha lipoic acid (ALA) in DN?
- ALA is an antioxidant
- We know the role of reactive oxygen species in the etiology of DN
- Q. Which are the important trials with ALA?
- SYDNEY 1 trial- IV ALA
- SYDNEY 2 trial- use oral ALA
- These trials have shown ALA to be effective
- Q. What is the dose of oral ALA to be used?
- Oral ALA in a dose of 600 mg OD can be used in cases refractory to other medications
- Q. Which opioids have been used?
- Tramadol
- Oxycodone
- Dextromethorphan
- However, they are best avoided as they can cause addiction
- Q. Are combination treatments more effective than a single drug?
- Yes
- Q. Is transcutaneous electric nerve stimulation useful?
- Yes
- TENS is useful for diabetic neuropathy
- Q. What about acetyl L carnitine?
- Some trials have shown it to be effective in a dose of 1000 mg
- Q. Which spray is effective?
- Isorbidade dinitrate spray
- Small trials have shown it to be effective
- Q. What is the role of NSAIDs?
- NSAIDs are effective in reducing pain in diabetic neuropathy
- However, it can worsen nerve injury hence it is better avoided than other meds
- Q. Which procedure is used in refractory DN?
- Spinal cord stimulation
- It is an invasive procedure
- Electrodes were introduced to give nerve stimulation to a dorsal column of the spinal cord
- Q. Which drug according to the American academy of neurology is most effective?
- Pregabalin – in dose of 300-600 mg/day
- Q. What is the ADA approach?
- 1st- Rule out non-diabetic etiology
- 2nd - Stabilize blood glucose
- 3rd- Tricyclic antidepressants / anticonvulsants
- 4th- Opioid and other agents
- **Non-glycemic measures **
- Q. What is the role of surgical decompression?
- It is known as Dellon’s procedure
- It is the decompression of peripheral nerves as a treatment of painful diabetic neuropathy
- However it is controversial and not recommended
- Q. Which anti-diabetic drug used in diabetes produces B12 deficiency?
- Metformin
- Q. What B12 level is optimal in diabetic patients?
- Generally -250 pg/ml
- In diabetics – 460 pg/ml is the optimal B12 level
- Q. Which B12 preparation is better for diabetics?
- Methylcobalamin Is better for diabetics, not cyanocobalamin
- It is given in a dose of 3000 ug/day which achieves a B12 level of 1000 pg/ml
- Q. Which 2 conditions are often associated with painful Diabetic neuropathy ?
- Mood disorder
- Sleep disorder
- Hence the treatment should address these issues as well
- Q. Apart from tramadol which is the other centrally acting opioid?
- Tapentadol
- It is available in India as TYDOL

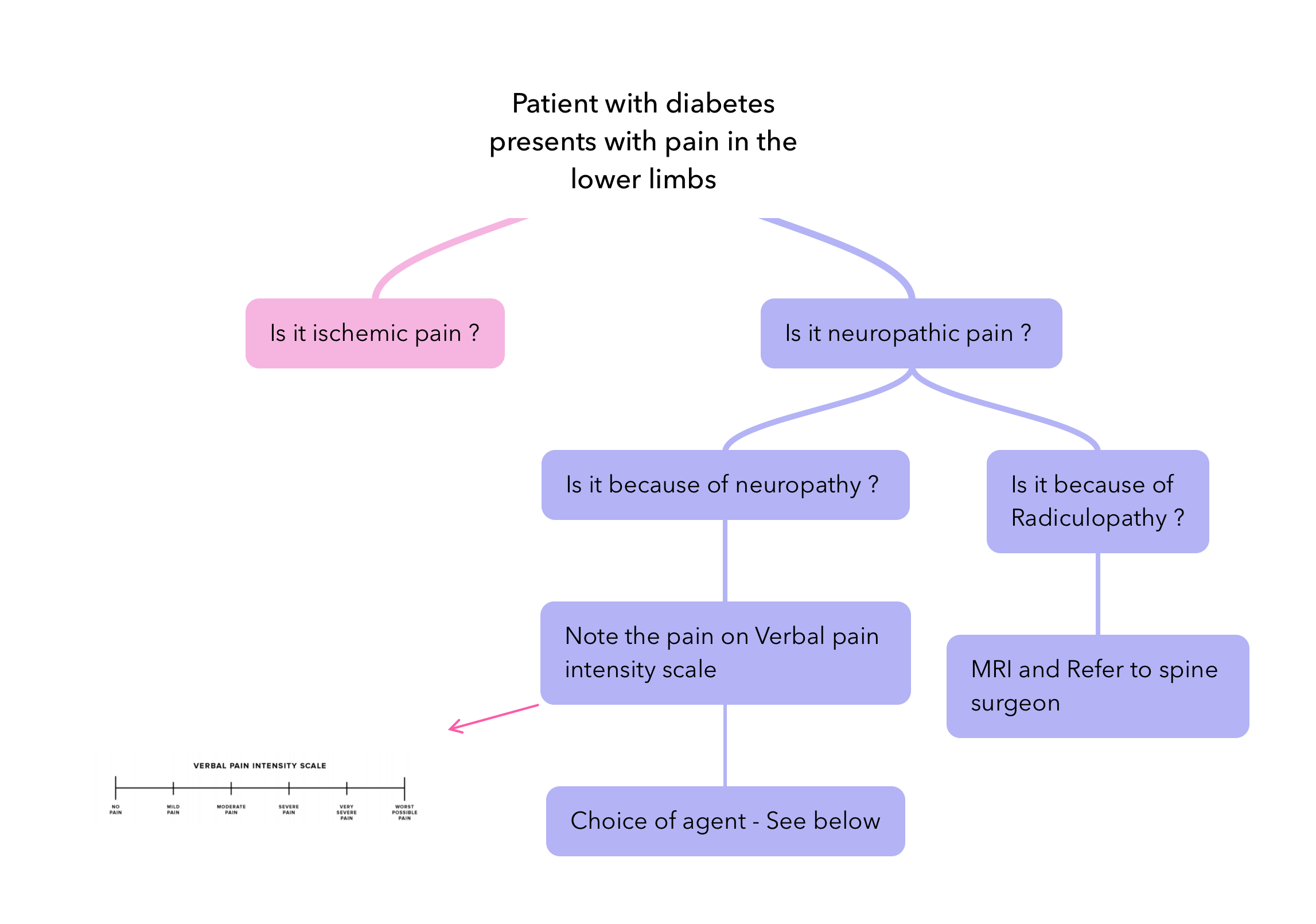
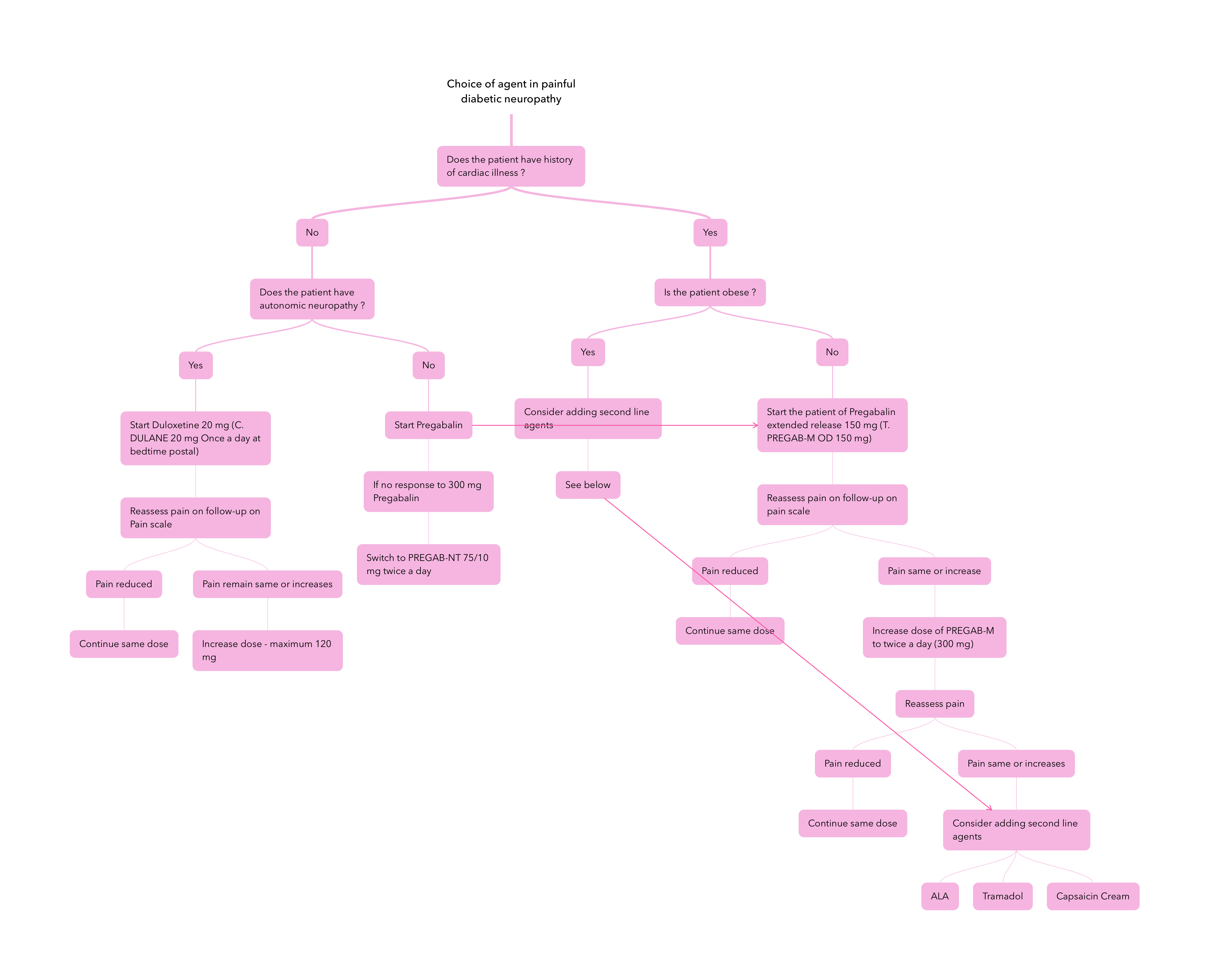
- Q. Give a practical strategy for the management of painful diabetic neuropathy in India.