- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
Connected notes
-
Q. Why is insulin requirement in CKD unpredictable?
- Insulin resistance increases in CKD
- Insulin degradation reduces in advanced CKD
- Both of these typically reverse on dialysis
-
Q. What are the other challenges of managing diabetes in CKD patients?
- HbA1c may be unreliable because of uremia
- Dextrose in the peritoneal fluid can interfere with diabetes management
- Metabolism of oral drugs is disturbed in CKD patients
- Changes in dietary intake and exercise is typical in CKD
-
**Monitoring glycemic control **
-
Q. Which method of HbA1c measurement is unreliable in a patient with CKD?
- Agar gel electrophoresis is unreliable in a patient with CKD
-
Q. What produces interference in HbA1c in CKD?
- Production of carbamylated hemoglobin due to urea causes false high measurement of HbA1c
-
Q. Which method of HbA1c measurement can be used without interference in a patient with CKD?
- Boronate – agorase affinity chromatography method
- Thiobarbituric acid method
- These can be used without interference
-
Q. Which other factors cause a falsely high value of HbA1c in CKD?
- Iron deficiency anemia
-
Q. Which factors cause false low values in CKD?
- Reduced RBC lifespan and hemolysis
- Recent RBC transfusion
- Use of EPO
-
Q. Should HbA1c still be used?
- It can be used
- We must know the background details of the patient (like described previously) for interpretation
-
Q. What are the options other than HbA1c?
- Glycated albumin is another option
- It measured HbA1c over a period of 7-14 days
- However, how it is affected in CKD – there is no evidence that it is better than HbA1c
-
Q. What is the problem with the use of glucometer inpatients on peritoneal dialysis?
- Glucometer, which uses the glucose dehydrogenase (GDH-PQQ) method, have interference with icodextrin in the peritoneal dialysis fluid
- The effect of icodextrin can last over two weeks after stopping PD
- However, newer strips do not use this method, and newer PD fluids do not have icodextrin
-
**Goals of therapy **
-
Q. What is the HbA1c target for patients with CKD not on dialysis?
- The target remains the same at 7% as for non-CKD patients
- However, patients who are at high risk of hypoglycemia or limited life expectancy may have more liberal targets
-
Q. What is the target in CKD patients on dialysis?
- Young patients <50 years without comorbidities- close to 7%
- Older patients and/or having comorbidities and high risk of hypoglycemia- close to 8%
-
Q. Why is the risk of hypoglycemia more in dialysis patients?
- Change of insulin resistance with dialysis
- Change in an eating pattern during dialysis
-
Treatment of non-dialysis CKD patients
-
Q. Which secretagogues are safe in nondialysis CKD patients?
- Glipizide- short acting SU- 2.5-10 mg/day or
- Repaglinide
-
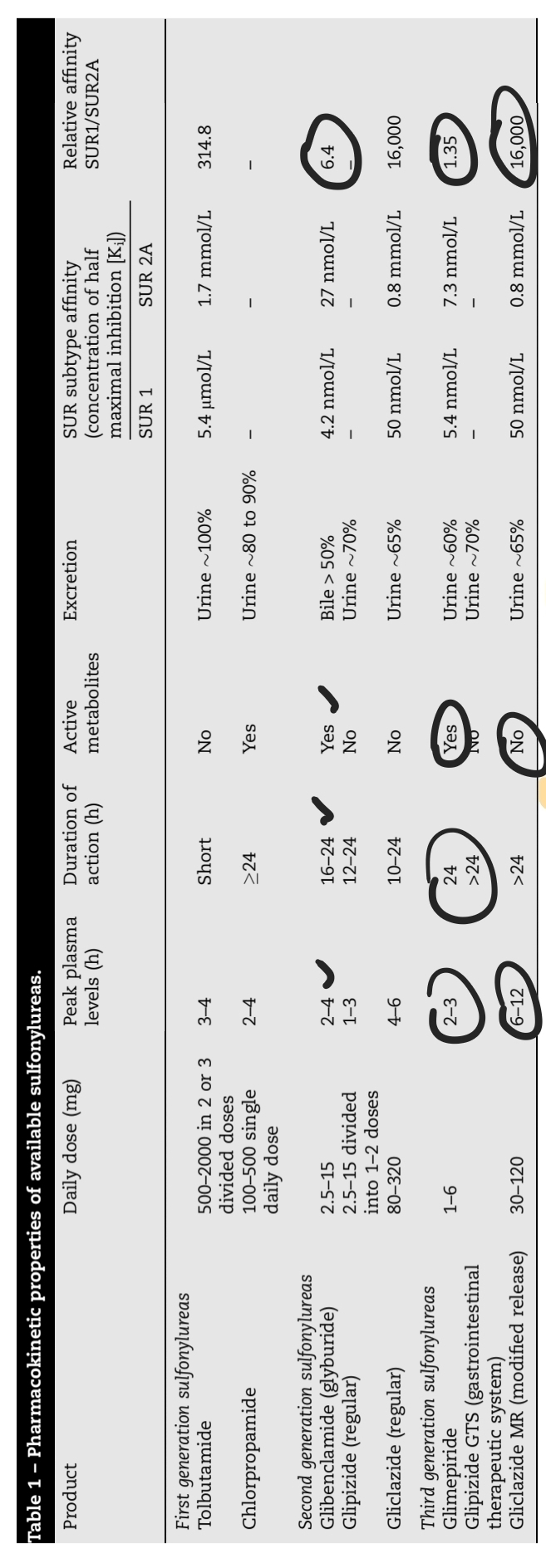
Q. Can you tell me something about using Sulphonylurea in patients with CKD ?
- SU with active metabolites like glibenclamide and Glimepiride can cause Hypoglycemia in patients with renal impairment
- Avoid glibenclamide in those with GFR <60
- Glimepiride - needs dose reduction for those with GFR <30
- For glipizde and Gliclazide - can be used safely without dose modification for GFR of 30-60
- For GFR <30- can it still use it with careful monitoring
-
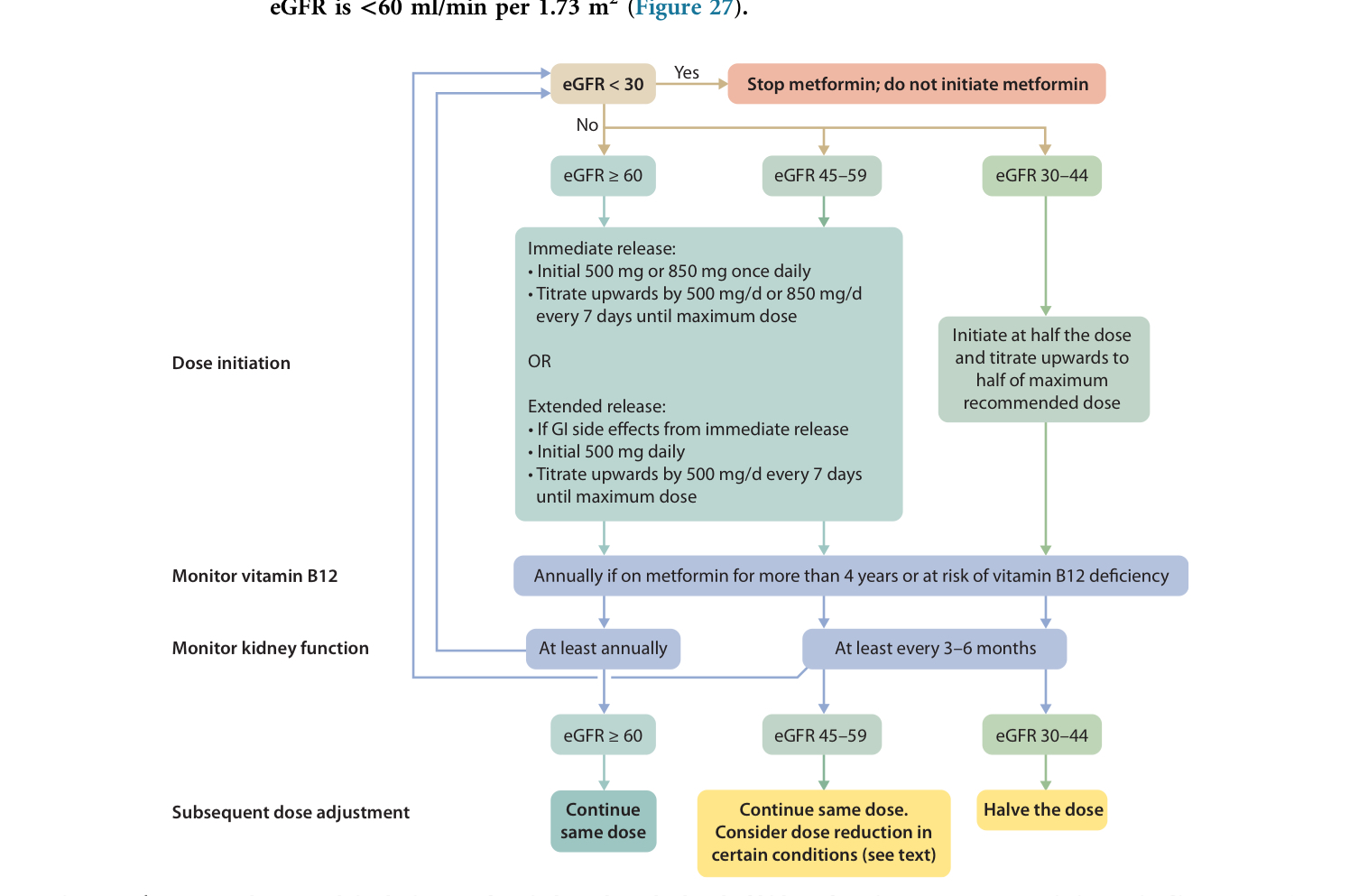
Q. What is the current guideline on metformin use and GFR?
-
GFR >45 can be used
-
GFR 30-45- Maximum Metformin use of 1000 mg /day
-
GFR < 30 – Avoid metformin
-
Also, avoid in patients with GFR <60 with a high risk of lactic acidosis like
- Hypotension
- Shock
- Hypoxia
- Radiocontrast use
- Sepsis
-
-
-
Q. Can DPP IV be used in CKD patients?
- Yes
- Saxagliptin and sitagliptin require dose adjustment
- Linagliptin does not require dose adjustment
-
Q. What is the dose of Sitagliptin in patients with renal failure?
- eGFR- 30-50 - 50 mg
- <30 - 25 mg
-
Q. What is the dose adjustment required for saxagliptin in renal failure?
- GFR < 50 – 2.5 mg of Saxagliptin
-
Q. What is the adjustment of insulin dose recommended in patients with CKD?
- GFR >50 – no dose requirement
- GFR 10-50- 25% reduction in dose
- GFR <10 % - 50% reduction in dose of insulin
-
**Treatment of diabetes in CKD patients on dialysis **
-
Q. What is the preferred therapy in CKD patients on dialysis?
- CKD patients on dialysis must be treated with Insulin
- This is as per 2005 K/DOQI guidelines
-
Q. What is the dose typically used in dialysis patients?
- Typical starting dose is 50% of the usual starting dose
-
Q. What is an approach to patients on PD?
- If a patient is already well controlled before starting PD- continue what he/she was taking
- If it was not well controlled or newly diagnosed diabetes- start with OAD- may move to insulin if required
-
Q. What are the advantages of Glipizide and repaglanide?
- Mainly have hepatic metabolism
- Only inactive metabolites are excreted through the kidney
- They have a short half-life
- Hence the risk of hypoglycemia is less
-
Q. Can metformin be used in Dialysis (HD/PD) patients?
- No
-
Q. Can insulin be given intraperitoneally?
- Yes
- But subcutaneous is preferred
- Intraperitoneal insulin is too complex for a patient to adjust
- Also, there is a risk of bacterial contamination of dialysis fluid while injecting insulin
- Finally, absorption is erratic in patients on intraperitoneal insulin
-
Q. Is there any study comparing SC vs. IP insulin?
- Yes
- One study has shown better results with IP insulin
- However, the dose use for IP insulin was almost double of SC insulin
-
Q. Which are carbohydrate-free peritoneal fluid preparations?
- They use
- Glucose polymer like icodextrin
- Or amino acid dialysate solution
-
More on Oral agents in CKD
-
Q. Are SU cleared by hemodialysis?
- SU are firmly bound to albumin and hence are not cleared by the HD process
-
Q. Glimiperide has liver metabolism or renal metabolism?
- It is metabolized in the liver
- However, it produces active metabolites, which is excreted through the kidney
-
Q. Is half-life of repaglinide same as that in non CKD?
- Some small amount of weak active metabolite is produced in repaglinide also
- Hence its half-life is a little prolonged in CKD
- Hence start with the lower dose of 0.5 mg and then up titrated
-
Q. What about Nateglinide?
- It is not recommended in CKD
- It has renal excretion
-
Q. Which gliptin is cleared by dialysis?
- Saxagliptin is cleared by dialysis
- Hence must be given after dialysis
-
Q. Why are TZD avoided in CKD patients?
- They cause edema and increase the risk of heart failure
-
Q. Are alpha-glucosidase inhibitors recommended in CKD?
- No
- They have active metabolites absorbed, which have renal excretion
-
Q. Why do CKD patients have minimal symptoms despite marked hyperglycemia?
- This is because they are oliguric/anuric
- Hence there is no hypovolaemia which is typically seen when the blood glucose levels are very high
-
Q. What is the typical electrolyte imbalance seen in CKD patients with severe hyperglycemia?
- Maked extracellular hypertonicity shift of potassium to outside the cell → hyperkalemia
- Shift of fluid inside the cell → hyponatremia
-
Q. What is the approach to the management of DK / severe hyperglycemia in CKD patients?
- Here, fluid administration is not a priority, and priority is the administration of insulin
-
Q. What is “Burnt out diabetes”?
- Many patients with ESRD on dialysis have normalization of HBA1c to level <6%
- The reasons for this are not known
- But this is called Burnt out diabetes
- Many patients develop hypoglycemia on ongoing treatment because of this
-
Q. What are the possible reasons for this burnt-out diabetes?
- Increase half-life of endogenous insulin
- Reduced caloric intake due to uremic toxins
- Certain uremic toxins like guanidino compounds have biguanide like effects
-
Q. Can fructosamine be used for monitoring patients with CKD and diabetes?
- Yes
- It gives glycemic control over 1-2 weeks
- Reduced albumin or protein losses in PD may cause false lowering of its values
- Some studies have shown it is more effective than HbA1c for monitoring in these patients
-
Q. Give some guidance for the management of hyperglycemia in in-patients during hemodialysis?
- Patients have different insulin sensitivity both pre and post dialysis
- Reduce basal insulin by 25% on the day following dialysis compared today before the dialysis
-
Use of SGLT2i in CKD
PLEASE NOTE- new guidelines have been published on SGLT2i use in CKD in 2022 - please see our note Updates on Management of Diabetic kidney disease
-
Q. Which are two important pathogenic mechanisms causing kidney disease in patients with diabetes?
- Glomerular hypertrophy
- intraglomerular hypertension
-
Q. What produces glomerular hyperfiltration?
- It is mainly due to afferent arteriole vasodilatation
- SGLT2 is increased in people with diabetes because of hyperglycemia hence there is an increase in sodium reabsorption
- This causes afferent vasodilatation
- This further leads to Glomerular hyperfiltration
- Glomerular hyperfiltration produces intraglomerular hypertension which leads to diabetic kidney disease
- AGE, IGF1, sorbitol, ANP etc have similar role on afferent arterial vasodilatation.
-
Q. Summarize the mechanism of renal damage in Diabetic nephropathy and how SGLT2 and ACEI protect the kidney?
- Step 1- Tubuloglomerular feedback
- Reduced GFR → reduced flow rate in kidney → increase Na reabsorption → reduced Na reaching the Macula densa → macula densa signals release of renin → RAAS → angiotensin II → efferent vasoconstriction → increase of GFR
- Angiotensin II produces both afferent and efferent Vasocontriction but efferent > afferent – hence the net increase of GFR
- Vice versa occurs, if there is an increase in GFR

- Reduced GFR → reduced flow rate in kidney → increase Na reabsorption → reduced Na reaching the Macula densa → macula densa signals release of renin → RAAS → angiotensin II → efferent vasoconstriction → increase of GFR
- Step 2 – Hypefilteration in diabetics
- People with diabetes have Glomerular hyperfiltration
- This is because IGF1, AGE, sorbitol afferent vasodilatation increase GFR
- Hence intact Tubuloglomerular feedback is required for normalizing GFR
- Step 3 Role of glycosuria
- In Diabetes, there is an increase of glucose in urine hence SGLT2 is activated → to increase Sodium and glucose reabsorption → remember, more Na is reabsorbed →, so less Sodium to Macula densa → , so more Renin release !!
- Already, the GFR is high due to hyperfiltration, and this adds fuel to the fire
- So there is a loss of Tubuloglomerular feedback in diabetics
- Step 4 – Fuel to the fire
- Hypertension and loss of nephrons further increase pressure on the remaining nephron and increase GFR
- Hence producing Intraglomerular hypertension and glomerular hypertrophy
- Step 4 – Now for ACEI relief
- ACEI provides noticeable relief by blocking the RAAS pathway preventing the increase of GFR caused by the renin system
- Step 5- SGLT2i
- SGLT2i inhibits sodium and glucose reabsorption and hence keeps the tubuloglomerular feedback intact!
- Hence it is renoprotective
- Step 1- Tubuloglomerular feedback
-
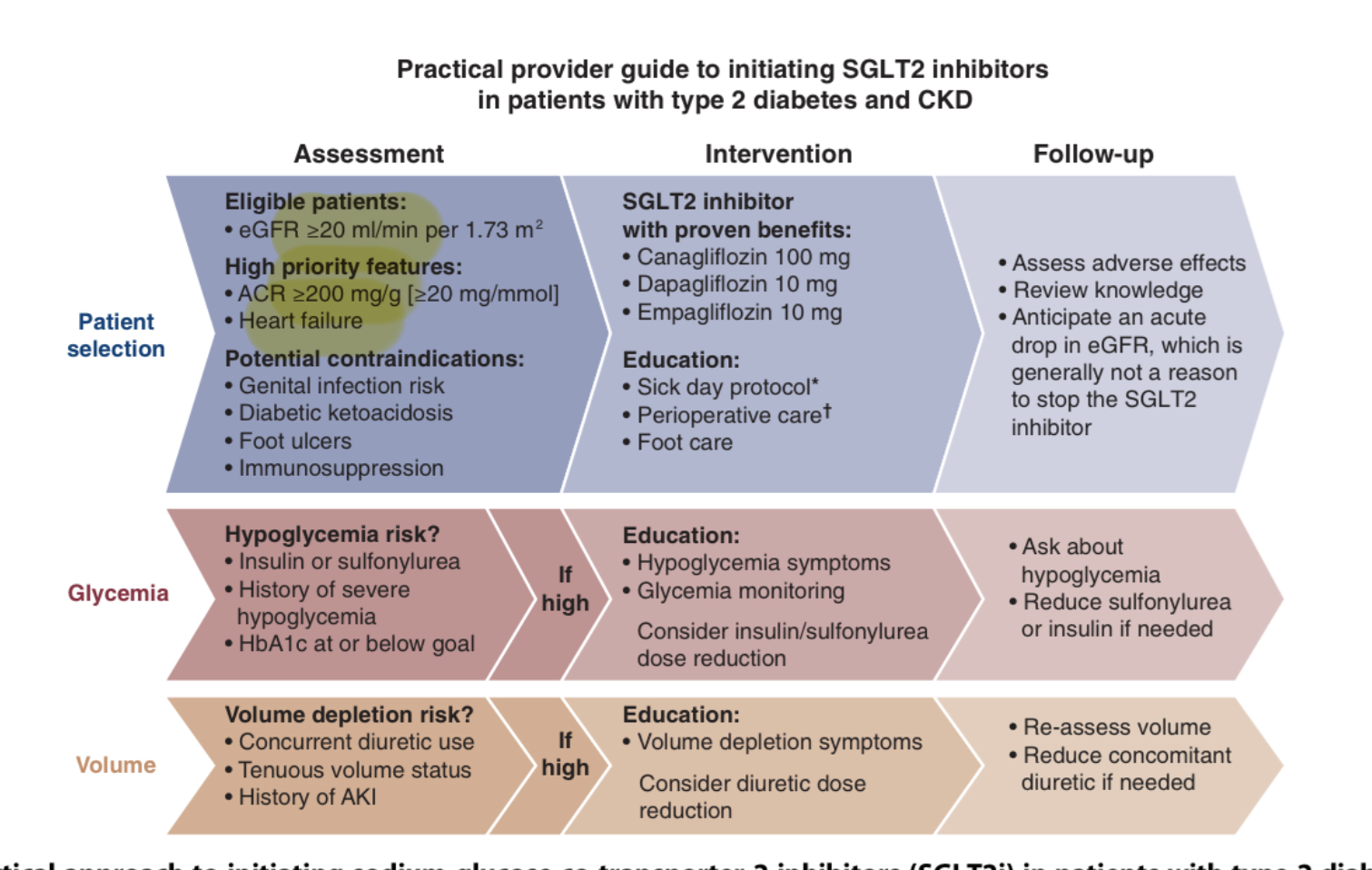
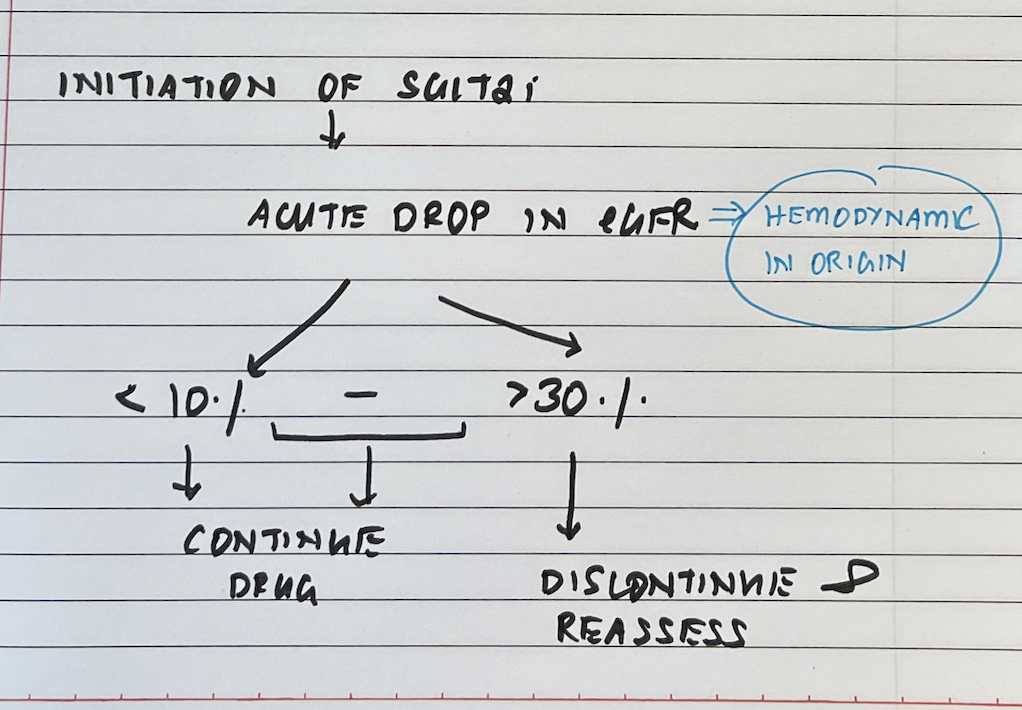
Q. Does the initiation of SGLT2i produce a reduction in patients with Diabetic kidney disease produce an acute decrease in eGFR?
- Yes
#update - 15-Dec-2022
- Q. As per the new guidelines up to what eGFR category can the SGLT2i be used?
- SGLT2i can be used initiated up to eGFR >20
- However, the drug can be continued in patients with type 2 diabetes, if the eGFR falls below this level
- The only consideration for stopping this drug is when the patient requires dialysis
- Q. Which patients with diabetic kidney disease should not be given SGLT2i?
- There is not enough data for:
-
- Type 1 diabetes
-
- Post-renal transplant
-
- Patients on dialysis
-
- eGFR <20- at this eGFR SGLT2i should NOT be initiated, but if the patient is already on the drug and eGFR falls to this level it can be continued till the patient is started on dialysis
- Q. Summarize some practical recommendations for initiating SGLT2i in Diabetic kidney disease.
- Q. Where does GLP-1 receptor agonist stand in the equation?
- It is considered the preferred second-line therapy in patients with Diabetic kidney disease for diabetes control, CV risk reduction, and weight loss
- However, since it does not have a dedicated CKD trial, it misses out on Level A evidence