-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Update credits
-
Q. Which organisms produced mucormycosis?
- Fungi from the Mucorales order produce mucormycosis in human beings
- They include:
- Rhizopus
- Mucor
- Rhizomucor
- Cunninghamella
- Saksenaea
- Apophysomyces
-
Q. What is the most devastating syndrome associated with mucormycosis and diabetes?
- Rhino-orbital-cerebral mucormycosis
- Pulmonary mucormycosis
-
Q. What produces Rhino-orbital-cerebral mucormycosis (ROCM)?
- Inhalation of spores of these fungi in susceptible patients produces this syndrome of ROCM
-
Q. Which are the other organs that can be potentially involved?
- Skin
- GI tract
- Renal
- Disseminated disease
-
Q. Where are the Mucorales organisms found in nature?
- They are ubiquitous
- They are often found in decaying vegetation and the soil
-
Q. Do people with an intact immune system develop mucormycosis?
- No
- Only people with compromised immunity develop mucormycosis
-
Q. What are the differences in hyphae of mucormycosis versus hyphae of aspergillus?
-
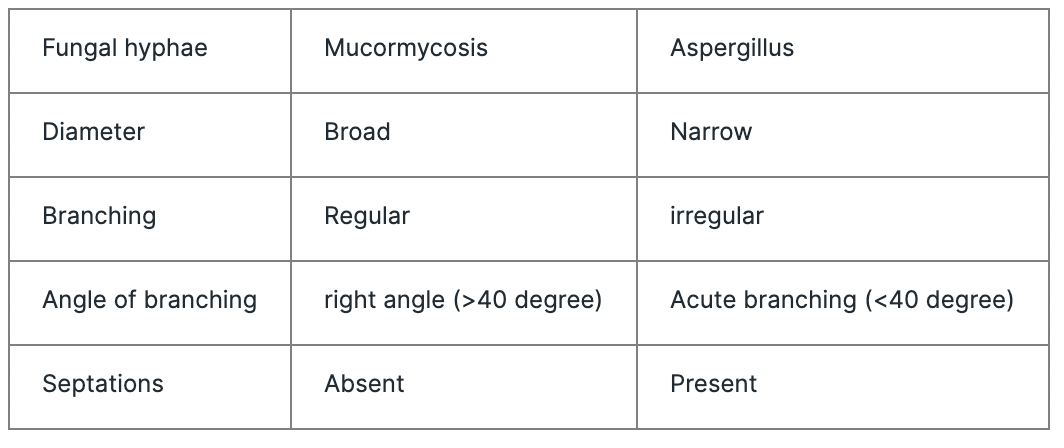
-

-

- Lactophenol cotton blue (LCB) mount from the growth revealed aseptate hyphae with nodal rhizoids and short sporangiophores with terminal spherical sporangia filled with brownish sporangiospores, suggestive of Rhizopus microsporus
-
-
Q. The lack of septations has a clinical consequence in mucormycosis. What is the clinical consequence of the same?
- The lack of septations makes the fungus fragile and hence the fungus finds it difficult to grow unless they have a very conducive environment
- It is also difficult to culture the same in the lab
- Specimens containing suspected mucormycosis must be finely minced to prevent damaging the hyphae
-
Q. Which chelating agent is known to increase the risk of mucormycosis?
- Deferoxamine
-
Q. Why does Deferoxamine increase the risk of mucormycosis?
- The deferoxamine and iron bind together to form feroxamine
- This is a siderophore for the species Rhizopus allowing increasing iron uptake by the organism and hence increasing their growth and tissue invasion
-
Q. Do other chelating agents like deferasirox also increase the risk of mucormycosis?
- No
- They do not form siderophores and hence do not increase the risk of mucormycosis
- They may be protective
- However, adequate studies for any benefit of the same in humans are missing
-
Q. What is a siderophore?
- Siderophore are organic compounds that help transport iron inside the cell of an organism
-
Q. Why do we see necrosis and infarction in patients having mucormycosis?
- This is because the fungal hyphae are angioinvasive
- The invasion of the vasculature of the host leads to necrosis and infarction
-
Q. Why does Mucormycosis thrive in a ketogenic environment?
- The Rhizopus species has an enzyme called KETONE REDUCTASE
- This helps to breakdown the ketone as fuel for these fungi
-
Q. Is there any additional pathology in diabetic ketoacidosis which helps the fungi grow?
- Presence of free iron is high in Diabetic ketoacidosis
- Again, this becomes a vehicle for the fungi to grow
-
Q. Broadly what are the risk factor for Mucormycosis?
- Diabetes mellitus with Ketoacidosis
- Use of Deferoxamine
- Increased iron stores
- Treatment with glucocorticoids
- COVID-19 infection with diabetes and glucocorticoid use
- Post-transplant
- AIDS
- Injection drug use
- Burns
- Malnutrition
- Hematological malignancies
-
Q. Do all patients with Mucormycosis have pre-existing diabetes?
- No
- Only 30-40% of patients have pre-existing diabetes
- Some of the others are diagnosed to have new onset of diabetes
- In the era of COVID-19, the development of Mucormycosis has been rampant, especially in patients having steroid-induced diabetes
-
Q. Is mucormycosis diabetes defining illness?
- Yes
-
Q. What type of mucormycosis infection is common with diabetes?
- Rhino-oculo-cerebral mucormycosis is common with diabetes
-
Q. Why has the incidence of mucormycosis in diabetes reduced in many countries?
- The incidence of mucormycosis in diabetes has reduced considerably
- One theory is that this is because of the widespread use of statins in diabetes
- Statins have an inhibitory effect on the growth of these fungi
- *"Exposure of R. oryzae to statins at concentrations below their MICs decreased virulence both in vitro and in vivo. Further investigation is warranted into the use of statins as adjunctive therapy in mucormycosis" *
-
Q. Apart from diabetes, what is the second most common underlying risk factor?
- Hematologic malignancies
-
Q. What are the common sources of Mucor in hospital settings?
- Hospital linen
- Nearby construction sites
- Tongue depressors
- Adhesive tapes
-
Q. Is Mucormycosis known to occur with IV cannula?
- Yes
- This has been often reported
-
Clinical Presentation
-
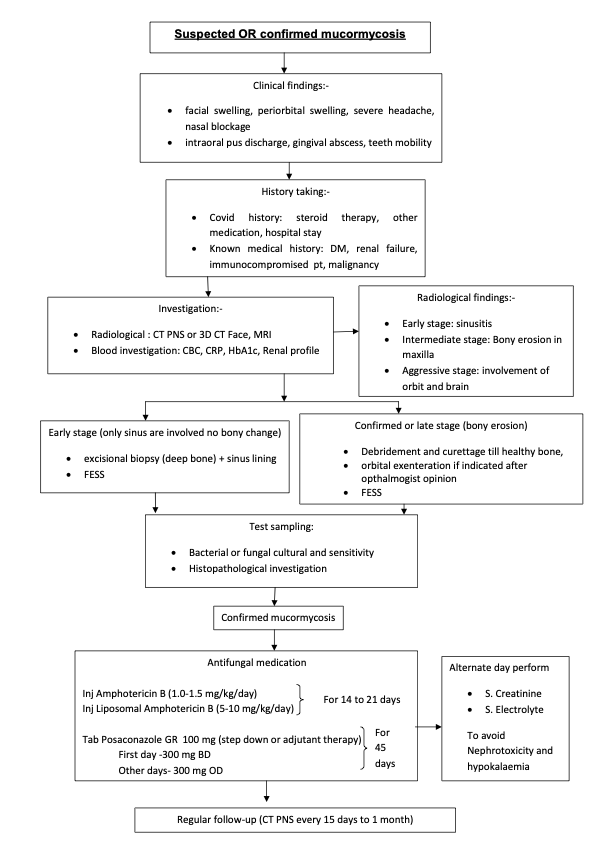
Q. What are the early clinical features of Rhino-cerebral mucormycosis?
- Clinical features resemble sinusitis
- Nasal discharge- often blackish
- Nasal congestion
- Headache
- Sinus pain
- Clinical features resemble sinusitis
-
Q. What is the typical clinical tell-tale sign for Rhino-cerebral mucormycosis?
- These patients have a characteristic 'black eschar' in the nasal mucosa
- They can have associated black purulent discharge from the nose
- These patients have a characteristic 'black eschar' in the nasal mucosa
-
Q. What are the features of eye involvement?
- Periorbital edema
- Proptosis
- Blindness
-

- Patient having Mucormycosis post-COVID19
- Patient was having diabetes mellitus with glucocorticoid use
-
Q. What is another frequent facial sign seen in these patients?
- These patients complain of numbness of the face
- This is because of the involvement of the branches of the fifth cranial nerve
-
Q. Which species amongst the mucor group produces the Rhino-cerebral mucormycosis?
- Rhizopus oryzae
-
Q. Where can this mucormycosis spread centrally?
- They can spread to the frontal lobe and Sphenoid and Cavernous sinus
-
Q. Is the hematogenous spread of mucormycosis known to occur?
- It is rare
- It is only seen in patients with hematological malignancy having neutropenia
-
- Rhino-cerebral mucormycosis is mainly seen in patients with diabetes mellitus
-
Q. What is the common sources of infection in cutaneous mucormycosis?
- Intravenous catheter / IV cannula are common hospital-acquired sources
-
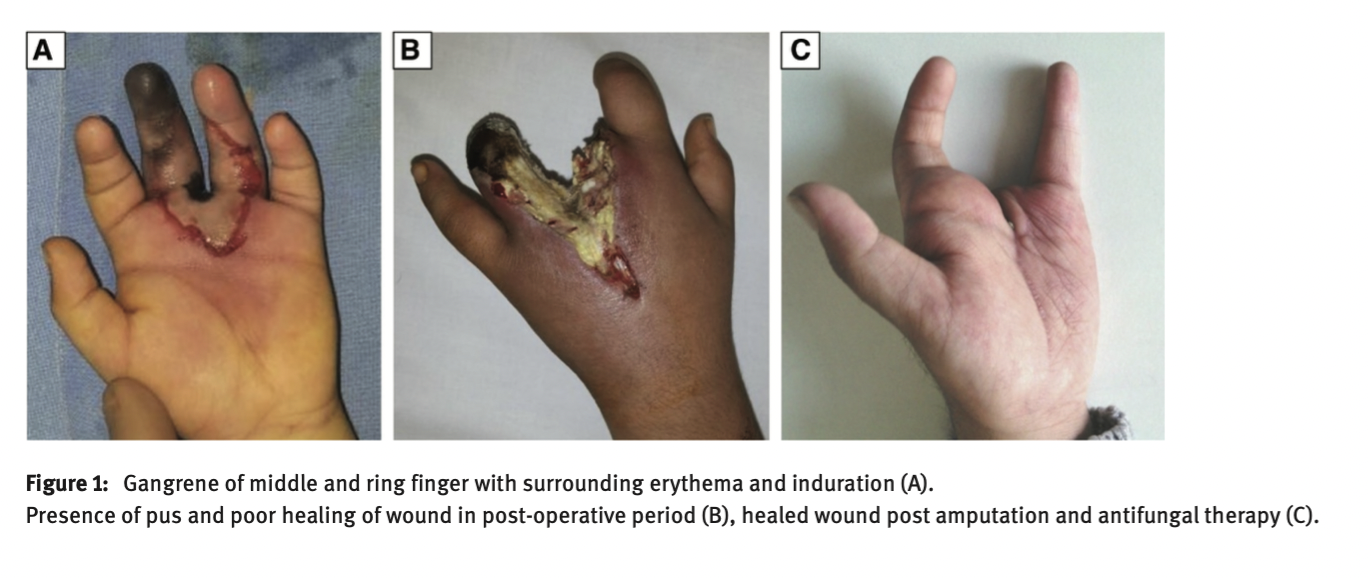
-
Diagnosis
-
Q. If a fungus from this group is isolated in a specimen, does it prove that the patient has mucormycosis?
- It is important to note that the fungi from this family are common contaminants in cultures and isolation of the fungi does not necessarily prove that the patient is having mucormycosis unless the patient has clinical signs and symptoms of the disease
- Interpreting in the right context of the disease is important in this scenario
-
Q. Apart from culture, which other technique is using for identifying the fungi?
- PCR is useful and promising
-
Q. Which imaging technique is more useful in such patients, CT scan or MRI?
- CT scan is useful for bony erosions
- However, MRI is more useful to detect intracranial involvement

-
Management
-
Q. Broadly, what is the management of Mucormycosis?
- Three things are essential
- Surgical Debridement of the involved area
- Antifungal therapy
- Good glycemic control
- Three things are essential
-
Q. What is the antifungal treatment of choice for such patients?
- These patients should be treated with Liposomal Amphotericin B given in the dose of 5-10 mg/kg/day for several weeks followed by Oral Posaconazole
- These are continued till all signs of infection are resolved
-
Q. Which other antifungal is an alternative to Posaconazole as step-down therapy?
- Isavuconazole
-
Q. What is the important point while giving posaconazole to the patient?
- Posaconazole must be given WITH FOOD (mainly fatty food) to enhance its absorption
- Delayed-release tablets may be used if available
-
Q. Is delayed-release preparation of Posaconazole available in India?
- Yes
- It is available as Picasa-GR Tablet from Intas pharma in a dose of 100 mg tablets
- It is expensive with a single tablet costing Rs. 400
-
Q. What is the dose of Posaconazole?
- Loading dose of 300 mg / 12 hourly on the first day followed by 300 mg every 24 hours daily
-
Q. Is Posaconazole available in Injectable form?
- Yes
- Posatral 300mg Injection
-
Q. What is the challenge with the IV preparation?
- It should be avoided in patients with renal impairment
- It has a vehicle called SBECD which is toxic and can potentially accumulate in such a scenario
-
Q. Can posaconazole suspension be used ?
- No
- It is not highly bioavailable and absorption is not assured
- It is available in India and it is very expensive
- It is available as Picasa 40mg Oral Suspension
-
Q. What is the advantage of liposomal AmpB compared to conventional?
- Liposomal AmpB is less nephrotoxic and hence larger doses can be given without nephrotoxicity
-
Q. How long is the therapy continued?
- Till all of the following conditions are met:
- Absence of all clinical signs of infection
- Resolution of all radiographic signs of active disease
- Reversal of underlying immunosuppression is achieved
- Therapy can extend for several months in most patients
- Till all of the following conditions are met:
-
Q. Amongst the various mucormycosis which species has the worst prognosis?
- The Cunninghamella species has the worst prognosis
-
Q. What is the mortality with Rhinocerebral mucormycosis?
- Poor prognosis
- Mortality is 25-60%
-
Amphotericin B (AmpB)
-
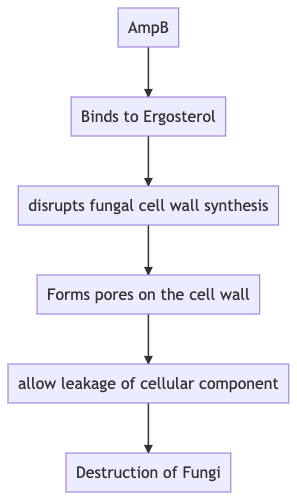
Q. What is the mechanism of action of AmpB against fungi?
-
Q. AmpB is Fungostatic or Fungicidal ?
- It is fungicidal
-
Q. Which fungi are sensitive to AmpB?
- Mucorales
- Candida
- Aspergillus
-
Q. Which fungi are resistant to AmpB?
- chromoblastomycosis
- Aspergillus terreus
- Candida lusitaniae
- Scedosporium spp
- Some Fusarium spp
-
Q. Resistance is emerging against which common fungi?
- Candida auris
-
Q. Which are the two major preparations of AmpB?
- AMPHOTERICIN B DEOXYCHOLATE
- LIPOSOMAL AMPHOTERICIN B
-
Q. In what forms is AmpB available?
- It is effective mainly in IV injectable form
- Oral suspension and inhaled are available in some countries but have limited use
-
Q. How and where does AmpB bind?
- It binds extensively to proteins-mainly lipoproteins
-
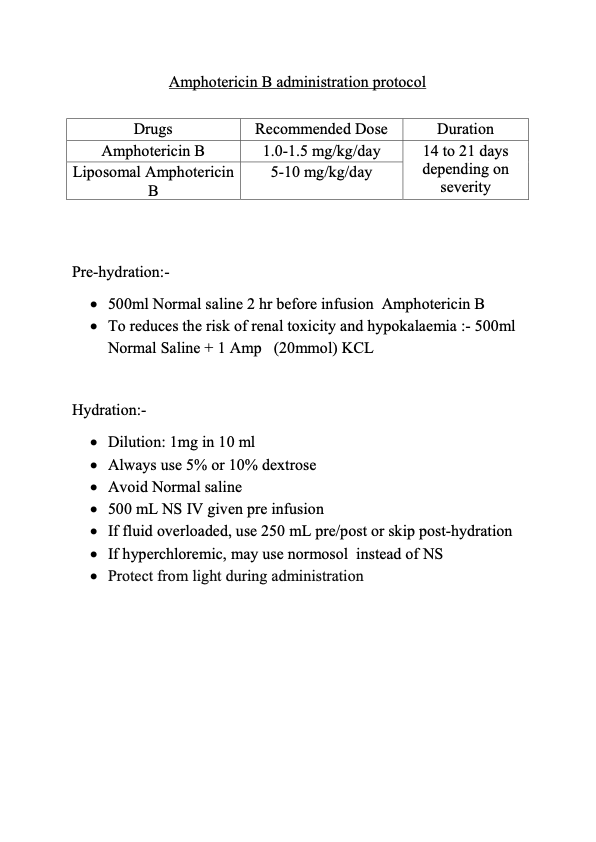
Q. What is the dosing in usual fungal infection and in Mucormycosis?
- AMPHOTERICIN B DEOXYCHOLATE - 1-1.5 mg/kg/day
- LIPOSOMAL AMPHOTERICIN B - 5-10 mg/kg/day
-
Q. Is a test dose required before giving AmpB?
- Yes.
- A test dose of 1 mg is administered before giving the final dose
- it is known to produce hypersensitivity reactions
-
Q. How is the IV dose of AMPHOTERICIN B DEOXYCHOLATE administered?
- It is given in 5% Dextrose - after the test dose
- The infusion is given for 4-6 hours
-
Q. Can it be given over a 24-hour infusion?
- 24-hour infusion will produce less nephrotoxicity
- However, the efficacy of the same in fungal infections has not been established
-
Q. Which is the immediate adverse reaction that occurs after the infusion of the injection?
- Nausea and vomiting are common after the infusion
- Chills and rigors can also occur
- This can be reduced by prophylactic NSAID (Ibuprofen is particularly useful in this setting)
-
Q. Is Thrombophlebitis common ?
- Yes
- Phlebitis can commonly occur in smaller veins
-
Q. How to avoid Thrombophlebitis?
- Use central vein
- Keep concentration of the in <0.1 mg/ml
- Avoid infusion time <4 hours
- Use different infusion sites
- Giving hydrocortisone (25 mg) or heparin 500-1000 IU/l to the infusion site
-
Q. Is the nephrotoxicity due to AMPHOTERICIN B DEOXYCHOLATE reversible?
- Yes
- It is potentially reversible
- There is a transient increase in creatinine in almost all patients
- Severe renal dysfunction due to the drug alone is rarely reported
- Basically, volume contraction is the likely culprit- which if corrected can be useful
-
Q. What can be done to prevent nephrotoxicity?
-
- Prefer liposomal preparation
- It is advisable to switch to liposomal preparation if Creatinine is >2.5 mg/dl
-
- Avoid volume contraction
- Potentially 250 mg of Normal saline before and after the infusion may be useful
-
-
Q. What are the common electrolyte imbalances following the infusion?
- Hypomagnesemia
- Hypokalemia
- Hyperchloremic metabolic acidosis
- This is all due to an increase in distal tubular membrane permeability
-
Q. What are the adverse hematological effects?
- AmpB can produce mild normochromic, Normocytic anemia
- This is transient
- Some patients may develop leukopenia
- AmpB can produce mild normochromic, Normocytic anemia
-
Q. How is the monitoring done of patients on AMPHOTERICIN B DEOXYCHOLATE?
- Daily S. Creatinine for 2 weeks- then weekly
- Twice weekly electrolyte- Pottasium and Magnesium
- Weekly CBC
-
LIPOSOMAL AMPHOTERICIN B
-
Q. What is the biggest advantage of using Liposomal AmpB?
- It reduces nephrotoxicity
-
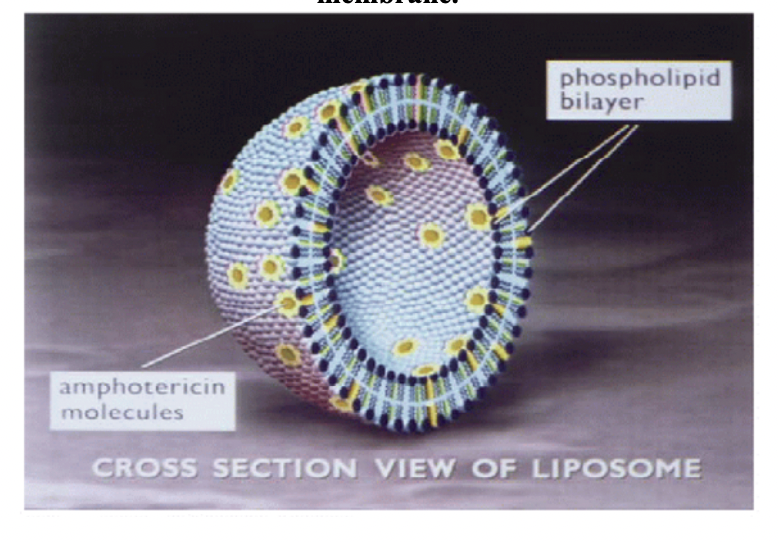
Q. What is the pharmacology of a liposomal preparation?
- Liposomal AmpB has liposomes which are spherical bilayered preparations of phospholipids and cholesterol
- The drug is embedded evenly into the spherical molecules
-
Q. Does Liposomal AmpB also produce reactions on infusion?
- Yes.
- However, the reaction is different from non-liposomal preparation- it is a form of type 1 hypersensitivity reaction
- Requires stopping of infusion and anti-histaminic/glucocorticoids
-
Q. Does it produce an electrolyte imbalance?
- Yes
-
Q. What is one peculiar lab anomaly that occurs with Liposomal AmpB?
- It may produce false elevation of phosphate levels
-
Q. What are the usual doses of Liposomal AmpB in mucormycosis?
- IV: 5 to 10 mg/kg/day
- 10 mg/kg/day recommended for patients with CNS disease or solid organ transplant recipients.
- Treatment duration is typically weeks to months depending on the response
-
Q. Does it require dose adjustment in Hepatic or renal diseases?
- No
-
Q. How long is the infusion of Liposomal AmpB given?
- While the standard non-liposomal AmpB has to be given over 4-6 hours, Liposomal AmpB can be given over 2 hours (over one hour also for patients who are tolerating it well earlier)
-
Q. What is the concentration of the solution that must be prepared for liposomal AmpB?
- 0.5-2 mg/ml
-
Q. How is Liposomal AmpB reconstituted?
- 12 ml of sterile water (NOT NORMAL SALINE) is mixed with the vial to yield 4 mg/ml of the preparation
- This is shaken vigorously for 30 seconds to disperse the content and make a yellow translucent solution
- This is further diluted in 5% Dextrose to produce a 0.5-2 mg/ml suspension
- A 5-micron filter is provided with the syringe - the contents are injected via this filter to the 5% Dextrose
- The filter must be used only ONCE for one vial
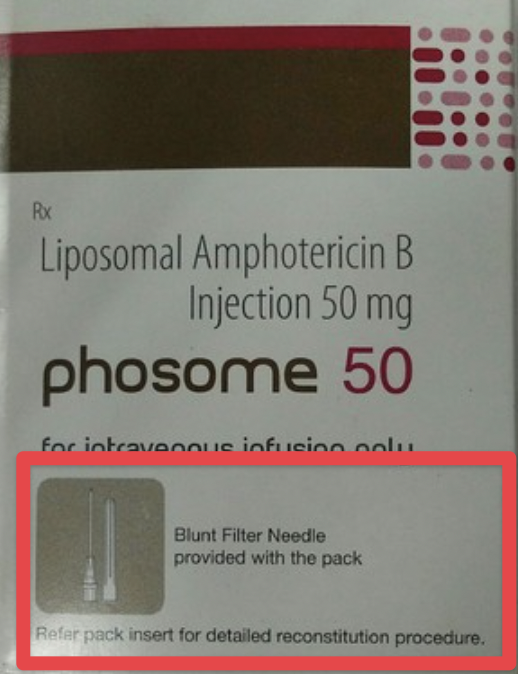
- An in-line membrane filter must be used for IV infusion. The diameter of this filter must be >1 micron
-
Q. Give the preparation for Liposomal AmpB available in India?
- Ambisome Injection - 50 mg vial
- Phosome 50mg Injection
-
Q. What is the difference in the price of Liposomal AmpB versus conventional AmpB in India?
- Liposomal AmpB costs Rs. 3000-5000 per vial while conventional costs Rs 300-500 per vial (10 times cost)
-
Q. What care do you have to take when Liposomal AmpB is given with corticosteroids?
- Watch for Hypokalemia
-
COVD-19 and Mucormycosis
-
Q. Apart from mucormycosi
- s, which another secondary infection is commonly being seen in patients with COVID-19 given steroids?
- Pulmonary aspergillosis
- Candida albicans
-
Q. What is the most common predisposing factor for the development of mucormycosis in patients with COVID-19 infection?
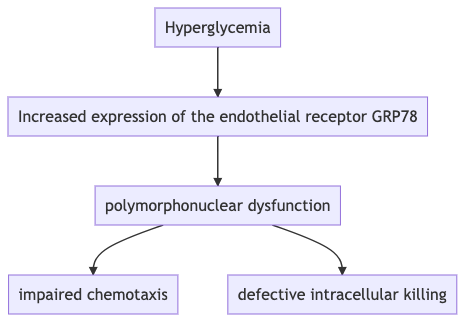
- Hyperglycemia is the strongest risk factor for the development of an epidemic of mucormycosis in patients with COVID-19 infection
- 47% of Indians are unaware of their underlying diabetes
- Many of them are found to have diabetes and severe hyperglycemia secondary to COVID-19 itself and administered glucocorticoids
-
Q. Why does hyperglycemia provide a conducive environment for infections?
-
Q. How do glucocorticoids increase the risk of infections?
- Glucocorticoids also impact Polymorphs function - it leads to Impairment in the neutrophil migration ingestion, and phagolysosome fusion
Author's personal views
We are seeing a massive upsurge in cases of Mucormycosis after COVID-19 infection. There are many theories for the same, however, one of the most important reasons is undiagnosed and untreated hyperglycemia. 47% of India's population is NOT AWARE that they have diabetes. Many of them are then given glucocorticoids without paying heed to their glycemic status. In all cases of diabetes (steroid-induced or otherwise) the only thing that works is pre-emptive or preventive action. Once the Glucose Toxicity (Glucotoxicity) cycle begins, it is difficult to bring it back to base level for several days. A simple act of checking a random sugar before the first dose of steroid and pre-empting the action of steroid can go a long way in preventing severe hyperglycemia and hopefully Mucormycosis. We will come out with a note on the management of hyperglycemia in COVID-19 soon
- Q. What can be done to prevent more cases of mucormycosis secondary to COVID-19 infection ? (Expert opinion) ?
-
- Rhino-oculo-cerebral mucormycosis is a diabetes defining illness. Mucormycoisis without diabetes or hematological disorder is very rare. Many of the patients with mucormycosis have undiagnosed diabetes mellitus. It is imperative that all patients with COVID-19 and all patients with mucomycosis be checked for Diabetes mellitus
-
- Patients given glucocortoicoids for home-care or in hospitals, must be checked for diabetes BEFORE starting the glucocorticoids. If they do have diabetes, the glucose should be intensely controlled. Expert opinion may be sought if management of hyperglycemia poses serious challenges.
-
- Statins may have a role in prevention of mucormycosis. It is also important to remember that statins are INDICATED in almost all adult patients with diabetes mellitus since people living with diabetes are considered to have high cardiovascular risk. Administration of statins in patients with diabetes mellitus should be considered a priority,
-
- Simple diagnostic and dosing recommendation and practical points thanks to Dr Lav Selarka
- Date: Tuesday, 11 May 2021!


- Patient with Mucormycosis post COVID-19. The interesting thing about this patient is that the patient had uncontrolled diabetes mellitus and COVID-19 and home treated, **but was NOT GIVEN STEROIDS. **
- Hyperglycemia seems to be the important parameter for Post-COVID-19 mucormycosis and NOT steroids themselves
Please consider donating to "Notes in Endocrinology" to keep us going. Please visit our DONATION page to know more
For more such notes in Endocrinology and Diabetes please visit our website www.endocrinology.co.in
For updates to the notes please visit https://shrtm.nu/JUYE
We have tried to be as comprehensive as possible. In case we have missed any key point, or made any error please do share with us at dromlakhani@gmail.com. We will update the note and will add your name in the credits.
Please do share with other doctors as we believe this could be very useful for COVID-19 warriors.