Fibrocalculous Pancreatic Diabetes
Author: Dr. Om J Lakhani
Updated: #jan2025
If you find this useful, please use the link to see the various ways in which you can Support us →
-
Q. What is the definition of Fibrocalculous pancreatic diabetes (FCPD)?
- Diabetes associated with non-alcoholic calcific pancreatitis seen in developing countries
-
Q. What is the prediabetic form of FCPD?
- It is called tropical calcific pancreatitis (TCP)
-
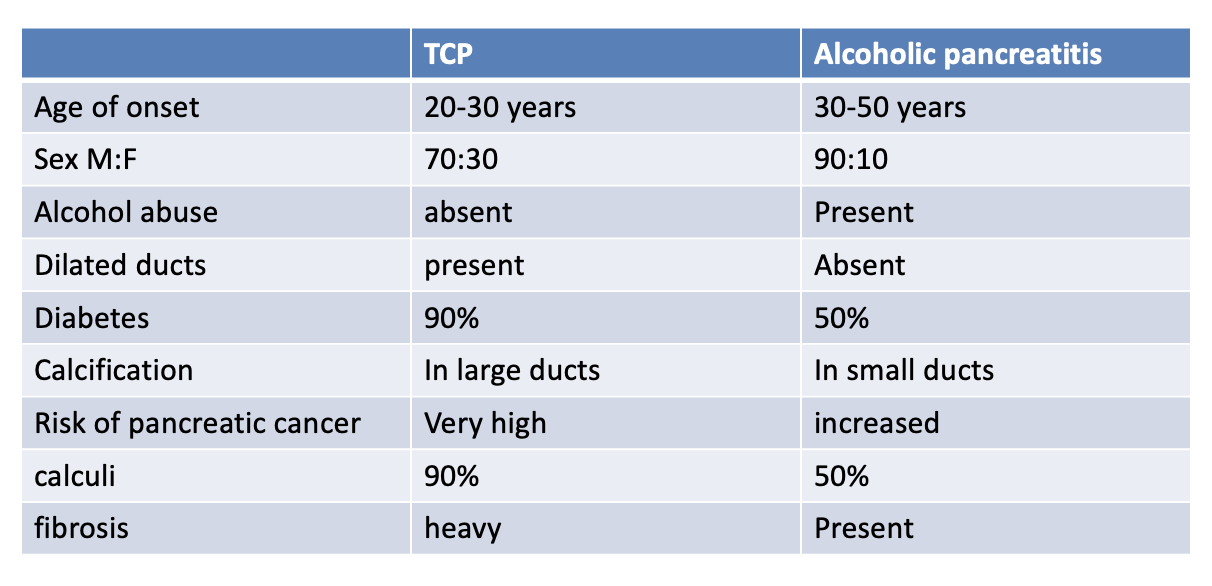
Q. Give the difference between TCP and Alcoholic pancreatitis?
-
Q. Who is the father of FCPD?
- Geeverghese
-
Q. Which are the two types of malnutrition-related DM (MRDM)?
- Fibrocalculous pancreatic diabetes
- Protein deficient diabetes mellitus
-
Q. What is the typical triad of FCPD?
- Abdominal pain - the first symptom - in childhood
- Pancreatic calculi - in adolescent
- Diabetes - in adulthood
-
Q. Where is the calcification seen in Plain X-ray in FCPD?
- Close to L1/L2 vertebra
-
Q. Ketosis is present in FCPD. True or false?
- False
- Patients with FCPD do not develop ketosis
-
Q. Intake of which food substance is implicated in causing FCPD?
- Cassava
-
Q. Which cancer risk is increased in FCPD?
- Pancreatic cancer
-
Q. There are no microvascular complications in FCPD, True or false?
- False
- It was believed earlier but not so anymore
- Microvascular complications are very much present in patients with FCPD
-
Q. What are the diagnostic criteria for FCPD?
- As given by Mohan et al
- Essential criteria
- Diabetes present
- Patient from a tropical country
- Absence of any other cause of pancreatitis
- Any 3 of the following
- Abnormal morphology of pancreas on imaging
- Abnormal pancreatic function test
- Abdominal pain - recurrent since childhood
- Steatorrhea
- Essential criteria
- As given by Mohan et al
-
Q. Which is the tumor marker for pancreatic cancer?
- CA 19-9
-
Q. What is the classical clinical description of a patient with FCPD?
- Cyanotic hue
- Emaciated
- Parotidomegaly
- Abdominal distention
-
Q. Why is there no ketosis in FCPD?
- Some of the theories for absence of ketosis in FCPD are as follows
- No non-esterified fatty acid hence less substrate for ketosis
- Also, there is reduced glucagon along with insulin
- High glucagon and reduced insulin is required for ketosis to develop
- The fat present is resistant to lipolysis
- There is some residual beta-cell function
- Carnitine deficiency - prevents fatty acid entering the mitochondria for beta-oxidation
- Some of the theories for absence of ketosis in FCPD are as follows
-
Q. Is the calcification present in the parenchyma or in the duct?
- FCPD - in the duct
- Alcoholic pancreatitis - in the parenchyma
-
Q. What is the composition of the calculi?
- It is composed of calcium carbonate
-
Q. Can ERCP and EUS be used to define pancreatic morphology in FCPD?
- Yes
-
Q. Which is the invasive test for detecting pancreatic function?
- Injection of secretin and Pancreozymin
- Collection of pancreatic juice
- Juice contains less of lipase, bicarbonate, and trypsin compared to normal
-
Q. Which are non-invasive (tubeless tests for pancreatic function)?
- BT-PABA (Bentriomide para aminobenzoic acid) - Urine / plasma
- Fecal elastase
- Fecal chymotrypsin
-
Q. Which is the gold standard tubeless test?
- Fecal elastase
-
Q. How is endocrine pancreatic function tested for in FCPD?
- Using C-peptide
- The value is intermediate between type 1 and type 2 - suggestive of residual pancreatic function
-
Q. What is done for abdominal pain in FCPD?
- It occurs earlier
- Non-opioid / opioid analgesics are used
- It resolves once the endocrine dysfunction occurs
- Pancreatic enzyme supplementation does not reduce the pain
-
Q. What is done for non-resolving pain?
- ESWL + ERCP
- Celiac plexus block
- Surgery drainage procedures - ductal decompression or pancreaticojejunostomy
- Surgery ablative procedures - partial or subtotal pancreatectomy
-
Q. What is done for the management of steatorrhea?
- Pancreatic enzyme supplementation
- Reduce diet fat
- Give vitamins
-
Q. What is the dose of pancreatic enzyme supplementation in these patients?
- Typical brand name is "Creon" 10,000 units before each meal
-
In clinical practice, it is observed that giving pancreatic enzyme supplements also has some beneficial effect on glycemic control. Some experts have suggested a link between the exocrine and endocrine dysfunctions.
-
Q. What is the best treatment of diabetes in these patients?
- 85% require insulin
- Some may do well with OAD because of residual pancreatic function
- However, incretin-based therapies are best avoided
- They often have brittle diabetes and are prone to hypoglycemia
-
Q. What is done for nutrition?
- Diet rich in proteins and carbs are given to combat the malnutrition
- Fat-soluble vitamins
- Avoid fat - to reduce steatorrhea
-
Q. Enlist the pathogenic factors for FCPD?
- Malnutrition
- Protein deficiency
- Cassava toxicity
- Oxidative stress
- Genetic and familial causes
-
Q. Which are the cyanogenic glycosides present in cassava?
- Linamarin
- Lotaustralin
-
Q. What are the investigations done to diagnose FCPD?
- Tests to detect pancreatic function
- Test to detect pancreatic morphology - X-ray, USG, EUS, ERCP, etc
-
Q. Which are the tests to detect pancreatic function?
- Fecal elastase
- Fecal chymotrypsin
- Fecal immunoreactive lipase
-
Q. Enlist the complications associated with FCPD?
- Pancreatic cancer - 100 times increased risk
- Retinopathy and other microvascular complications
- Pancreatic osteodystrophy - malnutrition + malabsorption + diabetes = severe osteoporosis
- Pancreatic exocrine deficiency
-
Q. Enlist the treatment options for FCPD?
- Diabetes management
- Exocrine pancreatic enzyme replacement
- Fat-soluble vitamin replacement - intramuscularly
- Pain management
- Endotherapy - ESWL + ERCP
- Early cancer detection
- Surgical therapy - mainly for the pain
-
Date: Monday, 19 April 2021
-
Source: Review article: Emerging concepts in the pathogenesis of diabetes in fibrocalculous pancreatic diabetes [1]
-
Q. Is malnutrition a cause or effect of FCPD?
- Recent studies suggest malnutrition is an effect rather than the cause of FCPD
-
Q. Enlist the various theories for FCPD over time?
- Cassava theory - Geerverghese and McMillin
- Increase oxidative stress theory
- Genetic theory - recent theory
-
Q. Which genetic mutation has been associated with FCPD?
- SPINK1
- PRSS1 and PRSS2
- Chymotrypsinogen C
-
Q. Diabetes onset is at what age?
- Generally age 20-30 years
- About 1-2 decades after the first episode of abdominal pain
-
Q. Is insulin secretory defect established in FCPD?
- Yes
-
Q. Is the exocrine and endocrine deficiency linked?
- It seems from some of the studies done by Yajnik et al
-
Q. What is the newer paradigm in the etiology of diabetes in FCPD?
- New interest in FCPD is directed to insulin resistance as a cause of diabetes in FCPD
-
Q. What is the link between insulin resistance and chronic pancreatitis?
- Some studies have shown that patients with pancreatic diabetes have hepatic insulin resistance due to internalization of hepatic insulin receptors and GLUT2
- The role of the pancreatic polypeptide has also been proposed
-
Q. What is the role of a pancreatic polypeptide?
- Studies have shown that pancreatic polypeptide regulates the expression of the IR gene in the liver
- Thus, impairment of PP will impair glucose homeostasis via IR gene expression in the liver
-
Q. Do patients with FCPD have insulin resistance similar to Type 2 diabetes patients?
- Yes
- This is according to a study by Mohan et al
- So FCPD patients have insulin resistance similar to type 2 diabetics!
-
Q. Is the BMI in these patients showing something else?
- Singla et al. showed that these patients have a higher body fat percentage despite low BMI
- This could contribute to the insulin resistance
-
Q. What is the vicious cycle of glucagon and insulin?
- As far as 35 years ago, it was proposed that diabetes is not just an insulin problem but also a problem with glucagon
- Insulin resistance increases insulin production and secretion → higher intra-islet insulin concentration → increase glucagon production → further increase insulin secretion → vicious circle
-
Q. Is glucagon indeed depleted in patients with FCPD?
- This theory is questioned now
- Some studies by Mohan and Yajnik have shown that FCPD may have preserved glucagon response and selective damage to beta cells
-
Q. What is the role of incretin hormones in the pathogenesis of diabetes in chronic pancreatitis?
- Knop et al. suggested that CP without diabetes had an intact incretin response compared to CP with diabetes
- This may be the missing link in FCPD
- Also, he showed that pancreatic enzyme replacement might augment incretin response - a theory that could have an impact on the management of FCPD
-
Q. What is the role of body composition causing diabetes in FCPD?
- There is a theory that the lack of fat tissue may be due to a lipodystrophy-like effect, which can lead to insulin resistance in FCPD patients
- Deficiency of fat stores increases hepatic triglyceride stores → increases circulating fatty acids → improves insulin resistance
- Date: Monday, 19 April 2021
- A 30-year-old male presented with a history of unintentional weight loss
- His weight reduced from 100 kg to 70 kg over a period of 3 months
- During this process, the patient was found to have hyperglycemia
- The patient was started on insulin, some weight was regained but over a few weeks, he started developing hypoglycemia
- Insulin was stopped, and the patient was started on oral antidiabetics by his physician
- At the age of 25, he had recurrent episodes of abdominal pain which were never investigated
- When he came to us, he had an HbA1c of 10%
- Looking at the unusual history, we decided to perform a CT scan of the abdomen
- True to what we suspected, we found the pancreas studded with calcification
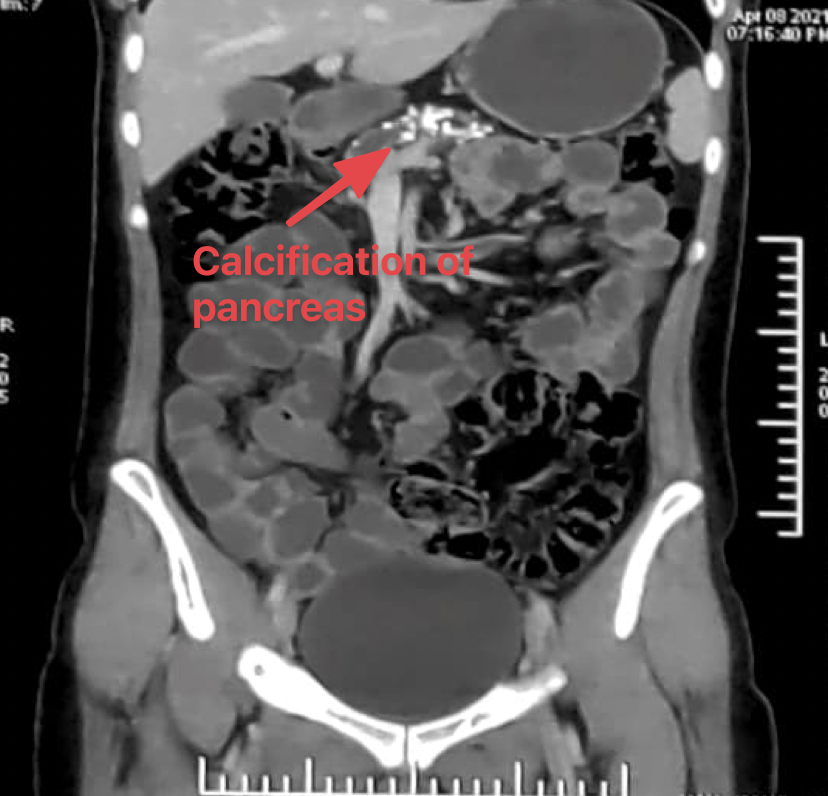
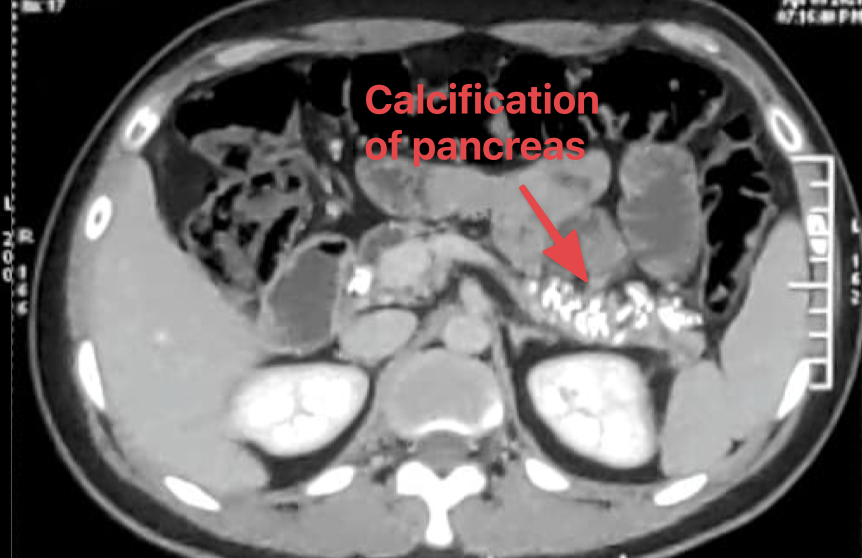
- There was no evidence of malignancy - however, the risk and screening for the same have been explained to the patient
- The patient was restarted on insulin and pancreatic enzyme supplementation along with nutritional replenishment
- Currently, he has regained some weight and maintains good glycemic control
Things to learn from the case:
- Sometimes a diagnosis of FCPD can be made retrospectively!
- In patients with acute symptomatic hyperglycemia - if the Glucose Toxicity (Glucotoxicity) breaks - the patient can start developing hypoglycemia. The risk of hypoglycemia is higher in patients with FCPD
- Abdominal pain can disappear over a period of time. At a later age, the patient may present with just exocrine and endocrine insufficiency
- This patient is from Rajasthan. FCPD is not restricted to some regions of the country and can be considered a pan-Indian issue
- Date: Friday, 9 July 2021
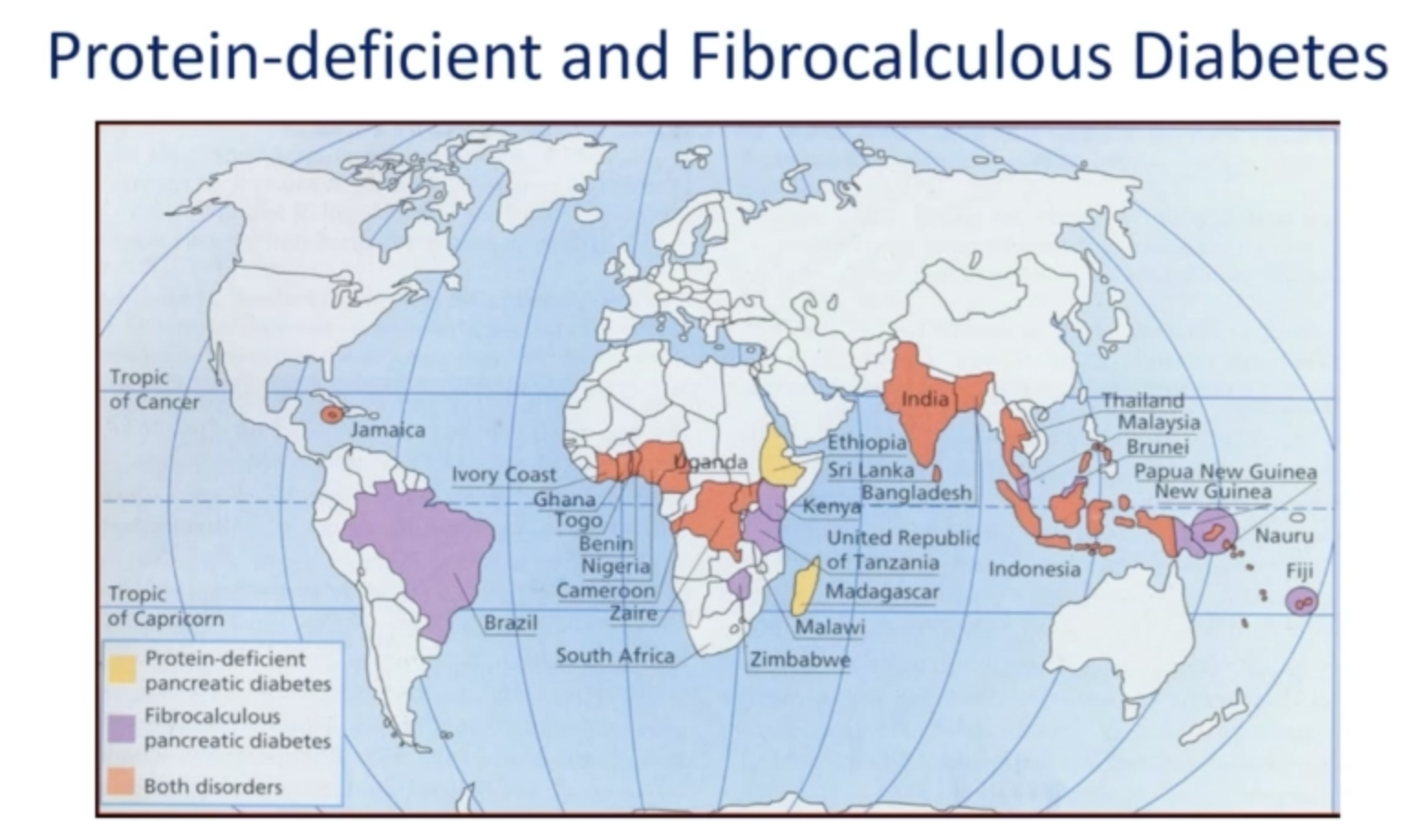
- Q. Can you give a map of regions in the world in which Fibrocalculous pancreatic diabetes is seen?
Multiple-Choice Questions
-
Question: What is the prediabetic form of Fibrocalculous Pancreatic Diabetes (FCPD)?
A. Type 1 Diabetes
B. Tropical Calcific Pancreatitis (TCP)
C. Alcoholic Pancreatitis
D. Protein Deficient Diabetes Mellitus
Correct Answer: B
Explanation: Tropical Calcific Pancreatitis (TCP) is the prediabetic form of FCPD, characterized by non-alcoholic calcific pancreatitis, which eventually progresses to diabetes. -
Question: Which of the following is a characteristic triad of Fibrocalculous Pancreatic Diabetes (FCPD)?
A. Abdominal pain in childhood, pancreatic calculi in adolescence, diabetes in adulthood
B. Abdominal pain in adulthood, pancreatic calculi in childhood, diabetes in adolescence
C. Diabetes in childhood, abdominal pain in adolescence, pancreatic calculi in adulthood
D. Pancreatic calculi in childhood, diabetes in adolescence, abdominal pain in adulthood
Correct Answer: A
Explanation: The typical triad of FCPD includes abdominal pain in childhood, pancreatic calculi in adolescence, and diabetes in adulthood. -
Question: Which of the following is true regarding ketosis in Fibrocalculous Pancreatic Diabetes (FCPD)?
A. Ketosis is common in FCPD due to insulin deficiency
B. Ketosis is absent in FCPD due to residual beta-cell function and other factors
C. Ketosis is present in FCPD due to high glucagon levels
D. Ketosis is present in FCPD due to malnutrition
Correct Answer: B
Explanation: Patients with FCPD do not develop ketosis due to residual beta-cell function, reduced glucagon levels, and other factors such as carnitine deficiency and resistance to lipolysis.
Dasgupta R, Naik D, Thomas N. Emerging concepts in the pathogenesis of diabetes in fibrocalculous pancreatic diabetes. J Diabetes. 2015 Nov;7(6):754-61. doi: 10.1111/1753-0407.12280. Epub 2015 May 6. PMID: 25707547. ↩︎