-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Important points:
- The diabetes in Cystic fibrosis is unique, having features of both type 1 and type 2 diabetes.
- However, patients with CF usually don't develop complete insulinopenia, making ketosis rare.
- Impaired glucose tolerance often develops first without accompanying fasting hyperglycemia. This progresses to impaired glucose tolerance with elevated fasting glucose levels, eventually leading to frank diabetes.
- The preferred screening method for patients with CF is the 2-hour 75-g oral glucose tolerance test.
- Hemoglobin A1c testing isn't sensitive and shouldn't be used for screening or diagnosing CFRD. #ClinicalPearl
- Consensus guidelines recommend screening for CFRD starting at age 10, though some CF centers begin screening at a younger age.
-
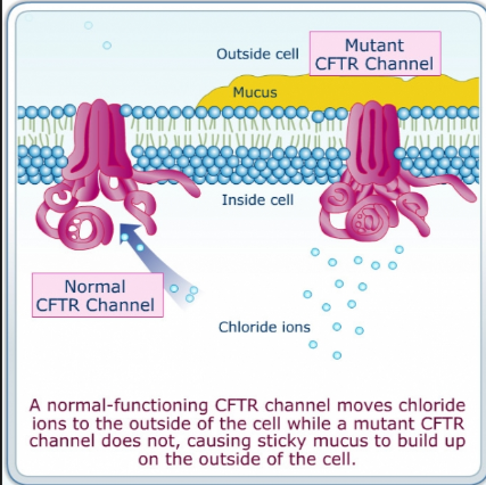
Q. What is the etiology of Cystic fibrosis?
- It results from a deficiency of the CFTR protein.
- This causes defective chloride transport.
- This defect makes secretions from various body organs thick and viscous.
-
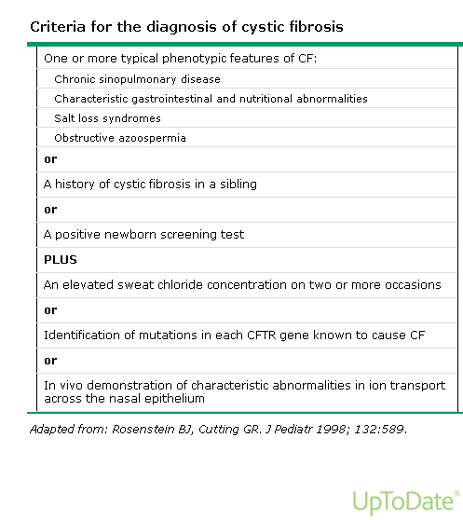
Q. How is the diagnosis of Cystic fibrosis established?
-
Q. List the systems involved in Cystic fibrosis.
- Pulmonary: bronchiectasis, sinusitis, recurrent pulmonary infections.
- GIT: recurrent pancreatitis, malabsorption.
- Endocrine: diabetes, osteoporosis.
- Genitourinary: absent vas deferens, infertility in both males and females.
-
Q. What is the mode of inheritance?
- Autosomal recessive.
- Multiple genes can lead to the clinical picture, resulting in variable clinical symptoms.
-
Q. Which is the primary investigation to diagnose cystic fibrosis?
- Elevated sweat chloride > 60 mmol/l confirms Cystic fibrosis.
-
Q. At what age does diabetes typically occur in cystic fibrosis?
- Middle school age and older.
-
Q. What is the etiology of diabetes in cystic fibrosis?
- Progressive destruction and fibrosis of the pancreas.
-
Q. Which clinical points are potentially related to Diabetes in cystic fibrosis?
- Presence of respiratory disease.
- Presence of pancreatic insufficiency.
-
Q. What are the consequences of diabetes on other manifestations of cystic fibrosis?
- Increased pulmonary infections and insufficiency.
- Increased mortality.
- Worsened nutritional status.
-
Q. How is screening for diabetes in cystic fibrosis conducted?
- Annually using OGTT starting at 10 years of age.
- HbA1c isn't used due to its low sensitivity in cystic fibrosis.
- During pregnancy.
- During pulmonary exacerbations.
- Annually using OGTT starting at 10 years of age.
-
Q. What is the clinical definition of diabetes in cystic fibrosis?
- Fasting >125 mg/dl – OGTT isn't needed.
- 2hr PG2BS in OGTT >200 mg/dl – confirms diabetes with or without fasting hyperglycemia.
-
Q. What is indeterminate hyperglycemia in cystic fibrosis?
- 1 hr OGTT >200.
- 2 hr <140.
-
Q. What is the management of choice for patients with CFRD?
- Insulin is the preferred treatment.
-
Q. Should insulin be used in patients with indeterminate hyperglycemia or IGT?
- In selected cases, insulin is initiated.
- Especially in those experiencing pulmonary exacerbations.
- It enhances nutritional status.
-
Q. Why are CFRD patients at a higher risk of hypoglycemia?
- Poor nutritional intake and glycogen stores lead to fasting hypoglycemia.
- Disordered insulin release results in reactive hypoglycemia post meals.
- Reduced glucagon response (though catecholamine response remains normal).
-
Q. What is the primary goal of therapy in CFRD with insulin?
- The main objective is to maintain nutritional status (avoiding excessive catabolism).
- To prevent pulmonary exacerbations.
- This contrasts with type 1 diabetes, where the primary therapy goal is preventing microvascular complications.
-
Q. What is the therapy goal?
- Keep HBA1c as low as possible (it's not used for diagnosis but for monitoring) – ideally below 5.5% if achievable without hypoglycemia.
- Reduce postprandial BG – ideally measured 1 hr post meal, aiming for <140 mg/dl.
- Maintain fasting levels between 70-90 mg/dl.
-
Q. How and when is screening for microvascular disease conducted?
- 5 years after diagnosing CFRD.
-
Q. True or false, does insulin treatment in CFRD improve the overall outcome and lung functions?
- True.