- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
-
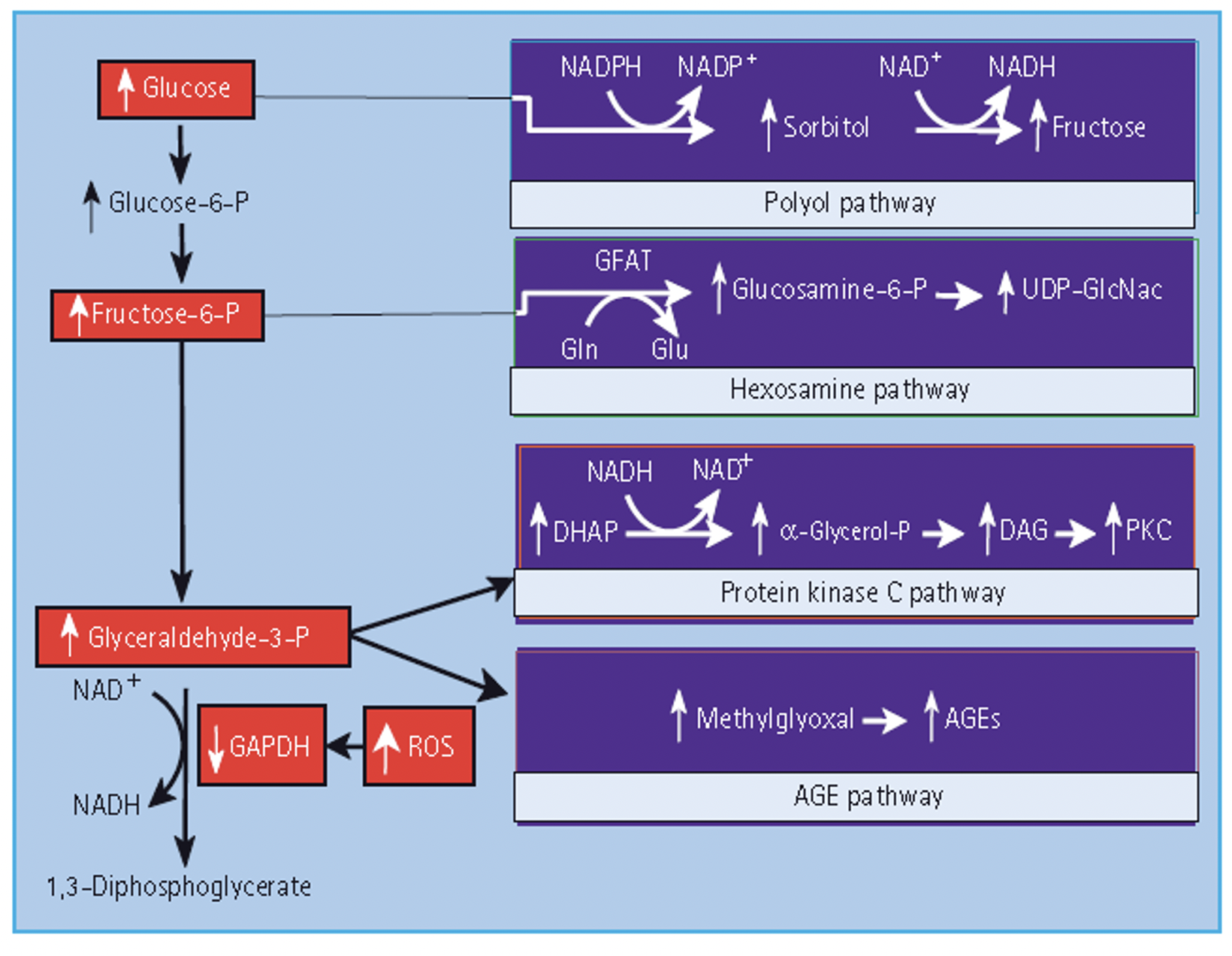
Q. Which are the primary pathways implicated in hyperglycemia-induced microvascular damage?
- Accumulation of Advanced Glycation End Products (AGEs)
- Accumulation of sorbitol (Polyol flux pathway)
- Hexosamine flux pathway
- Increase protein kinase C
-
**Polyol flux pathway **
-
Q. Describe the sorbitol pathway?
- Glucose is converted by Aldose reductase into sorbitol
-
Q. What are the consequence of sorbitol accumulation?
- Depletion of NADPH
- Increased cell osmolality
- Decrease in intracellular myoinositol
-
Q. Why is depletion of NADPH critical?
- NADPH is required for scavenging of radical oxygen species
- Reduction of NADPH reduces the ability of the cell to scavenge reactive oxygen species
-
Q. Summarize the polyol flux pathway with a diagram
-
Q. Give the sequence of formation of AGE?
-
Q. Which are the three precursors of AGE?
- Glyoxal
- Methylglyoxal
- 3-Deoxyglucosone
-
Q. What are RAGE?
- Receptor for AGE
-
Q. Describe the consequences of AGE?
- Glucose binds to protein formation of AGE:
- Crosslinking of AGE
- AGE binding with RAGE → proinflammatory pathway activated
-
**Hexosamine pathway **
-
Q. Describe the Hexosamine flux pathway?
-
Q. What does UDP N glucosamine do ?
- UDP N- glucosamine glycosylates transcription factors leading to increased transcription of certain proteins like TGF-beta, PAI-1, etc
-
Q. What happens to the hexosamine pathway?
- Increase in glucose leads to increase flux through the hexosamine pathway
- This leads to increase in the formation of ROS and disruption of various cell transcription factor
-
Q. Which drug reduces the flux of glucose via the hexosamine pathway?
- Benfotiamine
-
**Protein kinase c **
-
Q. What is the importance of protein kinase C?
- Increase glucose increase diacylglycerol → increase protein kinase C
-
Q. What are the consequences of protein Kinase C activation?
- Increase VEGF
- Increase TGF beta
- Increase NAPH oxidases increase ROS
- Increase PAI-1 → increase thrombosis
- Increase Nk-kb → increase proinflammatory cytokines
- increased endothelin 1 →vasoconstriction
-
Q. Which is the protein kinase C inhibitor?
- Ruboxistaurin
-
Q. Does the protein kinase C pathway affect microvascular complications only?
- No
- It can lead to both microvascular and macrovascular complications
-
Q. What isoforms of PKC produce what in diabetic nephropathy?
- PKC alpha- albuminuria
- PKC beta – glomerular hypertrophy and mesangial expansion
- Both increase reactive oxygen species
-
Q. Describe the IP3 /DAG pathway?
- DAG is increased in Diabetes and hence more production of Protein Kinase C
-
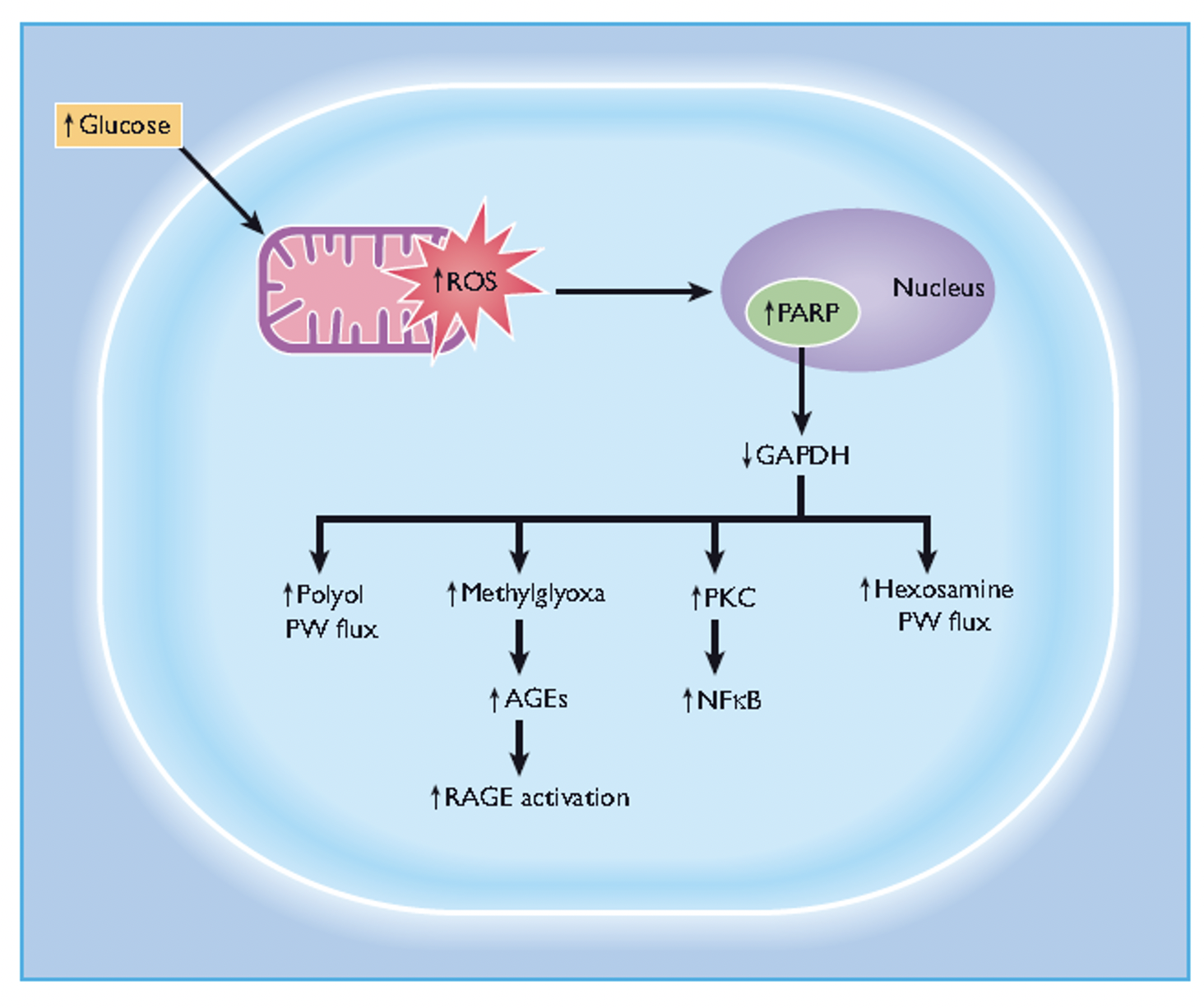
**Oxidative stress **
-
Q. What is the role of oxidative stress in the whole process?
- Oxidative stress in the final common pathway for all the metabolic processes described above
-
PARP (Poly-ADP ribose polymerase)
-
Q. What is PARP?
- Poly-ADP ribose polymerase
-
Q. What is the role of PARP in diabetic neuropathy?
- Increased glucose activates PARP
- PARP destroys NAD+
- This leads to increase free radicals and disruption of the DNA transcription process
- It also reduced G6PDH, which is a critical pathogenic factor
-
Q. What is the importance of G6PDH?
- Glyceraldehyde 6 phosphate dehydrogenase is a crucial enzyme in the glucose metabolism
- This is inhibited by PARP
- This leads to the accumulation of Glyceraldehyde 6 phosphate, which is shunted to produce DAG (Protein kinase C) and Methylglycoxal (which produces AGE)
-
Q. Describe some charts showing unifying pathways for diabetic microvascular complications and the role of G6PDH?