Frozen Shoulder (Adhesive Capsulitis) In Patients With Diabetes Mellitus
Author: Dr. Om J Lakhani
If you find this useful, please use the link to see the various ways in which you can Support us →
Definition and Epidemiology
-
Q. What is the definition of Frozen shoulder (adhesive capsulitis)?
- Frozen shoulder, also known as adhesive capsulitis, is a condition characterized by the gradual development of global limitation of active and passive shoulder motion.
- It is accompanied by severe shoulder pain.
- Radiographic findings other than osteopenia are absent in frozen shoulder.
- It is also referred to as painful stiff shoulder and periarthritis.
-
Q. Give me the epidemiology of Frozen shoulder (adhesive capsulitis).
- It is generally seen in the fifth and sixth decade.
- It is rare before the age of 40 years.
- It is 3 times more common in diabetes.
- Women are more affected than men.
- It is generally unilateral.
- It is generally self-limiting.
- It is more common in the non-dominant arm.
Relationship with Diabetes Mellitus
-
Q. What is the relationship between Frozen shoulder (adhesive capsulitis) and diabetes?
- Patients with diabetes mellitus are at a greater risk of developing frozen shoulder.
- Diabetics are over three times more likely to develop adhesive capsulitis compared to non-diabetics.
- The overall prevalence of frozen shoulder among diabetics is reported to be 10 to 20 percent.
- Prevalence of frozen shoulder in patients with long-lasting type 1 diabetes can be as high as 59 percent.
-
Q. Does the level of HbA1c predict the likelihood of frozen shoulder?
- No.
- According to Yian et al., "There was no association found between HbA1c level and the prevalence of frozen shoulder in this diabetic population." (See reference below)
-
Q. Which are the other conditions associated with Frozen shoulder (adhesive capsulitis)?
- Frozen shoulder has also been associated with thyroid disease, dyslipidemia, prolonged immobilization, stroke, autoimmune disease, Parkinson's disease, and antiretroviral therapy for HIV infection.
Pathophysiology
-
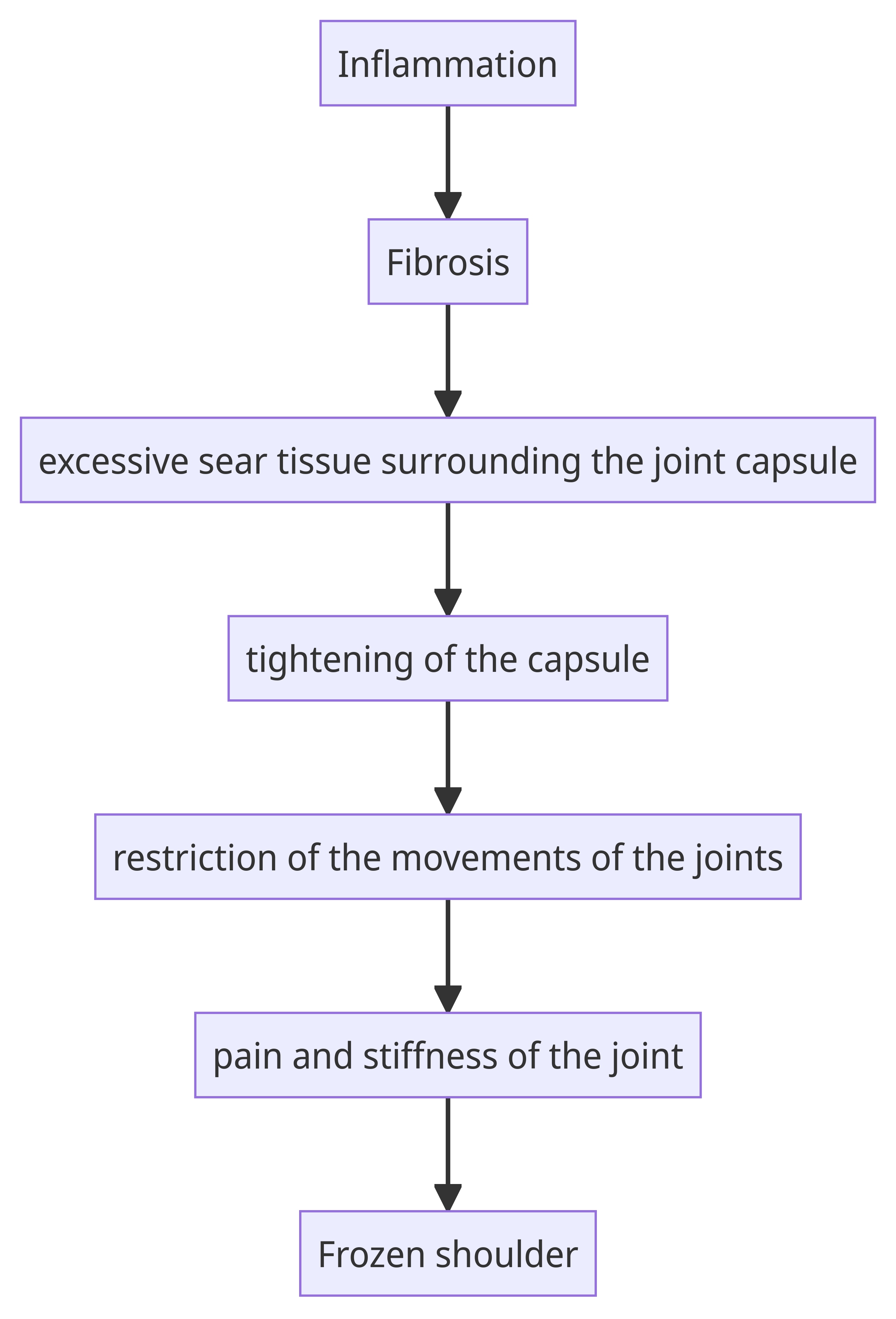
Q. What is the pathophysiology of Frozen shoulder (adhesive capsulitis)?
- Frozen shoulder, also known as adhesive capsulitis, is characterized by the thickening and tightening of the capsule surrounding the shoulder joint.
- The exact cause of frozen shoulder is not fully understood, but it is believed to involve a combination of factors including inflammation, fibrosis (formation of excessive scar tissue), and contracture (shortening and tightening) of the joint capsule.
- Inflammation within the joint leads to the release of inflammatory chemicals, which can cause pain and swelling.
- Over time, the inflammation triggers the production of excessive scar tissue within the joint capsule, leading to thickening and tightening of the capsule.
- The thickened and tight capsule restricts the normal movement of the shoulder joint, resulting in pain and stiffness.
-
Q. Is it similar to Dupuytren's contracture in its pathophysiology?
- It is possible.
- It is also thought that fibrosis is more common in diabetes.
Clinical Features
-
Q. What are the phases of frozen shoulder clinical features?
- The phases of frozen shoulder clinical features are as follows:
- Initial Phase: This phase is characterized by severe and disabling shoulder pain that is worse at night. There is also an increasing stiffness that lasts for two to nine months.
- Intermediate Phase: In this phase, the pain becomes gradually less pronounced, but there is severe loss of shoulder motion and stiffness. This phase lasts for 4 to 12 months.
- Recovery Phase: The final phase is marked by a gradual return of range of motion in the shoulder. It takes from 5 to 24 months to complete the recovery phase.
- The phases of frozen shoulder clinical features are as follows:
-
Q. What are the characteristics of the pain initially felt in patients having frozen shoulder?
- Initially, there is pain, followed by loss of motion.
- The pain is typically worse at night.
-
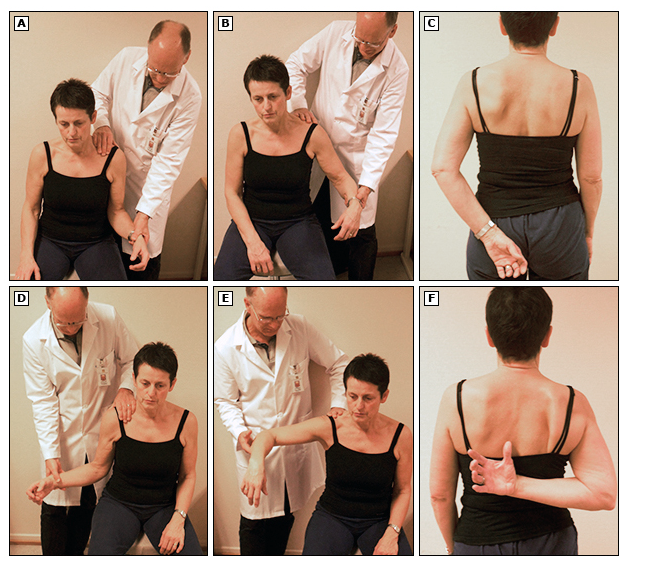
Q. Which movements of the shoulder joint are typically affected?
- External rotation
- Abduction
- The patient cannot place the hand on their back or buttock.
-
Q. Is the restriction of motion due to pain or is it true restriction of motion?
- It is true restriction and not just because of pain.
Diagnosis
-
Q. What is the "injection test"?
- The injection test is a diagnostic procedure used to distinguish between frozen shoulder and subacromial conditions.
- It involves injecting an anesthetic into the subacromial space (but outside the joint) to assess the response.
- In patients with frozen shoulder, active movement restriction and painful end detected with passive motion testing persist after the injection.
- In contrast, patients with subacromial pathology generally experience pain relief and improved range of motion after the injection.
- The injection can be performed with or without ultrasound guidance.
-
Q. Are investigations necessary for making a diagnosis of Frozen shoulder (adhesive capsulitis)?
- No.
- Investigations are optional and mainly done to rule out other conditions.
-
Q. What is the role of performing a plain x-ray in case of a frozen shoulder?
- Plain radiographs are generally of limited diagnostic use in patients with frozen shoulder.
- Most often, the plain film is normal, except for potentially ruling out other disorders such as glenohumeral osteoarthritis.
- X-rays are not typically necessary to diagnose frozen shoulder.
- MRI and ultrasound may be more helpful in revealing characteristic changes in the soft tissues consistent with frozen shoulder and assessing the rotator cuff.
-
Q. What are the MRI findings in case of frozen shoulder?
- MRI has good sensitivity and specificity in making the diagnosis. The findings include:
- Thickening of the coracohumeral ligament and the soft-tissue structures in the rotator cuff interval
- Coracohumeral ligament thickening
- Fat obliteration of the rotator cuff interval
- Enhancement of rotator cuff interval
- Enhancement of axillary joint capsule
- Hyperintensity of inferior glenohumeral ligament
- MRI has good sensitivity and specificity in making the diagnosis. The findings include:
-
Q. What are the findings on an ultrasound?
- Thickening of the coracohumeral ligament and the soft-tissue structures in the rotator cuff interval (in the early phase)
-
Q. How will you differentiate clinically frozen shoulder from subacromial conditions?
- Patients with subacromial conditions often have a history of heavy lifting or repetitive movements, especially above shoulder level.
- Patients with subacromial conditions often complain of activity-related pain and problems performing usual activities.
- Limitations in shoulder motion are more often due to pain in patients with subacromial conditions, as opposed to the mechanical restrictions found with frozen shoulder.
- Patients with frozen shoulder may have a spontaneous onset without an apparent cause or a history of overuse or abnormal activity.
- Frozen shoulder can develop following shoulder injuries, surgery, or prolonged immobilization for any reason.
- Patients with frozen shoulder often complain of chronic, severe, nagging pain deep in the shoulder joint, especially at night.
- Age can be a distinguishing factor, as frozen shoulder is unlikely in patients younger than 40 years of age, while patients older than 70 are more likely to have rotator cuff tears or glenohumeral osteoarthritis.
-
Q. What is the important difference between these conditions in terms of range of motion?
- In subacromial conditions, the limitation of motion is mainly due to pain.
- Hence, there is a reduction in active range of motion, but passive range of motion is preserved.
- However, in the case of frozen shoulder, the restriction is due to pain as well as actual restriction in movement, and hence both active and passive range of motion is affected.
- Physiotherapy is helpful after the initial painful phase is over.
Management
-
Q. What is the principle of management of Frozen shoulder (adhesive capsulitis)?
- It is generally self-resolving and does not need any treatment in most cases.
-
Q. What treatment can be offered for moderate to severe pain?
-
- Intra-articular glucocorticoids
-
- Suprascapular nerve block
-
-
Q. What is the role of physiotherapy in Frozen shoulder (adhesive capsulitis)?
- Physical therapy is commonly used to treat frozen shoulder.
- Evidence for the effectiveness of physical therapy is limited.
- A meta-analysis of 32 trials found that the efficacy of manual therapy or exercise remains unclear, with most studies reporting no significant differences among treatment groups.
- One study suggested that exercise performed within the limits of pain led to greater improvements in shoulder function than intensive physical therapy.
- More aggressive stretching of the shoulder muscles and capsule may be useful in the later phase of the condition.
- The addition of supervised physical therapy following an intraarticular injection of glucocorticoid may result in more rapid improvement than injection alone.
- Patients with mild disease and those early in the recovery phase of frozen shoulder may benefit from performing gentle range of motion exercises, such as pendulum swings, as long as they do not cause undue discomfort.
- ^^To summarize - physical therapy is useful, but only more gentle exercises rather than more aggressive situations.^^
-
Q. What kind of shoulder motion exercises are recommended?
- Gentle abduction
- Gentle external rotation
- Gentle internal rotation
- Abduction-adduction with exercise band
- Flexion-extension with exercise band
- Seated external rotation with elbow resting on table
-
Q. What is the role of oral glucocorticoid therapy?
- Oral glucocorticoid therapy is not recommended as a routine treatment for frozen shoulder.
- Intraarticular glucocorticoid injections are more effective than oral glucocorticoids for treating frozen shoulder.
- Oral glucocorticoids may have potential adverse effects.
- Intraarticular glucocorticoid injections lead to improved range of motion and pain relief in frozen shoulder.
-
Q. What is the role of intraarticular glucocorticoid injection?
- Intraarticular glucocorticoid injections are beneficial in the treatment of frozen shoulder.
- They can lead to improved range of motion and pain relief. However, the benefits are temporary.
- Multiple injections may be beneficial, with up to three injections showing evidence of effectiveness.
- Adverse reactions may include increased pain after injection, facial flushing, rash, and irregular menstrual bleeding.
- Sonographic guidance for intraarticular injections is being used more frequently and may improve effectiveness.
- Further randomized trials are needed to test the hypothesis of ultrasound-guided injections and alternative injection sites.
- Pending the results of such studies, it is suggested to use intraarticular injections.
-
Q. What is the role of glucocorticoid injection combined with physical therapy?
- Glucocorticoid injection combined with physical therapy may be more effective than either therapy alone for frozen shoulder.
- It can result in faster improvements in shoulder function compared to other treatment approaches.
- The combination therapy has shown to provide pain relief, improve range of motion, and reduce disability.
- Evidence supporting the effectiveness of glucocorticoid injection combined with physical therapy is limited but promising.
-
Q. What is the role of suprascapular nerve block?
- Suprascapular nerve block can reduce the pain associated with early frozen shoulder.
- It may provide additional benefits by addressing the involvement of the suprascapular nerve in the pathophysiology of frozen shoulder.
- A systematic review and meta-analysis showed significant improvements in pain, motion, and overall shoulder function following a suprascapular nerve block.
- In a randomized trial, patients treated with a suprascapular nerve block in addition to glenohumeral injection and physical therapy experienced reduced pain, increased mobility, and a resolution of symptoms six months sooner than patients treated with glenohumeral injection and physical therapy alone.
-
Q. What is intraarticular dilatation?
- Intraarticular dilatation, also known as hydrodilatation or arthrographic distension, is a treatment for frozen shoulder.
- It involves combining an intraarticular injection of an anesthetic with an infusion of saline to dilate the glenohumeral capsule.
- Saline is injected into the joint under pressure to increase joint volume and improve glenohumeral motion.
- It is based on the finding that frozen shoulder involves thickening and contraction of the glenohumeral joint capsule and surrounding collagenous tissue, leading to reduced joint volume.
- Studies have shown that arthrographic distension with saline and glucocorticoid provides short-term benefits in pain reduction, range of motion, and overall shoulder function in patients with frozen shoulder.
-
Q. What is the role of surgery in these cases?
- Surgical referral should be deferred as long as the patient is making progress with nonoperative management.
- Surgery should be reserved for patients who do not respond to conservative management.
- There are no formal guidelines to determine the appropriate timeframe for surgical referral.
- Most patients should be managed conservatively for at least 10 to 12 months, as long as they are making progress.
-
Q. What type of surgery is done in such cases?
- Arthroscopic release of adhesive capsulitis
- Manipulation under anesthesia
Glycemic Control and Outcomes
- Q. In patients with diabetes mellitus and frozen shoulder, how does good glycemic control improve the outcomes?
- ^^Currently, there is no evidence to suggest that improvement in glycemic control leads to improved outcomes in patients with Frozen shoulder (adhesive capsulitis).^^
Additional updates
-
Q. What is the role of nasal calcitonin spray in frozen shoulder ?
- One small study (Rouhani et al) has shown promising results for the use of calcitonin nasal spray in treating frozen shoulder (adhesive capsulitis).
- This double-blinded randomized clinical trial involving 64 patients demonstrated that intranasal calcitonin spray, when used alongside physiotherapy and NSAIDs for 6 weeks, significantly improved pain, range of motion, and functional outcomes compared to placebo.
- The treatment was found to be safe, with no significant adverse effects reported.
- While these results are encouraging, further research may be needed to fully establish the role of calcitonin nasal spray in managing adhesive capsulitis.
-
Q. What is the role of using Intra-articular steroids early in the course of the disease ?
- One recent case series explored and found that early use of Intra-articular steroids in the Stage 1 of the disease led to better outcomes
- The research article is summarized here: Ultrasound-Guided Glenohumeral Corticosteroid Injection for the Treatment of Adhesive Capsulitis of the Shoulder The Role of Clinical Stage in Response to Treatment
References
- Yian EH, Contreras R, Sodl JF. Effects of glycemic control on prevalence of diabetic frozen shoulder. J Bone Joint Surg Am. 2012 May 16;94(10):919-23. doi: 10.2106/JBJS.J.01930. PMID: 22617920.
- Rouhani A, Mardani-Kivi M, Bazavar M, Barzgar M, Tabrizi A, Hashemi-Motlagh K, Saheb-Ekhtiari K. Calcitonin effects on shoulder adhesive capsulitis. European Journal of Orthopaedic Surgery & Traumatology. 2016 Aug;26:575-80.