- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
- Q. At what stage does macular edema occur in diabetes?
- Macular edema can occur at any stage
- Q. What is Diabetic macular edema ?
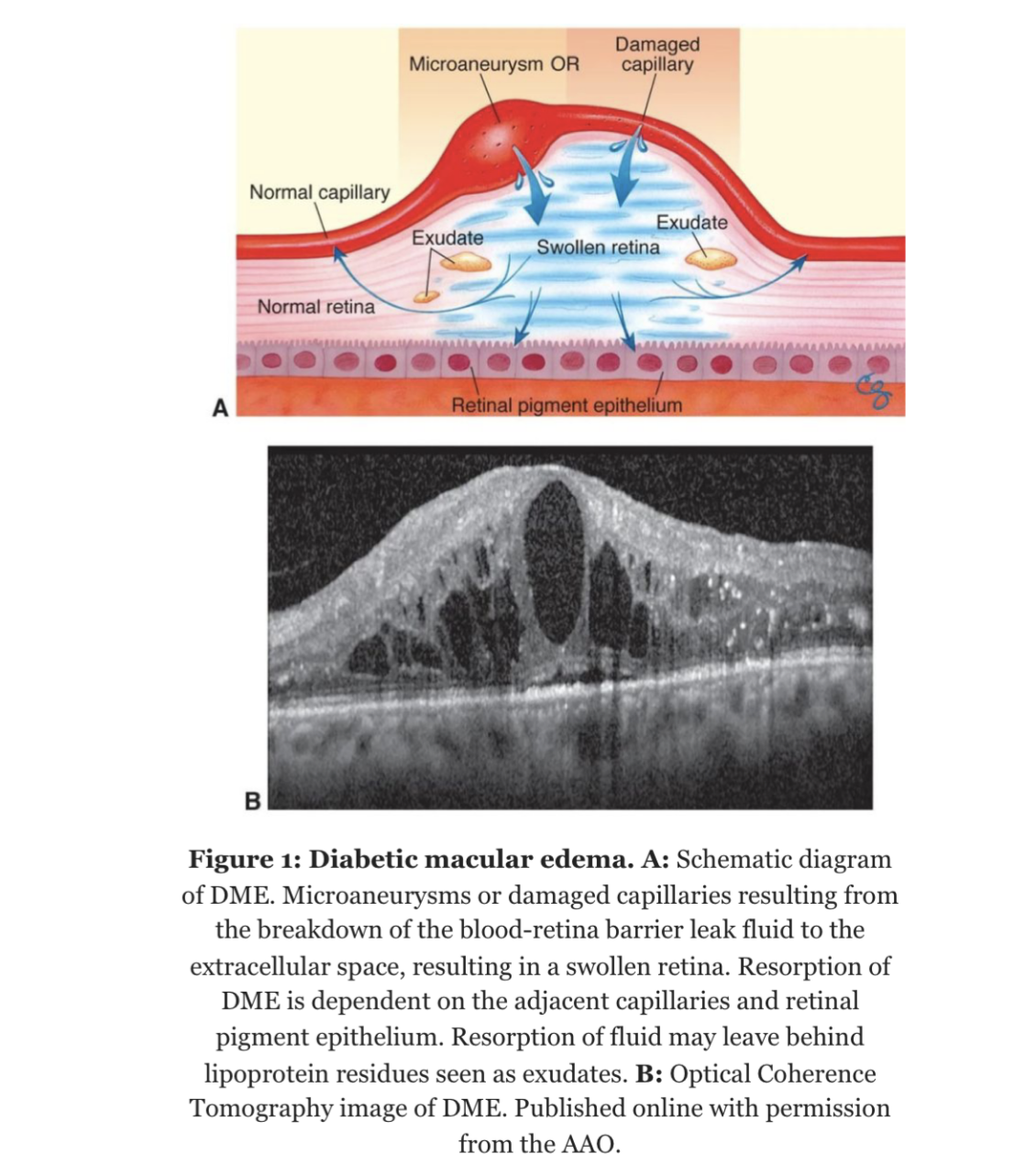
- Diabetic macular edema (DME) is the accumulation of excess fluid in the extracellular space within the retina in the macular area, typically in the inner nuclear, outer plexiform, Henle’s fiber layer, and subretinal space.
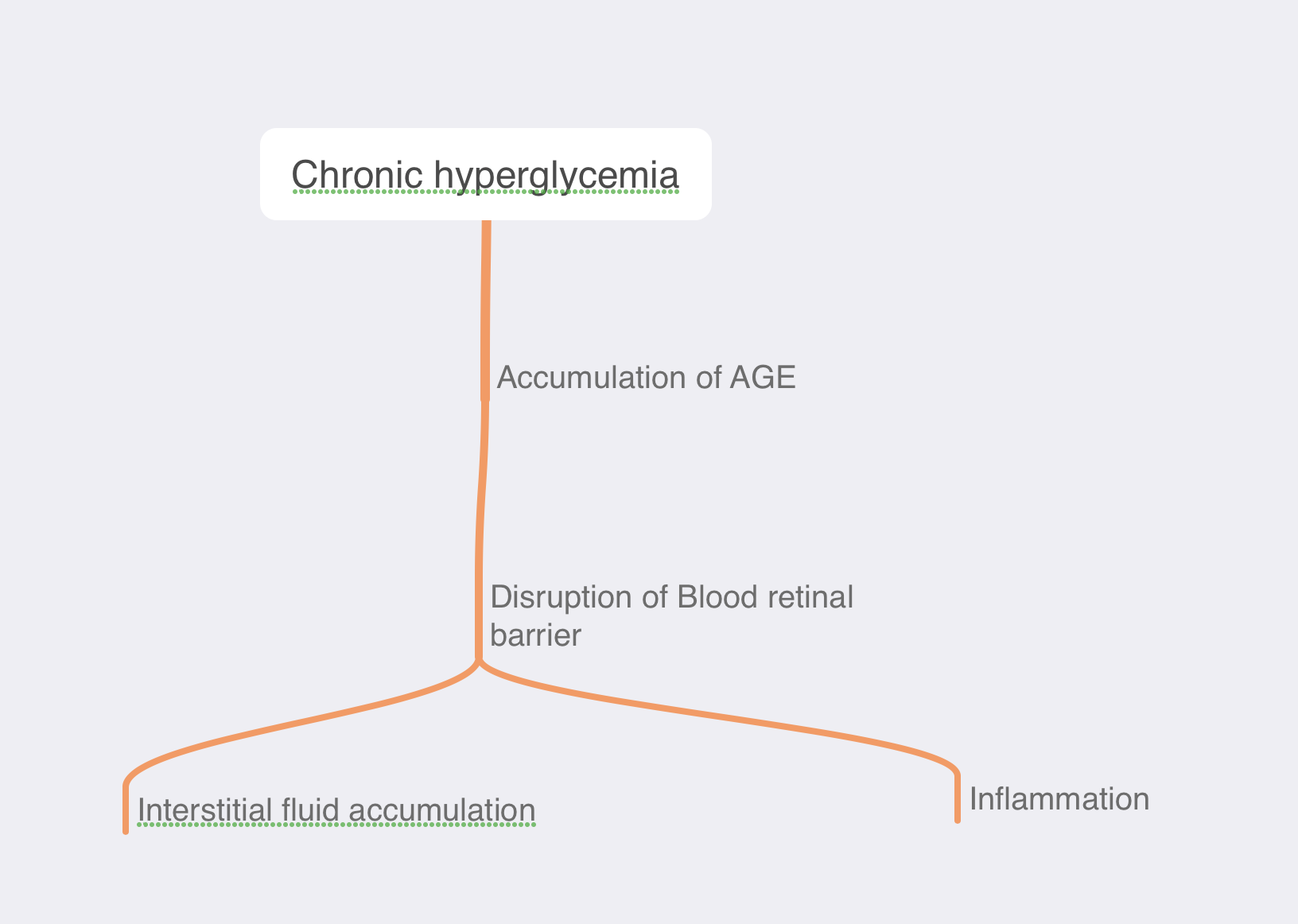
- Q. What is the pathophysiology of Diabetic macular edema ?
- Q. What are the clinical features of Diabetic macular edema ?
- Diabetic macular edema involving the fovea can cause blurred vision and metamorphopsia (a syndrome in which the shape of objects appears distorted)
- This can eventually lead to moderate to severe visual loss
- However in some patients it can be asymptomatic
- Q. What are the two most important clinical signs of macular edema?
-
- Hard exudates
-
- Retinal thickening
-
- Q. What exactly are Hard exudates ?
- Hard exudates are lipoprotein residues of serous leakage from damaged vessels, seen as biomarkers for diabetic macular edema (DME). They are typically seen in various patterns, including circinate rings and focal aggregations of exudates
- Q. What are the various patterns of retinal thickening in diabetic macular edema?
- The various patterns of retinal thickening in diabetic macular edema (DME) include focal leakage from microaneurysms or capillaries, diffuse poorly demarcated areas of capillary leakage, disorganization of the retinal inner layers (DRIL), external limiting membrane (ELM) and ellipsoid zone (EZ) disruption, and vitreomacular interface abnormalities (VMIA) such as vitreomacular adhesion (VMA), vitreomacular traction (VMT), and the epiretinal membrane (ERM)
- Q. What is the difference in terms of treatment of focal leakage versus diffuse capillary leakage in Diabetic macular edema ?
- The treatment of focal leakage in diabetic macular edema involves laser photocoagulation, which involves burning the affected area to reduce the leakage.
- The treatment of diffuse capillary leakage involves pan-retinal photocoagulation, which involves burning the peripheral retina to reduce the leakage
- Q. What are the risk factors for Diabetic macular edema ?
-
- High HbA1c
-
- Hypertension
-
- Dyslipidemia
-
- Impaired renal function
-
- use of Pioglitazone and other thiazolidinediones
-
- Q. Apart from the usual, what other treatment can be given to prevent Diabetic macular edema from developing?
- In patients with NPDR (Non-proliferative diabetic retinopathy) - the use of Anti-VEGF injections is known to prevent the development of Diabetic macular edema
- Q. How is macular edema visualized?
- Fluorescein angiography
- Optical coherence tomography- OCT
- Fundus with stereoscopic vision
- Q. What is the definition of CSME?
- Retinal thickening within 500 microns from the fovea
- Hard exudate within 500 microns from the fovea
- Retinal thicking of 1500 microns area within 1 disc diameter from the fovea
- Q. What is the name of this criteria?
- Modified Airlie house criteria
- Q. What is Wilkinson’s classification of DME?
- Mild- exudates near posterior pole but far from the macula
- Moderate- approaching the macula
- Severe – involving the macula
- Q. What is the use of Fluorescein angiography?
- Fluorescein angiography confirms the diagnosis of ME
- It also defines the area of ischemia which guides laser therapy
- Q. What does the thickness mapping in OCT designate?
- Thick areas designate capillary leakage
- It correlates with loss of visual acuity
- **Role of Optical Coherence Tomography (OCT) in Diabetic macular edema **
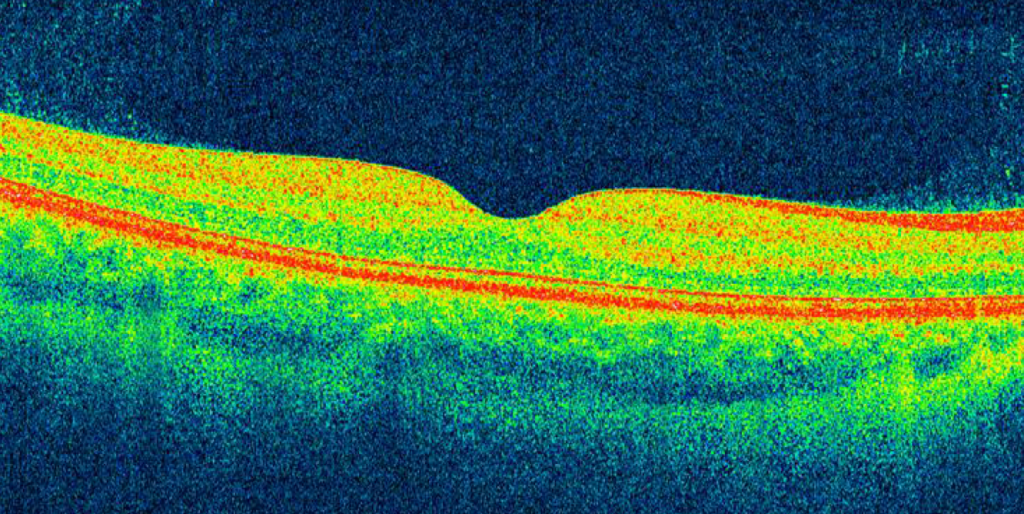
- Q. What is OCT?
- It is a non-invasive test that gives a cross-section of the retina
- Q. What technology does it use?
- It uses a concept called interferometry to create a cross-section of retina of 10-15 microns in size
- Q. What is the main use of this?
- The main use of OCT is to see macular lesions in the retina
- Macula is better to the image compared to the periphery of the retina
- Q. Which are the conditions for which OCT is used?
- Macular hole
- Macular pucker/epiretinal membrane
- Vitreomacular traction
- Macular edema and exudates
- Detachments of the neurosensory retina
- Detachments of the retinal pigment epithelium (e.g. central serous retinopathy or age-related macular degeneration)
- Retinoschisis
- Pachychoroid
- Choroidal tumors
- Q. Where is it gaining popularity?
- OCT is gaining popularity in the evaluation of optic nerve disorders
- Q. What is the main disadvantage of OCT?
- OCT uses light instead of sound which is used in ultrasound
- Hence the media needs to be clear for proper OCT imaging
- So it cannot be used if the patient has a cataract
- Q. What are the layers of the retina seen on the OCT?
- Q. What does the following OCT show?
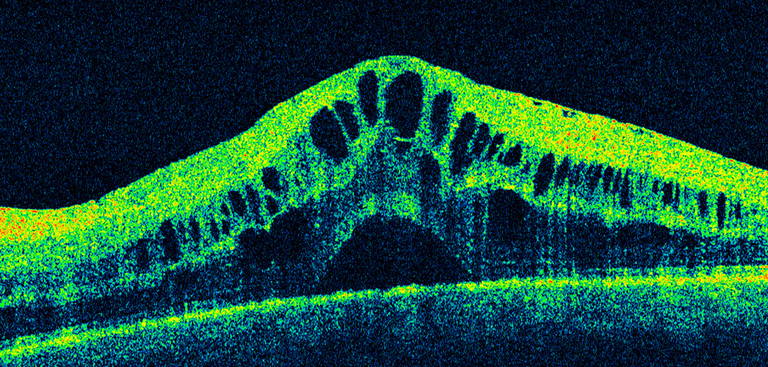
- This is an image of a classic Diabetic macular edema
- There is cystoid intraretinal fluid collection in the outer plexiform layer of the retina
- Q. What is the use of OCT in glaucoma ?
- OCT is very useful for the assessment of optic nerve for glaucoma
- It measures the nerve fiber layer thickness and cup-to-disc ratio
- it compares this to normal personal data
- This helps to track the optic nerve edema
- Q. What is the difference between the terms Cystoid macular edema, Diabetic macular edema , and Clinically significant macular edema ?
- Cystoid macular edema refers to macular edema due to any cause
- Diabetic macular edema refers to CME due to Diabetes
- Clinically significant macular edema refers to macular edema due to diabetes which fulfills the ETDRS criteria
- Q. What is the ETDRS criteria for Clinically significant macular edema ?
- Retinal thickening within 500 um of the fovea
- Hard exudates within 500 um of the fovea with associated retinal thickening
- Retina thickening greater than 1 disc area which is located within 1 disc diameter of the fovea
- Q. Do the OCT measurements correlate with vision in patients with Diabetic macular edema ?
- There is a correlation but it is generally poor to modest
- Studies have shown that eyes with disorganization of the retinal inner layers (DRIL) have a worse baseline and final visual acuity despite anti-VEGF injections and that the resolution of DRIL has resulted in better visual outcomes
- Q. What is the center involving DME and non-center involving DME based on OCT?
- Center Involving DME: Diabetic Macular Edema (DME) that involves the central subfield zone (1 mm in diameter) as seen on OCT. This type of DME is associated with worse baseline and final visual acuity and is characterized by focal leakage from microaneurysms or capillaries. It is also associated with a lower rate of complete resolution of DME, with 40% of eyes still showing persistent DME after two years of treatment.
- Non-Center Involving DME: Diabetic Macular Edema (DME) that does not involve the central subfield zone (1 mm in diameter) as seen on OCT. This type of DME is associated with disorganization of the retinal inner layers (DRIL), external limiting membrane (ELM) and ellipsoid zone (EZ) disruption, and vitreomacular interface abnormalities (VMIA)
- Q. What is DRIL?
- DRIL stands for Disorganization of the Retinal Inner Layers. It is an OCT biomarker for DME and is identified on OCT when there is disruption of the demarcating interface lines between the ganglion cell-inner plexiform complex (GCL-IPL), inner nuclear layer (INL), outer plexiform layer (OPL), and outer nuclear layer (ONL).
- Eyes with DRIL have a worse baseline and final visual acuity despite anti-Vascular Endothelial Growth Factor (VEGF) injections and have almost eight times greater risk for poor visual recovery.

- Q. What is the role of Fluorescein angiography in Diabetic macular edema ?
- Fluorescein angiography is a diagnostic imaging technique used to assess the blood vessels in the retina.
- It can be used to detect and diagnose diabetic macular edema by identifying areas of leakage and abnormal blood vessel growth.
- It can also be used to monitor the progression of the disease and the effectiveness of treatments.
- it is mainly used at present to guide laser therapy
- Its application is gradually reducing with the advent of the use of OCT
- Q. Tell me more about Fluorescein angiography.
- Fluorescein angiography is a diagnostic imaging technique used to detect and monitor diabetic retinopathy.
- It involves injecting a fluorescent dye into the bloodstream, which is then absorbed by the retinal blood vessels.
- The dye is then illuminated with a special light source, allowing the blood vessels to be visualized and any abnormalities to be identified.
- This technique can be used to detect early signs of diabetic retinopathy, such as microaneurysms, and to monitor the progression of the disease.

- Management of Diabetic macular edema
- Q. What is the first line therapy for Diabetic macular edema ?
- Anti-VEGF agents are the first line therapy for Diabetic macular edema
- Q. Which are the various anti-VEGF agents used in Diabetic macular edema ?
- The various anti-VEGF agents used in Diabetic macular edema include bevacizumab, ranibizumab, and the Port Delivery System with Ranibizumab.
- Q. What is the DRCR retina network algorithm for Anti-VEGF therapy in DME?
- The DRCR Retina Network anti-VEGF treatment algorithm recommends six monthly injections, unless the visual acuity is 20/20 or better and the central subfield thickness is <320μm for men or <305μm for women on the Heidelberg Spectralis, in which case treatment may be withheld starting the fourth month.
- If there is evidence of stability over the previous two or more visits, further treatment may be withheld.
- Q. What is the advantage of Aflibercept over other anti-VEGF agents?
- The advantage of Aflibercept over other anti-VEGF agents is that it has a longer half-life, which may require less frequent treatments. Additionally, it has been shown to result in a 9-13 letter gain in BCVA compared with a 1.3 letter loss of BCVA in eyes treated with laser
- Q. What is the role of intravitreal steroids DME?
- The role of intravitreal steroids in DME is to improve vision and decrease retinal thickness, as there is an inflammatory component to DME. Steroids have powerful anti-edematous and anti-inflammatory effects as they decrease several pro-inflammatory mediators (IL-6, IL-8, TNF-α, MCP-1, ICAM-1, VEGF, etc.). However, long-term results have not shown the maintenance of these effects.
- Q. What is the role of laser photocoagulation in DME?
- Laser photocoagulation is a treatment option for diabetic macular edema (DME). It is used to reduce the amount of fluid in the macula, which can help improve vision.
- Laser photocoagulation can be used as a primary treatment for DME or as an adjunct to anti-VEGF therapy.
- It is most effective when used in combination with anti-VEGF therapy, as it can help reduce the number of injections needed.
- Laser photocoagulation can also be used to treat persistent DME that does not respond to anti-VEGF therapy.
- Q. What kind of laser is used for Focal and diffuse CSME?
- Focal laser and grid laser are used as an adjuvant for Focal and diffuse CSME respectively
- Q. What is the role of surgery for DME?
- Surgery is not typically recommended as a first-line treatment for diabetic macular edema (DME).
- However, in cases where medical therapy and pharmacotherapy have not been successful in resolving the DME, vitrectomy surgery may be considered.
- Vitrectomy surgery involves removing the vitreous gel from the eye and peeling away the epiretinal membrane, which can help to reduce macular edema and improve vision.