-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Introduction
-
Q. How many islet cells are present in the endocrine pancreas ?
- 3 million
-
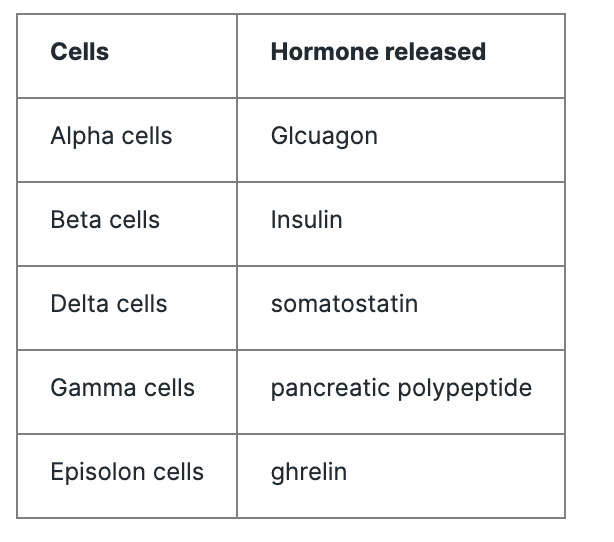
Q. What are the different types of cells present in the endocrine pancreas ?
-
Q. Of these cells, which cell is the most abundunt ?
- Beta-cells
- They compose 60% of the islet cells
-
Q. What are the difference between smaller islets and larger islets of pancreas ?
- Smaller islets have more propotion of Beta-cells
- they are closer to blood vessals
- the release more insulin
-
Q. How do beta-cells regenerate in the pancreas following extreme Beta-cells loss ?
-
- Neogenesis from Ductal cells
-
- Transdifferentiation from Alpha cell and delta cells
-
- Replication of beta-cells
-
-
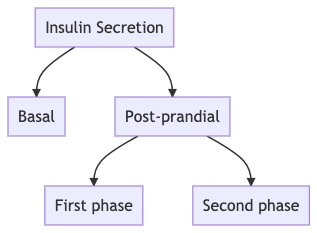
Q. What are the forms in which the insulin is released in the human body?
- Basal insulin secretion
- Transcription factors play a role in the release of basal insulin
- They are
- HNF 4alpha
- HNF1 alpha
- IPF1
- HNF 1 beta
- NeuroD1
- Nutrient mediated insulin release
- See below
- Basal insulin secretion
-
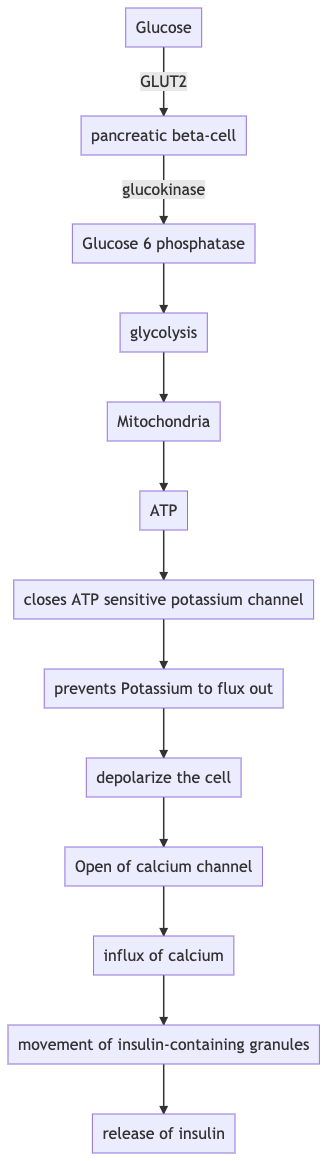
Q. Explain the process of nutrient mediated insulin released from the pancreatic beta-cells ?
- -
- Closure/inhibition of K+ Channel releases insulin ….
- If it remains open → neonatal diabetes
- If it remains closed → hypoglycemia
-
Q. Can you tell us more about the biology of the ATP-sensitive potassium channels present on the beta-cells of the pancreas?
- The SUR1-Kir6.2 pair constitutes the ATP sensitive pottasium channel
- The SUR1 respond to Sulphonylurea
- The SUR1 is encoded by the ABCC8 gene
- Closing of the ATP sensitive pottasium channel helps in the release of insulin
- If the channel remains closed as in Loss of function mutation, it can produce hypoglycemia- as it occurs in Persistent hyperinsulinemic hypoglycemia of infancy
- If the channel remains open (as it occurs in Gain-of-function mutation), it produces diabetes mellitus. This occurs in Neonatal diabetes mellitus
-
Q. What is the role cyclic-AMP second messenger in the release of insulin from beta-cells ?
- cAMP acts as an "amplifier" for insulin release
- the action of cAMP is independent of the ATP sensitive pottasium channel, however it is still glucose dependent system
- The GLP-1 and GIP (The incretin ) act via the cAMP pathway
-
Q. Are there any glucose sensors present in the pancreatic beta-cells which are indepdent of the glucose metabolism ?
- Yes. Other glucose sensors indepdent of glucose metabolism have been seen observed in rodent models. Two of them undergoing investigations currently are
- Sweet taste receptors
- Calcium sensory receptors
- Yes. Other glucose sensors indepdent of glucose metabolism have been seen observed in rodent models. Two of them undergoing investigations currently are
-
Q. What is the importance of the sweet taste receptors ?
- Interestingly, sweet taste receptors are present on the pancreatic beta-cells of the human islets
- Though their role in human islets is still under investigations, in rodent models they have been found to release insulin independent of the glucose metabolism.
- Studies does in Wistar rats have shown that the "sweet taste" stimulates the release of insulin early on. This is also called the " Cephalic phase insulin release ".
- As discussed above, their role in human beings is yet to be studied, but is is an interesting area of research.
-
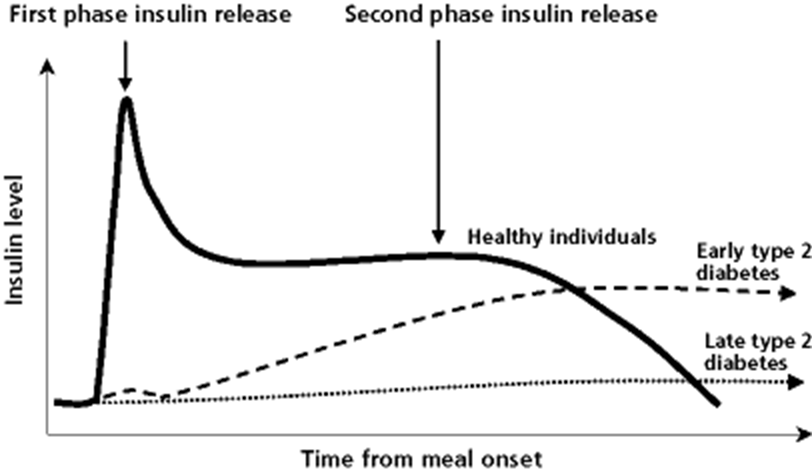
Q. What is the first phase and second-phase insulin secretion?
- Acute glycemia after a meal leads to immediate burst release of preformed insulin → this is the first phase of insulin secretion
- This is followed by slow and sustained release of insulin- 2nd phase insulin secretion which lasts for 1-2 hours
-
Q. In what time frame is 1st phase of insulin released?
- 1st phase insulin in response to glucose occurs within 3-5 min and subsides in 10 min
-
Q. What is the periodicity of basal insulin secretion?
- Insulin bursts are released every 11-14 min
- Loss of pulsatility of basal insulin secretion is the first thing that is lost in the case of type 1 diabetes
-
Q. What is the earliest change in insulin secretion seen in type 2 diabetes?
- Loss of 1st phase insulin secretion
- #Clinicalpearl
- Loss of pulsatility of basal insulin is 1st defect in type 1 diabetes
- Loss of 1st phase of insulin secretion is the first defect in type 2 diabetes
-
-
Neural regulation of the Beta-cells function
-
Q. Which region of the brain is involved in the neural regulation of the beta-cell function?
- The Hypothalamus
-
Q. What is the impact of the autnomomic nervous system in the beta-cell function ?
- The sympathetic system via alpha-2 receptor blocks the release of insulin and enhances glucagon release
- The parasympathetic system vias the M3 muscarinic receptor enhances the release of insulin and suppressed glucagon release
-
-
** Beta-cells mass**
-
Q. What is the beta-cell mass ?
- Beta-cell mass is the net amount of beta-cell
- the net mass be reduced by some factors and increased by some factors
-
Q. What factors reduce the beta-cell mass?
- Beta-cell apoptosis
- Dedifferentiation to alpha and other cells
-
Q. What factors increase the beta-cell mass ?
-
- Neogenesis from Ductal cells
-
- Transdifferentiation from Alpha cell and delta cells
-
- Replication of beta-cells
-
-
Q. What is the average life span of beta-cells ?
- 25 years
-
Q. What are "virgin" beta-cells ?
- In the peripheral of the islet there is a pool of immature or virgin beta-cell which can transdifferentiate into either alpha or beta-cell depending on the microenvironment
- this can be a potential lifelong reservoir of beta-cells
-
-
** Beta-cells insulin content**
-
Q.How much of an insulin reservoir does the pancreas have at any given point of time ?
- In normal healthy lean individuals, the pancreas has a reserved of 200-250 units of insulin at any given time which is enough to last for about 10 days
-
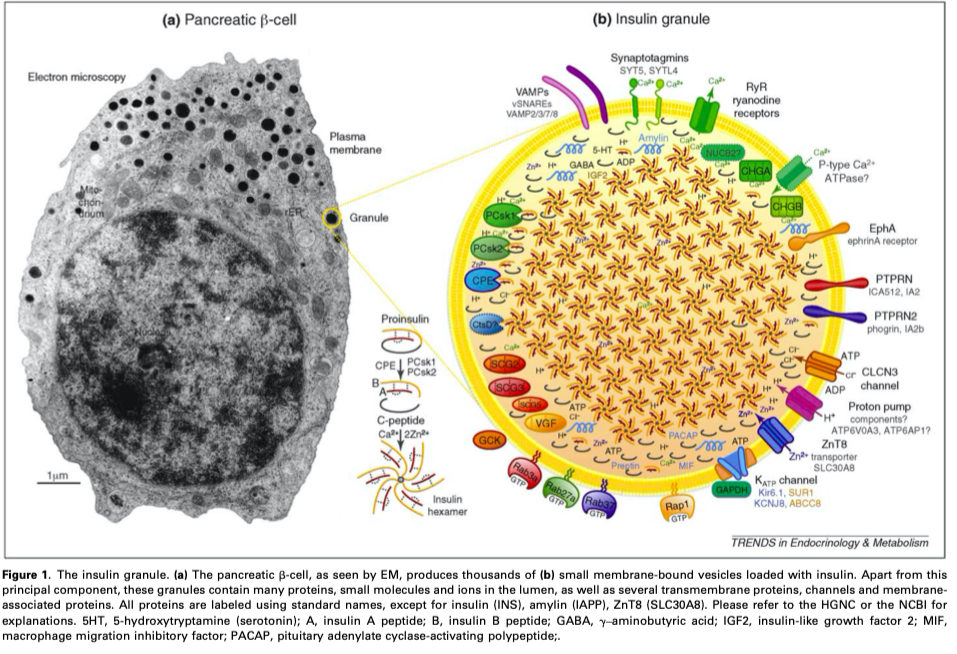
Q. Where is the insulin stored within the beta-cells ?
- Insulin is stored within anout 5000 secretory granuales present in the beta-cells of the pancreas
-
Q. Can you tell us about the basic structure of an insulin granule ?
- The insulin granule has a a elctron dense core which contains insulin packed in hexamers
- On the outside there is one calcium and two zinc ions which stabilize this core
- Ref: The insulin secretory granule as a signaling hub
-
Q. What percentage of granule insulin is secreated in response to glucose ?
- Only a small fracture of granule insulin (<1%) is secreated in response to glucose stimulation
-
Q. What is the half life of an insulin granule ?
- It is just about 5 days
-
Q. What is the difference between younger and older granules ?
- Younger granules are more mobile than the older granules
-
-
**Measures of insulin secretion and beta-cell mass **
-
Q. What are the various methods for measuring insulin secretion?
- OGTT and IVGTT
- Measuring insulin levels
- Arginine induced glucose secretion
-
Q. Which of these tests correlate best with beta-cell mass?
- Insulin response to glucose and arginine correlate best with beta-cell mass
-
Q. Which nuclear imaging technique is being developed to assess beta-cell mass?
- PET Scan
-
Q. How much beta cell mass is lost before fasting blood glucose starts to rise?
- 60-70% of the beta-cell mass is lost
-
Q. Is insulin measurement of a good test for the assessment of beta-cell mass?
- No
- Because insulin resistance greatly determines insulin level and hence fasting insulin level is not a great test for beta-cell mass
-
Q. What is AIRgluc?
- It is an acute insulin response to glucose
- It is a good test for the assessment of beta-cell mass
- IV glucose is given and the amount of rising of insulin in 10 min is measured
- This measures the first phase insulin response
- People at risk of type 2 / type 1 diabetes have less insulin secretion in 1st 10 min (loss of 1st phase insulin response) compared to normal people
-
Q. What is a hallmark in response to various stimuli in type 2 diabetes?
- In type 2 diabetes – 1st phase insulin response to glucose is lost but the response to arginine or isoproterenol is maintained
- This is the hallmark of type 2 diabetes
-
Insulin secreation verus plasma insulin
-
Q. What is insulin predominantly secreated ?
- Insulin is predominantly released into the portal circulation
-
Q. What is C-peptide ?
- The pancreatic proinsulin is broken down into insulin and C-peptide
- the C-peptide is released in equimolar concentration as insulin
-
Q. Why is C-peptide a better measure of insulin secreation ?
- This is because of the following reasons:
- a) The amount of C-peptide that is released is equal to the amount of insulin release
- b) C-peptide is NOT extracted by the liver whereas majority of endogeous insulin is extracted by the liver (rememeber insulin is released into the portal circulation)
- c) C-peptide clearance accours via kidney - but this is constant. That means at any given point of time, the amount cleared by kidney is constant to the amount which is being produced
- d) Exogenous insulin does not impact the measured of c-peptide hence c-peptide is a measure of endogenous insulin production
- This is because of the following reasons:
-
Q. Can you calculate the exact amount of insulin being secreated by measuring the C-peptide levels ?
- Yes.
- Using a mathematical process can Deconvolution you can measure the an approximate amount of insulin which is secreated by measuring the C-peptide
-
Q. What is Deconvolution ?
- This is an algorithm based process in which the recorded data can be reversed engineered to find the original signal
- This is based on the theory that the recorded data or signal is the the original signal which is then filtered
- So basically by measuring the C-peptide you can trace it back to its root and find the amount of insulin which is secreated
-
Q. Does the C-peptide measured in the urine correlate with the insulin secreation ?
- Yes
- Urine c-peptide to creatinine ratio (UCPCR) give a good estimate of beta-cell reserve in patients with Type 1 Diabetes
- It is typically measured 2 hours after a meal
- Sample is collected using boric acid as preservative
- UCPCR value <0.2 nmol/mmol is strongly suggestive of absolute insulin deficiency as seen in long-standing Type 1 Diabetes
-
Characteristics of Insulin secreation in Vivo
-
Q. Under normal physiological conditions which is more stable insulin sensitivity or insulin secretion?
- Insulin sensitivity is relatively stable in normal physiological conditions. The insulin sensitivity only varies by 30 to 80% throughout the 24 hour period. In a pharmacological way we can improve the insulin sensitivity only by as much as 2 times the baseline.
- Insulin secretion on the other hand can vary throughout the day and can vary based on the meal which is taken. You can improve insulin secretion by manyfold in the same individual.
-
Q. As a gross figure how much insulin is required to dispose of 75 g of glucose in a lean individual vis-a-vis a obese individual ?
- According to William's textbook of endocrinology 0.5 units of insulin is required to dispose of 75 g of glucose in an insulin-sensitive lean individual.
- In an obese insulin resistant individual this figure is as high as 45 units.
-
Q. What is an ' insulinogenic index ' ?
- Insulinogenic index is the simplest marker of First phase insulin secreation
- It is calculated using an OGTT
- It is the ratio of the change of insulin secreation in 30 minutes from baseline to post glucose load divided by the change in glucose value during this period
- IGI = δinsulin (0-30 min)/δglucose (0-30 min)
- (Insulin is measured in microunits per millilitre, whereas glucose is measured in milligrams per decilitre)
- IGI = δinsulin (0-30 min)/δglucose (0-30 min)
-
-
-
Modes of Beta-cell response
-
Q. Give an outline of insulin secreation in the human body ?
-
Q. What are the three main modes of Beta-cell response (insulin secretory response) ?
- 1) First phase insulin secreation
- 2) Beta-cell glucose sensitivity
- 3) Potentiation of insulin secretion -
Q. What is First phase insulin secreation ?
- Insulin release occurs in two ways
- a) Basal- continuous insulin that is released from the beta-cell irrespective to the food or glucose intake
- b) Post-meal insulin release
- In the post-meal insulin release- there is an acute response to glucose upsurge that occurs within 2 minutes of glucose excursion which is called the first-phase insulin secreation
- This is a burst of insulin secreation that occurs from preformed and mature insulin secretory granules
- This is a form of pre-emptive method of preventing a glucose surge. This first phases suppresses hepatic glucose production and enhances the peripheral glucose utilization
- The First phase insulin secreation can be assesed by
- a) Hyperglycemic clamp
- b) Intravenous glucose tolerance test IVGTT -
Q. What is second phase insulin secretion ?
- It is the slow and sustained release of insulin post the glucose load
- This is derived mainly from the reserve pool of insulin granules
-
- First phase insulin- from readily releasable pool (RRP)
- Second phase insulin- from reserve pool
- Q. In terms of new theory, how do we sub-divide the RRP in three parts ?
-
"Old Face"- these are predocked granules ready to be released. They are already docked and released as soon as the signal arrives.
-
"The restless newcomer"- they are newly recruited on stimulation and are fuse almost immediately to the plasma membrane
-
"The resting newcomer"- they are recruited on stimulation but are first docked (rested) and then they fuse to the plasma membrane and released
-
All the three contribute the the first phase insulin secretion
-
Q. What is Beta-cell glucose sensitivity ?
- As discussed earlier, the Beta-cells sense the glucose excusrsion and release insulin in response to the same
- In that regards, beta-cell is both a sensor of glucose and a producer of insulin
- Beta-cell glucose sensitivity is the measure of the ability of the beta-cell to sense the glucose
- There is a school of thought that the Beta-cell glucose sensitivity is one of the early defects that occur in patients with Type 2 Diabetes
- ie if the glucose cannot be sensed properly, how will insulin be released in reponse to the same
- Naturally, the First phase insulin secreation is affected by the same.-
Q. What is potentiation of insulin secreation ?
- In a normal beta-cell the insulin secreation is potentiated in accordance to the glucose levels
- other factors like incretins, fructose, Sulphonylurea etc may also help in the potentiation- Q. Apart from glucose what are the other nutrient factors that impact insulin release ?
- Some amino-acids like Arginine and Free Fatty acid also potentiate insulin release apart from the glucose
- Q. Apart from glucose what are the other nutrient factors that impact insulin release ?
-
Insulin secreation in a fasting state
-
Q. Is basal insulin secreted in a pulsatile manner ?
- Yes
- Basal insulin is secreted in short bursts of 5-14 minutes
- Over a period of 24 hours there are also 80-180 minute ultradian cycles
-
Q. What happens to the pulsatile secretion in a hyperglycemic state ?
- The pulsatile secretion is disrupted in a hyperglycemic state
-
Q. What is the importance of Prolinsulin to insulin ratio ?
- The higher proinsulin to insulin or proinsulin to c-peptide ratio is a marker of beta-cell dysfunction and risk of diabetes mellitus
-
-
Insulin secretory response to intravenous glucose
-
Q. What is the Hyperglycemic clamp ?
- This is a study done for assessing the first phase and second phase insulin response
- Here the person is given an acute burst of glucose
- Initially there is a sharp increase in the glucose secreation. This is the First phase insulin secreation
- Then there is a small dip in insulin release
- This is followed by a slow and sustained release of insulin again- which is the second phase insulin secreation
-
Q. What is the typical magnitude of First phase insulin secreation ?
- In a normal individual for a glucose upsurge of >126 mg/dl , the first phase insulin secreation (also called Acute insulin response) is typically 4 nmol/m2 of body surface area.
- This is approximately 1 unit in a 70 kg man.
- This is about 10% of the total insulin release in the second phase
-
Q. Is it true the loss of first phase insulin secreation is the earliest marker of Beta-cell dysfunction ?
- Yes.
- That is correct
-
There is another school of thought which is a below
- "Insulin is released from the pancreas in a biphasic manner in response to a square-wave increase in arterial glucose concentration. The first phase consists of a brief spike lasting ∼10 min followed by the second phase, which reaches a plateau at 2–3 h. It is widely thought that diminution of first-phase insulin release is the earliest detectable defect of β-cell function in individuals destined to develop type 2 diabetes and that this defect largely represents β-cell exhaustion after years of compensation for antecedent insulin resistance. In this article, the origins of these concepts are reviewed and recent evidence ^^is presented suggesting that reductions in both phases of insulin release are equally early, that they precede insulin resistance other than that simply due to obesity, and that they therefore may represent the primary genetic risk factor predisposing individuals to type 2 diabetes^^"
-
-
** Intravenous glucose tolerance test IVGTT **
- Q. What is IVGTT ?
- This is another method for assessment of First phase insulin secreation
- Here the glucose is infused IV and the insulin and c-peptide are measured at regular intervals
- Here the First phase insulin secreation is similar to Hyperglycemic clamp but the subsequent response (second phase) is different because of the different methodology
- Q. What is IVGTT ?
-
Graded glucose infusion test
- Q. What is Graded glucose infusion test ?
- This is a test for dose response relationship between insulin secreation and glucose infusion
- ProSciento literature states the procedure as follows:
- "After an overnight fast a basal (control) period is followed by sequential incremental intravenous infusions of glucose calculated to raise the blood glucose concentration from fasting levels to the hyperglycemic range (approximately 300mg/dL,17 mmol/L).
- A graded infusion of 20% glucose is administered at 2, 4, 6, 8, and 12 mg/kg/min each for 30 minutes. Blood samples are drawn at 10, 20, and 30 minutes during each 30-minute period for measurement of glucose, insulin,and plasma C-peptide
- This is used in research labs to generate pre-clinical data on effectiveness of novel therapies in diabetes
- Q. What is Graded glucose infusion test ?
-
Slow beta-cell response modes and adaptation mechanisms
- Q. In an individual with a good beta-cell reserve, does a mild chronic hyperglycemia, sustain the insulin secreation ?
- Yes.
- Graded glucose infusion tests have shown that in subjects with good beta-cell reserved, a chronic mild hyperglycemia can potentiate the insulin secreation and the body can maintain homeostasis.
- Q. In an individual with a good beta-cell reserve, does a mild chronic hyperglycemia, sustain the insulin secreation ?
-
**Regulation of insulin secretion **
-
Q. Summarize the various factors that regular insulin secretion?
- Nutrients that enhance insulin release
- Glucose
- Fatty acid
- Amino acids
- Nutrients that enhance insulin release
-
Intra-islet hormones
- Glucagon – increases insulin
- Somatostatin – reduces insulin
-
Neurotransmitter
- Acetylcholine- increase insulin
- Catecholamine
- Via alpha2- reduce insulin
- Via beta 2 – increases insulin
-
Gut hormones
- Increase insulin
- GLP1
- GIP
- VIP
- Secretin
- Reduce insulin
- Ghrelin
- Increase insulin
-
Adipokine
- Increase insulin
- adiponectin
- Reduce insulin
- Leptin
- Resistin
- Increase insulin
-
Other hormones
- Increase insulin
- Vitamin D
- Estrogen
- Reduce insulin
- IGF1
- Thyroid hormone
- Increase insulin
-
Glucocorticoids have dual-action
- directly reduce insulin but produce hyperglycemia which increases insulin
-
Drugs
- SU and GLL1 analog- increase insulin
- Diazoxide – reduce insulin
-
Q. How do non-nutrient factors regulate insulin secretion?
- Via cAMP – eg: glucagon, GLP1
- Via Phospholipase C – CCK, Acetylcholine
-
Metabolic control of insulin secretion
-
Q. What is the primary regulator of insulin secretion?
- Glucose!
-
Q. Apart from glucose, which other nutrients can potentially release insulin?
- Amino acids
- Fatty acids
-
Q. Which amino acids enhance insulin secretion?
- Glutamine + leucine
- Arginine
-
Q. What is the action of free fatty acid on insulin secretion?
- Free fatty acid enhances Glucose stimulated insulin secreation
- This probably compensates for the increased insulin resistance produced by free fatty acids in initial stages
-
Q. Which are two pools of insulin stored in secretory granules?
- Readily releasable pool – RRP – 1% - responsible for the 1st phase insulin release
- Reserve pool - 99% - needs to undergo preparatory steps to be released
-
**Hormonal regulation of insulin secretion **
-
Q. What is the effect of estradiol on insulin secretion?
- Estradiol enhances insulin secretion
- ER receptors are present on the pancreatic islets
-
Q. What is the effect of melatonin on insulin secretion?
- Newer studies have shown that melatonin inhibits insulin secretion
-
Q. Which important gut hormone increases insulin secretion?
- GLP1
-
Q. Which other gut hormones increase insulin secretion?
- CCK
- VIP
- Gastrin
- GIP
- Secretin
-
Q. What is the effect of leptin on insulin secretion?
- Leptin inhibits insulin secretion
-
Q. What is the effect of IGF1 on insulin secretion?
- IGF1 reduces insulin secretion
-
Q What is the effect of thyroid hormone on insulin secretion?
- It mildly reduces insulin secretion
-
Q What is the effect of vitamin D on insulin secretion?
- It enhances insulin secretion
-
Q. What is the effect of glucocorticoid on insulin secretion?
- Direct effect – inhibit insulin secretion
- Indirect effect – increase insulin secretion by producing hyperglycemia and insulin resistance
-
Q. What is the effect of catecholamines?
- They inhibit insulin secretion by acting via alpha 2 receptors
- However, beta 2 receptors - it enhances insulin secretion
-
Q. What about somatostatin?
- It inhibits insulin secretion
-
Q. What about glucagon?
- Increases insulin secretion
-
**Pharmacological control of insulin secretion **
-
Q. Summarize the impact of various drugs influencing insulin secretion?
- Potassium channel blockers- SU and Meglitanitdes increases insulin secretion
- Potassium channel openers- Diazoxide reduce insulin secretion
- Calcium channel blockers- reduces insulin secretion , however in vivo has little effect
- GLP1 analog- enhance insulin secretion
-
-
- Source: Talk on "Assessment of Insulin Secretion and Sensitivity"
- Date: Monday, 10 May 2021
Please consider donating to "Notes in Endocrinology" to keep us going. Please visit our DONATION page to know more