- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
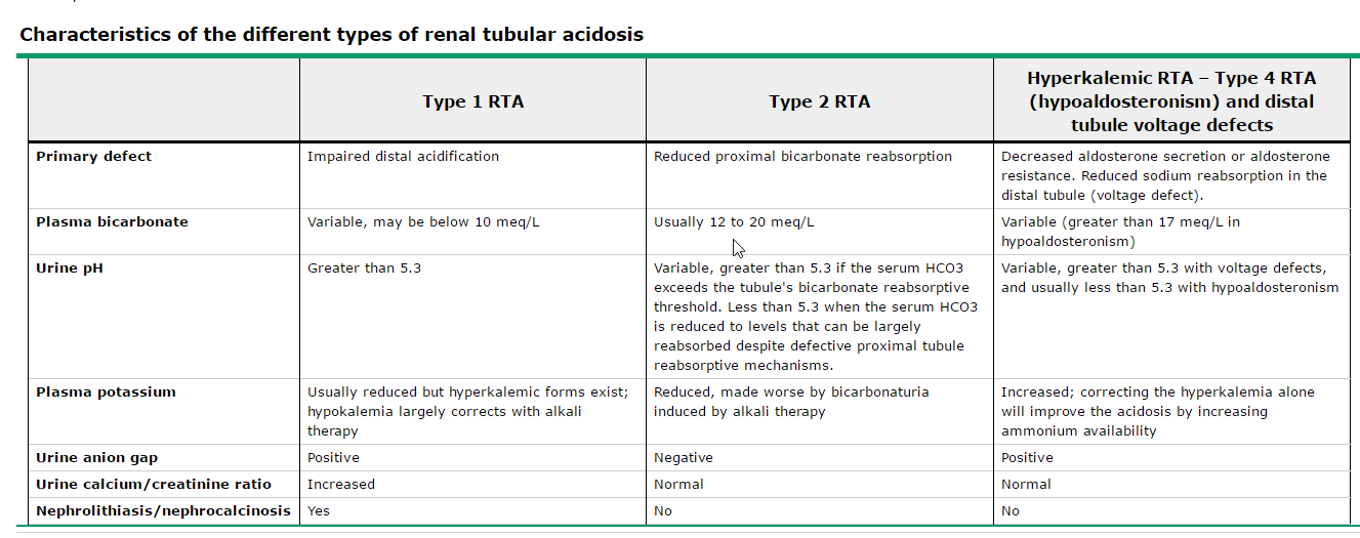
- Q. Summarize the various forms of RTA?
- Etiology and diagnosis
- Q. What is distal and what is proximal RTA?
- Distal RTA: failure to excrete hydrogen ion distally.
- Proximal RTA: failure to reabsorb bicarbonate at the PCT.
- Q. Name some common causes of Distal RTA?
- Idiopathic:
- Familial – Autosomal dominant or Autosomal recessive
- Drugs:
- Amphotericin B, Ibuprofen.
- Autoimmune disease: SLE, Sjogren’s.
- Conditions producing hypercalciuria: idiopathic hypercalciuria, PHPT, vitamin D toxicity.
- Wilson’s disease.
- Medullary sponge kidney.
- Idiopathic:
- Q. What are common causes of Proximal RTA?
- Familial: CA2 deficiency is one of the familial causes.
- Drugs: Carbonic anhydrase inhibitor, Topiramate.
- Multiple myeloma.
- Other congenital causes: Wilson’s disease, GSD type 1, hereditary fructose intolerance.
- Q. How does pH help in differentiating the two conditions?
- pH >5.5 in distal RTA.
- pH is variable in proximal RTA, depending on the bicarbonate load. If high, then pH is high; if low, then pH is low.
- Q. What are two classical lab features of RTA?
- Normal anion gap metabolic acidosis.
- Hypokalemia.
- Q. Which is an important test to distinguish distal RTA from other causes of normal anion gap metabolic acidosis?
- Urinary ammonium excretion.
- This is reduced in the case of distal RTA and is a classical feature.
- However, urinary ammonium excretion cannot be estimated directly by most labs.
- Hence, urinary anion gap is a useful substitute.
- Q. How is urine anion gap estimated?
- Urine anion gap = urinary (Na + K – Cl).
- Q. What is the normal urine anion gap?
- Normal UAG is POSITIVE.
- Urine anion gap is a marker of NH4 excretion in urine.
- NH4 is excreted as NH4Cl, hence higher excretion means more Cl released, leading to a more NEGATIVE UAG.
- Hence Negative UAG = Increased NH4 excretion.
- Q. How is UAG helpful in the diagnosis of distal RTA?
- UAG is positive in a healthy individual.
- UAG is positive in Distal RTA (reduced NH4 excretion).
- UAG is negative in other causes of metabolic acidosis, indicating increased NH4 excretion.
- Q. What is an alternative test to urine anion gap?
- Urine osmolal gap.
- Q. How is urine osmolal gap calculated?
- UOG = Measured UO – Calculated UO.
- Calculation of UO:
- Calculated urine osmolality (mosmol/kg) = (2 x [Na + K]) + [urea nitrogen in mg/dL]/2.8 + [glucose in mg/dL]/18.
- Q. What is the interpretation of UOG in acidosis?
- UOG is a direct estimate of NH4.
- UOG >200 mosm/kg in metabolic acidosis indicates other causes of metabolic acidosis.
- UOG <100 mosm/kg indicates Distal RTA.
- Pearl:
- UAG – Positive in distal RTA.
- UOG – Reduced <100 mosm/kg in distal RTA.
- Urine ammonium excretion – reduced in distal RTA.
- Pathophysiology
- Q. What is the difference in hypokalemia between proximal and distal RTA?
- Hypokalemia improves with alkali therapy in distal RTA.
- It worsens with alkali therapy in proximal RTA.
- Clinical features
- Q. At what age does Distal RTA present?
- Distal Renal Tubular Acidosis (RTA) can present at any age.
- However, the onset of distal RTA varies based on the cause.
- In adults, new-onset distal RTA is often associated with autoimmune diseases such as Sjögren's syndrome and rheumatoid arthritis, or hypercalciuria.
- Distal RTA may be the presenting manifestation of autoimmune diseases such as Sjögren's syndrome.
- Hereditary distal RTA, caused by genetic mutations, is most commonly diagnosed in children.
- Mutations in genes such as SLC4A1, ATP6V0A4, ATP6V1B1, ATP6V1C2, and FOXI1 have been identified as major causes of hereditary distal RTA.
- Q. What are the clinical features of distal RTA in children?
- Clinical features are mainly due to underlying disease.
- AR forms of familial RTA are more severe.
- Recessive form associated with:
- Severe hyperchloremic metabolic acidosis (serum bicarbonate levels may decrease below 10 mEq/L).
- Moderate to severe hypokalemia (serum potassium ≤ 3.0 mEq/L).
- Nephrocalcinosis.
- Vomiting.
- Dehydration.
- Poor growth.
- Rickets.
- Bilateral SNHL in some cases with mutations of the gene that encodes B1 subunit of the H-ATPase pump.
- Q. What are the clinical features of proximal RTA in children?
- Growth failure.
- Metabolic bone disease: rickets, osteomalacia.
- Proximal muscle weakness due to hypokalemia.
- Constipation.
- Hypovolemia.
- Q. Which RTA has an increased risk of stone formation and why?
- Distal RTA.
- This is because:
- Increased urinary calcium excretion.
- Alkaline pH of urine.
- Hypocitraturia.
- RTA due to carbonic anhydrase inhibitor also produces stones.
- Other proximal RTA does not increase the risk of stones.
- Distal RTA.
- Treatment
- Q. What is the treatment of distal RTA?
- Bicarbonate replacement:
- Adults: 1-2 meq/kg/day.
- Children: 4-8 meq/kg/day.
- Bicarbonate given as:
- Sodium citrate.
- Sodium bicarbonate.
- Potassium citrate (preferred in case of hypokalemia).
- Bicarbonate replacement:
- Q. What is the aim of treatment of distal RTA?
- Normalization of serum bicarbonate (22-24 meq/l).
- Q. What is the treatment of proximal RTA?
- It requires correction of acidemia and hypophosphatemia.
- Giving bicarbonate to these patients may worsen hypokalemia, hence give only Potassium citrate.
- Dose is 10-15 meq/kg/day.
- If high-dose alkali is not tolerated, give thiazide diuretic, which produces mild volume depletion, resulting in more sodium reabsorption with passive bicarbonate reabsorption in proximal tubules.
- Q. Can patients with distal RTA have hypophosphatemia?
- Yes, patients with distal Renal Tubular Acidosis (RTA) can have hypophosphatemia.
- Hypophosphatemia in distal RTA can occur due to increased urinary phosphate excretion.
- This is often secondary to the metabolic acidosis that is characteristic of distal RTA.
- The acidosis can lead to increased bone resorption, releasing calcium and phosphate into the bloodstream.
- The kidneys respond by increasing urinary excretion of both calcium and phosphate, which can lead to hypophosphatemia.
- However, hypophosphatemia is not a universal finding in distal RTA, and its presence can be influenced by other factors such as dietary phosphate intake and the presence of other medical conditions.
- Q. Can distal RTA present acutely?
- Distal Renal Tubular Acidosis (RTA) typically presents as a chronic condition, but acute presentations can occur.
- Acute presentations are often triggered by an underlying illness or the initiation of a medication that impairs the kidney's ability to excrete acid.
- Symptoms of an acute presentation can include severe metabolic acidosis, hypokalemia, and various systemic symptoms such as fatigue, muscle weakness, and nausea.
- In children, an acute presentation may also include poor growth, vomiting, dehydration, and rickets.
- Regardless of the timing of presentation, the management of distal RTA involves correcting the acid-base imbalance, treating the underlying cause if identifiable, and managing any complications such as electrolyte imbalances or kidney stones.
- Q. How do you treat distal RTA?
- Treatment for distal (type 1) renal tubular acidosis (RTA) typically involves:
- Alkali therapy: This is the mainstay of treatment for distal RTA. It involves the administration of oral alkali supplements to correct the acidosis and replace urinary bicarbonate losses. Sodium bicarbonate or sodium citrate are commonly used.
- Potassium supplementation: Hypokalemia, a common feature of distal RTA, may require treatment with oral potassium supplements.
- Addressing underlying causes: If distal RTA is secondary to a specific cause such as an autoimmune disease or medication, addressing the underlying cause can help manage the condition.
- Regular monitoring: Patients with distal RTA require regular monitoring of their electrolyte levels and acid-base status to ensure the effectiveness of treatment and adjust as necessary.
- Management of complications: Chronic kidney disease is a potential complication of distal RTA. Regular monitoring of kidney function and appropriate management strategies are important.
- Genetic counseling: In cases where distal RTA is hereditary, genetic counseling may be beneficial for patients and their families.
- Treatment for distal (type 1) renal tubular acidosis (RTA) typically involves:
- Q. What is the dose of Sodium bicarbonate that we must use in distal RTA?
- The dose of sodium bicarbonate used in the treatment of distal RTA can vary based on the individual patient's needs.
- Typically, the goal of therapy is to maintain a serum bicarbonate level of at least 20 mEq/L.
- To achieve this, an initial dose of 1 to 2 mEq/kg/day of oral sodium bicarbonate or sodium citrate is often used.
- This dose is usually divided into multiple doses throughout the day to maintain a steady state of alkali in the body and prevent a sudden surge in pH.
- Q. What is the bicarbonate content in a 500 mg sodium bicarbonate tablet (e.g., Sobosis)?
- 1 mEq NaHCO3 is 84 mg. 1000 mg = 1 gram of NaHCO3 contains 11.9 mEq of sodium and bicarbonate ions.
- So, a 500 mg tablet has 5-6 mEq of sodium bicarbonate.
- Q. So, what dose of Sobosis would be required to treat a 70 kg adult with distal RTA?
- To determine the dose of Sobosis required to treat a 70 kg adult with distal RTA, we need to calculate the total daily dose needed to maintain a serum bicarbonate level of at least 20 mEq/L.
- Assuming an initial dose of 1 to 2 mEq/kg/day, the total daily dose for a 70 kg adult would be:
- 1 mEq/kg/day x 70 kg = 70 mEq/day
- 2 mEq/kg/day x 70 kg = 140 mEq/day
- So, the total daily dose of Sobosis required for this patient would be between 70 to 140 mEq/day, depending on the severity of their distal RTA.
- Using the bicarbonate content in a 500 mg Sobosis tablet (5-6 mEq), we can calculate the number of tablets required per day:
- 70 mEq/day ÷ 5 mEq/tablet = 14 tablets/day
- 140 mEq/day ÷ 6 mEq/tablet = 23.3 tablets/day (rounded up to 24 tablets/day)
- Therefore, a 70 kg adult with distal RTA would need to take between 14 to 24 tablets of Sobosis per day to maintain a serum bicarbonate level of at least 20 mEq/L.
- Q. Is a 1 gram tablet of Sobosis available?
- Yes, Sobosis forte is 1 gram.
- So, this would be around 7 tablets.