- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Join our WhatsApp channel to get regular updates from “Notes in Endocrinology” and “Endocrinology India”: https://whatsapp.com/channel/0029VaFyQnfHbFUz0LVdBO3****h
Support us:
- Support you by Becoming a YouTube member (Click here).
- Premium Membership- Download PDF version of Notes, Get ad free video and more
- Consultant Membership- Above plus Download Powerpoint presentation of the notes
- Support us by purchasing our book - Click here for more details:
-
Q. What is the definition of Osteoporosis?
- It is a disease characterized by
- Low bone mass
- Microarchitectural disruption
- Increase skeletal fragility
- Leading to an increase in fracture risk
- WHO defines it as T score <-2.5
- It is a disease characterized by
-
Q. Give the WHO diagnostic criteria for osteoporosis?
- Normal T score >-1.0
- Osteopenia – T score -1.0 to -2.5
- Osteoporosis – T score <-2.5
- Severe osteoporosis- T score < -2.5 + Fragility fracture
-
Q. What are the diagnostic criteria based on AACE 2020 guidelines ?
-
- T-score − 2.5 or below in the lumbar spine, femoral neck, total proximal femur, or 1/3 radius
-
- Low-trauma spine or hip fracture (regardless of bone mineral density)
-
- T-score between − 1.0 and − 2.5 and a fragility fracture of the proximal humerus, pelvis, or distal forearm
-
- T-score between − 1.0 and − 2.5 and high FRAX® (or if available, TBS-adjusted FRAX®) fracture probability based on country-specific thresholds
-
-
Q. What are T-score and Z-score?
- The T-score is the number of standard deviations of the BMD from the normal value of a young adult
- The Z-score represents the number of standard deviations of the BMD from the normal value of the age, sex, race/ethnicity matched control subjects
-
Q. When to use T-score and when to use Z-score?
- T-score is used for the standard diagnosis of osteoporosis in postmenopausal and elderly men
- Z-score is used to diagnose low bone mass or vulnerable bones in premenopausal women or young men.
-
Q. What Z score cutoff is used for diagnosis of osteoporosis in Young premenopausal women?
- If the Z score is < -2.0 the lady is said to have "low bone mass". Osteoporosis may not be a suitable term to use for premenopausal women, but a low bone mass term may be used as a substitute to "osteoporosis" and means the same diagnostically
- In premenopausal women - the search for the secondary cause is a must
-
Q. Is FRAX for India available ?
- Yes
- Please use the link https://www.sheffield.ac.uk/FRAX/tool.aspx?country=51
-
Q. What is the cut-off for treatment based on the FRAX score ?
- FRAX shows 10 years probability of fracture
- The indications for intervention are :
- 3% for hip fracture or
- ≥ 20% for major osteoporotic fracture
-
Q. If a patient has a fragility fracture, does she need a DEXA scan for the diagnosis of Osteoporosis ?
- No
- A fragility fracture is diagnostic of osteoporosis
- It does not need a DEXA scan to prove the diagnosis
-
Q. What is a fragility fracture ?
- "A fragility fracture is usually a fracture sustained from force similar to a fall from a standing position or less that would not have occurred in healthy bone, excepting fractures of the skull, face, fingers, and toes."
-
Q. What are the current screening guidelines for osteoporosis by NOF?
- All women >/= 65 years
- All men >/= 70 years
- All between ages 50-69 years with risk factors for osteoporosis
- Adults having fractures after 50 years
- Those with low bone mass and RA
- Those with low bone mass on Gc of dose predinisolone equivalents >/= 5 mg for >/= 3 months
-
Q. What is the mortality rate following a hip fracture in postmenopausal women?
- 2-year mortality rate in postmenopausal women following a hip fracture is 12-20%
-
Q. Enlist the risk factors for Osteoporosis?
- Advancing age
- Rheumatoid arthritis
- Current cigarette smoking
- Excessive alcohol consumption
- Glucocorticoid use
- Family history of hip fracture
- Rheumatoid arthritis
- Previous fragility fracture
- Other secondary causes
- Hypogonadism
- Early menopause
- Malabsorption
- IBD
- CLD
- Primary hyperparathyroidism
-
Q. What is the indication for lateral X-ray in the elderly?
- All men >80 years and women >70 years with BMD T score <-1.0
- All men 70-79 years and women 65-69 years with T score <-1.5
- Postmenopausal women and men >50 years with
- Historical height loss > 4cm (>1.5 inch)
- Prospective height loss >2 cm (0.8 inch)
- Low trauma fracture
- Recent or ongoing Glucocorticoid use
-
Q. What are the preferred screening tests?
- DEXA
-
Q. What are the sites for DEXA for screening?
- Hip and spine
- In the elderly Hip alone is enough
-
Q. Which hip should be measured, right or left?
- Ideally at baseline both hips should be measured
-
Q. Which specific sites are to be measured?
-
- Total Hip
-
- Femoral neck
-
- Lumbar spine L1-L4
-
-
Q. When is BMD repeated if the initial BMD does not show osteoporosis?
- Women > 65 years
- Initial BMD <-2.0 – 2.5 at any site or having a risk factor for ongoing bone loss- every 2 years
- Initial BMD <1.5 to -2.0 at any site – every 3-5 years
- Initial BMD <1.0- 1.5 with no other risk factor – every 10-15 years
-
Q. What are the arguments in favor of screening for osteoporosis?
- BMD has a definite link with fracture risk
- Treatment is available which can prevent fracture
- Knowledge of risk will help improve compliance with lifestyle and treatment
- It is a common disease with a high impact on morbidity and mortality
- Screening tests are easily available
-
Q. What are the arguments against screening?
- BMD is not the only criteria that define the risk of fracture
- If BMD Is normal- does it rule out the risk of fracture?
- Cost of screening
- Single measurement of BMD less important than serial measurements
-
Q. For what duration of glucocorticoid use, should DEXA be done?
- For post-menopausal women, if glucocorticoids are given for >3 months or anticipated to be given for >3 months, a DEXA must be done at baseline without fail
-
Osteoporotic fracture risk assessment
-
Q. What are the methods for assessment of osteoporosis fracture risk?
- FRAX
- BMD measurement
- Assessment of bone microarchitecture (beyond BMD)
-
Q. How is bone microarchitecture assessed?
- HR pQCT
- Tetracycline labeled transiliac bone biopsy
- Micro MRI
- High-resolution MRI
- Trabecular bone score – indirect marker
-
[[FRAX]]
-
Q. In FRAX, the Risk of fracture is expressed as absolute risk or relative risk?
- It is expressed as an absolute risk of fracture in the next 10 years
-
Q. FRAX is applicable for age group patients?
- Patients between the age of 40-90 years
-
Q. Which are the factors considered in FRAX?
- Age
- Sex
- BMI
- Parental fracture of the hip
- Previous fracture (A previous fracture denotes more accurately a previous fracture in adult life occurring spontaneously, or a fracture arising from trauma which, in a healthy individual, would not have resulted in a fracture. Enter yes or no (see also notes on risk factors)
- Current smoking
- Alcohol - >/= 3 units/day
- Rheumatoid arthritis
- Glucocorticoid use – Prednisolone >5 mg for >3 months
- Secondary osteoporosis
- Femoral neck BMD
-
Q. Which are factors included in secondary osteoporosis?
- Type 1 diabetes
- Hypogonadism
- Premature menopause
- PHPT
- CLD
- Malabsorption
- Malnutrition
- Uncontrolled hyperthyroidism
- Osteogenesis imperfecta
-
Q. What will the results give you?
- 10-year risk of
- Major osteoporotic fracture
- Hip fracture
- Each in percentage
- 10-year risk of
-
Q. Is FRAX for India available?
- Yes
- Please use the link https://www.sheffield.ac.uk/FRAX/tool.aspx?country=51
-
Q. What is the bias of basing treatment based on FRAX?
- Treatment based on FRAX will treat more older patients with higher T scores compared to younger patients with the lower T scores
-
Q. What are the limitations of FRAX?
- Limited to 4 ethnicities
- Only takes into account Hip BMD and not lumbar or other BMD
- Other cases it may underestimate the risk (see below)
- All regions data not available
-
Q. FRAX is used for which ethnicities?
- Black
- Hispanic
- Asian
- Caucasian
-
Q. In which patients do FRAX underestimate the fracture risk?
- Type 2 diabetics
- Multiple fractures
- Family history of non-hip fracture
- High dose Gc >7.5 mg
- Severe vertebral fractures
- Low Lumbar BMD with normal hip BMD
-
Q. Overall does FRAX underestimate or overestimate fracture risk?
- Overall, FRAX underestimates future fracture risk
- Also fall events and the risk of falls are not directly captured by FRAX
-
Q. Which other fracture risk calculator also takes risk of fall into account?
- Garvan Fracture risk calculator
-
Measurement of BMD
-
Q. What are the methods for measurement of BMD?
- DEXA
- Peripheral DEXA
- pQCT
- Quantitative ultrasound
-
Q. How much does fracture risk increase for every 1 SD fall in BMD T score?
- 2 times increase risk
-
Q. Where is peripheral QCT measured?
- Forearm
- Calcaneus
- Finger
-
Q. What are the advantages and disadvantages of pDEXA (Peripheral DEXA)?
- Advantage- Portable
- Disadvantage
- Cannot be used for classifying based on the WHO model
- Cannot be used for follow-up treatment
-
Q. What parameters are measured using quantitative ultrasound (QUS)?
- It does not measure BMD
- But measures
- SOS – speed of sound
- Stiffness Index- SI
- Quantitative ultrasound index
- Broadband ultrasound attenuation
-
Q. Is QUS a good fracture predictor?
- Yes
-
Q. What are the disadvantages of QUS?
- WHO criteria are not based on QUS
- It cannot be used to monitor therapy as it changes very slowly
- It cannot be used for treatment decisions as no trials are based on it
-
**pQCT **
-
Q. What is measured in pQCT?
- Volumetric BMD – in mg/cm3
- DEXA measure in g/cm2
-
Q. What is the biggest advantage of pQCT?
- Measurement of Cortical and trabecular fractions of the bone
- It is mainly a research tool at present since it is more expensive and more radiation is used
-
Q. Can it be used for FRAX calculation?
- Yes hip QCT adjusted for BMD can be entered into the FRAX data
-
**Newer techniques **
-
Q. What is [[TBS (Trabecular bone score)]]?
- It is the trabecular bone score
- It is a software addition to the DEXA machine
- It gives the texture of the bone which correlates with the bone microarchitecture
- It can be used with FRAX
-
Q. How do you interpret TBS?
- High TBS values suggest a more homogenous texture of bone suggesting good bone microarchitecture and lower fracture risk
- Low TBS suggests a higher fracture risk
- This has been validated in several studies
-
Q. What are the interpretation based on exact values?
- TBS
- ≥1.350 → Normal
- 1.200-1.350 → Partially degraded microarchitecture
- ≤1.200 → degraded microarchitecture
- TBS
-
Q. In which cases is TBS particularly useful?
- It is a useful addition to FRAX, especially in cases where FRAX is likely to underestimate the fracture risk
- Examples are [[Type 2 Diabetes mellitus]] and [[Primary hyperparathyroidism (PHPT)]]
-
Q. What is the advantage of HR- pQCT?
- Cell tells about the bone microarchitecture
- micro MRI can give similar information
-
Q. What is Hip structural analysis?
- It takes data obtained from the DEXA to look at hip parameters
- It measures Hip axis length which correlates with fracture risk and other parameters like Neck shaft angle etc
-
Skeletal site to measure
-
Q. Which are common sites for DEXA?
- ISCD recommends
- Hip
- Lumbar
- For assessment commonly
- However, if they cannot be assessed – a distal radius can be used
- Lumbar is less useful in the elderly who have degenerative disc disease and aortic calcification
- ISCD recommends
-
Q. Which are the 2 most important non-BMD risk factors for fracture?
- Advancing age
- Previous fracture
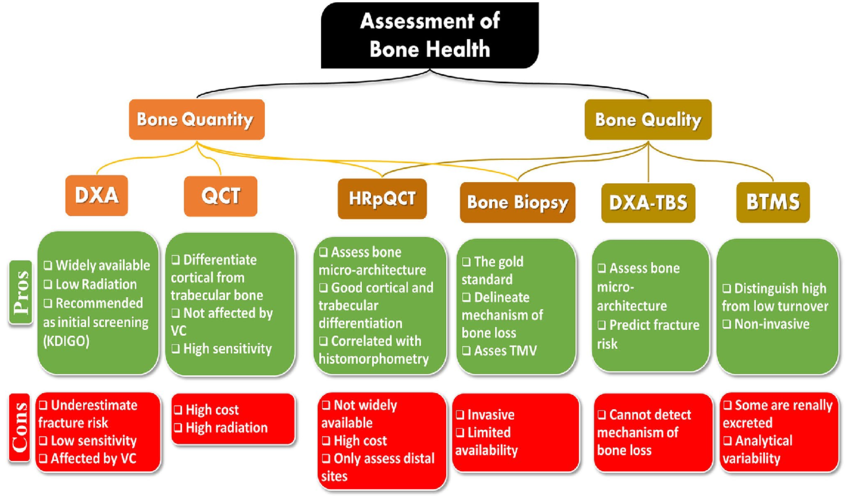
- Q. Give the parameters which help to assess bone quality and bone quantity
- Please see the flow chart below
References:
- Camacho PM, Petak SM, Binkley N, Diab DL, Eldeiry LS, Farooki A, Harris ST, Hurley DL, Kelly J, Lewiecki EM, Pessah-Pollack R. American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis—2020 update. Endocrine Practice. 2020 May 1;26:1-46
- Abdalbary M, Sobh M, Elnagar S, Elhadedy MA, Elshabrawy N, Abdelsalam M, Asadipooya K, Sabry A, Halawa A, El-Husseini A. Management of osteoporosis in patients with chronic kidney disease. Osteoporosis International. 2022 Nov;33(11):2259-74.