Join our WhatsApp channel to get regular updates from “Notes in Endocrinology” and “Endocrinology India”: https://whatsapp.com/channel/0029VaFyQnfHbFUz0LVdBO3****h
Support us:
- Support you by Becoming a YouTube member (Click here).
- Premium Membership- Download PDF version of Notes, Get ad free video and more
- Consultant Membership- Above plus Download Powerpoint presentation of the notes
- Support us by purchasing our book - Click here for more details:
- Q. What are the 2 major aspects of management of osteoporosis ?
- Lifestyle measures
- Pharmacological therapy
- **Lifestyle measures **
- Q. What are the lifestyle measures ?
- exercise- weight bearing
- Adequate calcium and vitamin D - 1200 mg and 800 IU for adults
- Avoid smoking
- Reduce alcohol intake
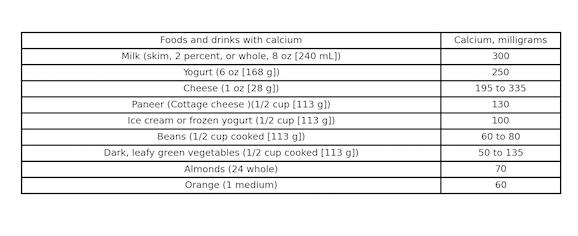
- Q. Give the sources of Calcium ?
- **Pharmacological therapy **
- Q. What is the indication for pharmacological therapy for osteoporosis ?
- Hip or vertebral fragility fracture
- T score < -2.5 at femoral neck, total hip or vertebral BMD
- Osteopenia + FRAX score of >3% at hip and >20% elsewhere
- **Choice of drug **
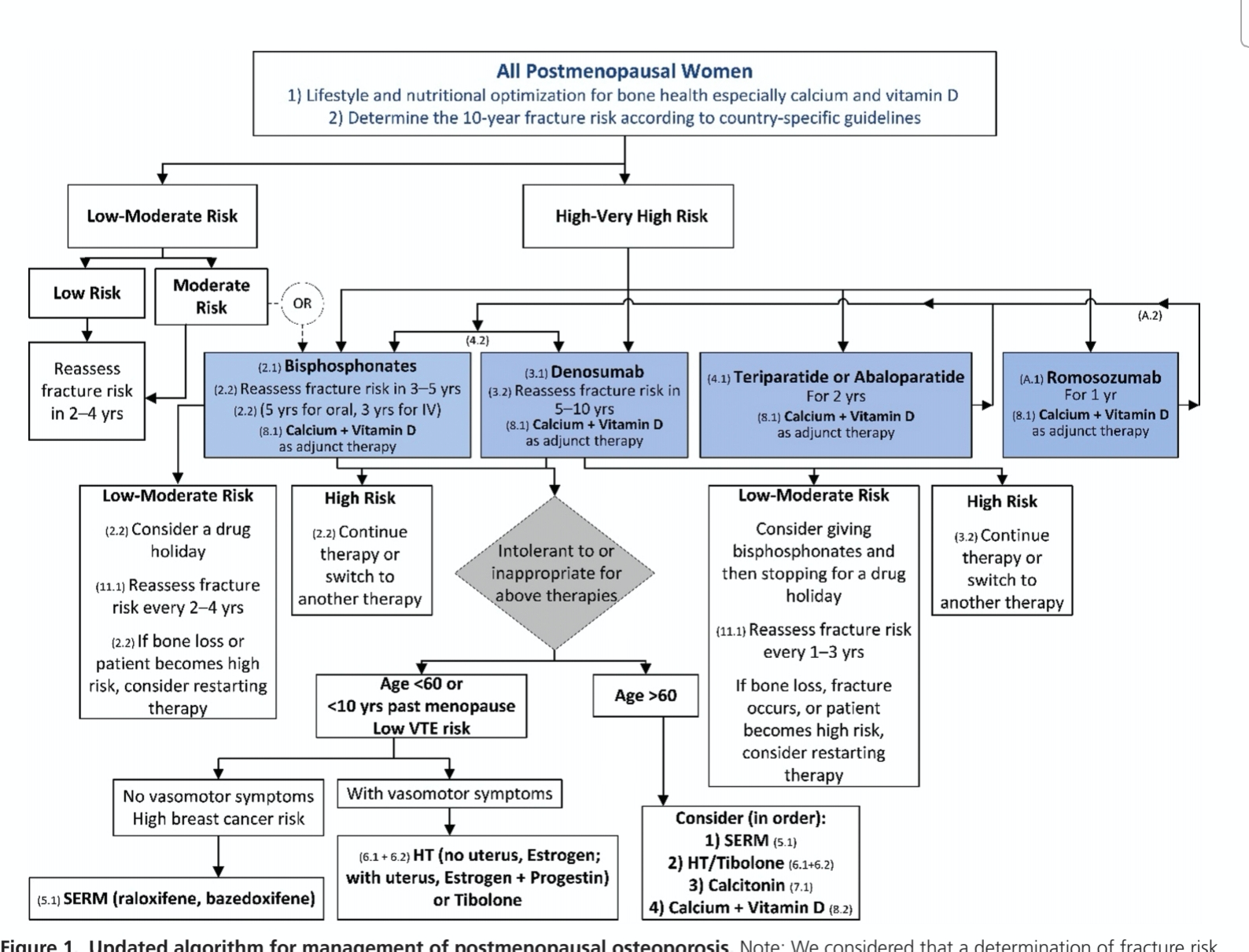
- Q. Give the outline for management of osteoporosis based on Endocrine society guidelines for post-menopaual osteoporosis ?
- Q. Give the outline based on AACE guidelines
- Q. What are contrainidcations to oral bisphosphonates ?
- Esophageal disease
- GFR <30
- Q. In which cases is teriperatide used as initial therapy ?
- Those with severe osteoporosis defined as
- Initial T score <-3.5
- Initial T score <-2.5 with presence of fragility fractures
- Teriparatide is given for 24 months and followed up with Bisphosphonates
- Those with severe osteoporosis defined as
- **Monitoring response to treatment **
- Q. When is BMD repeated after starting initial therapy ?
- BMD is repeated after 2 years
- If BMD is stable or improved – then monitor less frequently thereafter
- Q. When are Bone turnover markers typically used while monitoring therapy ?
- They are typically used in patients in whom either patient is not complaint or they have malabsorption and the effect or oral drugs is not certain
- Q. Which are the two most commonly done BTM ?
- CTX - otherwise called Beta-crosslaps in serum - Bone resorption marker
- Also done at Lal path labs (https://www.lalpathlabs.com/SampleReports/R168.pdf)
- test is called "TA CROSSLAPS; BETA CTx"
- test code: R168
- 2 mL (1 mL min.) plasma from 1 Lavender Top (EDTA) tube. Overnight fasting is mandatory. Ship refrigerated or frozen.
- P1NP most commonly used bone formation marker
- Serum propeptide of type I collagen (PINP). It is a bone formation Bone turn over marker (BTM) very useful in monitoring for Teriparatide
- It is available at Lal Path lab- test code is B165A
- Also available at Metropolis - P0001- Cost is Rs. 1650
- CTX - otherwise called Beta-crosslaps in serum - Bone resorption marker
- Q. Do Indians have a different bone turnover than others ?
- Yes
- In Indian Bone turnover is 20-30% more than caucasians
- Q. What are the normal BTM values in Indians ?
- Normal values of BTM in India
- Normal values of BTM in India
- Q. How can you use Bone turnover markers to guide the use of appropriate drugs for osteoporosis ?
-
- If P1NP and CTX are both high- this is suggestive of increased bone turnover- use Anti-resorptive agents
-
- If P1NP and CTX are both low- this is suggestive of low turnover- use Anabolic therapy
-
- If P1NP is low and CTX is high- It suggest more bone destruction but less bone formation- use anabolic therapy first and then use anti-resorptives
-
- Q. What are some innovations from Indian institutions regarding this ?
- even a single dose of Zolendronate can lead to good bone mass for a long time- this can be detected using BTM - from CMC
- If Teriperatide is taken for even 4 days in a week- it is effective - From PGI
- Q. How to do the Bone turnover markers test ?
- test to be done in the morning
- Fasting
- 8-10 am
- In female- in the follicular phase
- Q. How are Bone turnover markers useful in patients with Type 2 Diabetes mellitus and osteoporosis ?
- They often have normal DEXA
- BTM - show reduced bone turnover- low values of both BTM
- But have more vertebral fractures
- Q. When is change in BMD considered significant ?
- Change in BMD is considered significant when it is more or less than the least significant change
- Q. What is the least significant change ?
- LSC is the 2.77 times the precision error in measurement of BMD at each site by a particular technologist
- Precision error can be calculated using ISCD calculator
- It should be measured by the technologist himself
- Machine also give the LSC values but they may be less than the error by a technologist
- It is given in g/cm2
- Q. Tell me more about this ?
- So every operator of a DEXA machine need to calculate his or he precision error. This is done using ISCD Calculator in which he or she enters two or more scan readings of th about 15-30 patients.
- Based on this the precision error is calculated and the Least significant change is calculated as 2.77 x precision error
- Now when we see the scan, we need to compare the current with previous DEXA and need to see the change in the BMD
- This change in BMD has to be more than the LSC to be considered significant
- Q. Describe the step wise management of Osteoporosis in post-menopausal women based on Newer guidelines and newer evidence
- Step 1: Baseline assessment
- BMD-DEXA
- FRAX score
- Basic tests
- Calcium
- Vitamin D
- PTH
- ALP
- Serum creatinine
- Clinical assessment of other secondary causes based on history, clinical signs and symptoms
- Cushing syndrome - Iatrogenic or Endogenous
- Breast cancer risk
- Use of other osteoporosis causing medication
- Risk or currently having Diabetes mellitus
- Thyrotoxicosis
- Rheumatoid arthritis
- Malabsorption
- Post-bariatric surgery
- CKD
- CLD
- Post-transplant
- Indication of Vertebral fracture assessment / spine X ray:
- ≥ 4 cm height loss
- kyphosis
- recent or current long-term oral glucocorticoid therapy.
- Unexplained back pain or radicular pain
- If patient is found to have any secondary cause of osteoporosis refer to Endocrinologist for management of Endocrine condition or Rheumatologist for Rheumatological condition
- Explain lifestyle measures/ vitamin D and calcium to all patients as needed
- Primary osteoporosis- move to step 2
- Step 2: Risk assessment
-
- Low / Moderate risk
- All of the following:
- T score- greater than -2.5
- 10 year FRAX risk score for Hip fracture < 3%
- 10 year FRAX risk score for Major osteoporotic fracture - <20%
-
- High risk
- Any of the following:
- T score- less than -2.5
- 10 year FRAX risk score for Hip fracture > 3%
- 10 year FRAX risk score for Major osteoporotic fracture - >20%
- With NO current or prior history of fragility fracture
-
- Very high risk
- Prior or current history of fragility fracture or multiple vertebral fracture
-
- Step 3- First line management
- a) Risk Based
- b) BTM based
- Step 3A- Risk based
- Low/Moderate risk- No specific treatment - reassess every 2-4 years. In some cases Alendronate may be given
- High risk
- Cost is not a factor and no contraindication - Consider Denosumab therapy
- Cost is an issue and no contraindication- consider Bisphosphonates - Alendronate or Zolendronate
- Presence of contraindications to above therapy- see second line agents
- Very high risk
- Teriperatide
- Second line therapy- for those having contraindications to first line therapies
- Age >60 years
- Raloxifene - SERM
- Age <60 years
- No vasomotor symptoms or prior current or family risk of breast cancer- Raloxifene
- Vasomotor symptoms with no contraindications
- No uterus- Estrogen alone
- With uterus
- Estrogen + progesterone HRT/MHT or
- Tibolone
- Age >60 years
- Step 3B- BTM based:
-
- If P1NP and CTX are both high- this is suggestive of increased bone turnover- use Anti-resorptive agents
-
- If P1NP and CTX are both low- this is suggestive of low turnover- use Anabolic therapy
-
- If P1NP is low and CTX is high- It suggest more bone destruction but less bone formation- use anabolic therapy first and then use anti-resorptives
-
- Step 4 - Follow-up
- BTM every 3 months (optional)
- DEXA every 2 years with same machine and operator ideal
- Step 1: Baseline assessment
- **Decline of bmd on treatment **
- Q. What is done if there is decline in BMD more than LSC on treatment when the patient is on therapy ?
- Step 1
- If BMD declines on treatment or there is fracture while on therapy then first step is to do the following:
- Check the vitamin D and calcium intake
- Check adherence to therapy
- Check absorption of oral agent
- If all of these are checked and verified then go to next step
- If BMD declines on treatment or there is fracture while on therapy then first step is to do the following:
- Step 2
- See the magnitude to decline
- If decline is <5% - then continue the same drug and repeat DXA after 2 years
- If decline is >5%- then switch to IV bispho or other alternative therapies
- Step 3
- If there are fractures while on treatment with antiresorptives then consider switching to Teriparatide
- Teriparatide is less effective when used after antiresorptive and more effective is used before antiresorptive
- Step 1
- special cases and other notes
- Q. When are bisphosphonates started after fracture ?
- It is typically started 4-6 weeks after fracture
- Q. What are the non bone effects of Raloxifene in post menopausal women ?
- Reduces risk of breast cancer
- Neutral on heart and endometrium
- Increase hot flashes and risk of thromboembolic event
- Q. Which drugs are no more used for osteoporosis ?
- Calcitonin
- Strontium
- Q. When do Bone turn over marker normalize after osteoporosis therapy ?
- Bone breakdown marker- 3-6 moths
- Bone formation marker- 6-9 months
- *Drug holiday in case of Bisphosphonates **
- Q. After what period of time of Bisphosphonates use can you give drug holiday ?
- The decision to initiate a bisphosphonate holiday typically depends on the individual patient's risk factors and response to therapy. However, some general guidelines can be applied.
- For oral bisphosphonates, a drug holiday may be considered after 5 years of continuous therapy.
- For intravenous bisphosphonates like zoledronic acid, a drug holiday may be considered after 3 years of therapy.
- Q. Which patients should not be considered for Drug holiday ?
- Subgroups of patients who might benefit from continued therapy without a holiday at 5 (oral) or 3 (IV) years of therapy include those with a T-score <-2.5 at the hip, recent fracture on therapy, and prevalent spine fractures.
- Q. How are BTM used for monitoring Drug holiday with Bisphosphonates
- BTM can be used here
- If CTX <100 pg/ml and P1NP <30 ug/ml - we can give drug holiday
- Monitor using the BTM
- if the levels start increasing more than 3 x the last value - then consider zoledonate again
- Q. How long is the drug holiday generally given ?
- The duration of a bisphosphonate holiday can vary greatly depending on individual patient factors, including their risk of fracture, age, and overall health status.
- Generally, a bisphosphonate holiday can last anywhere from 1 to 5 years.
- During this time, it's crucial to continue monitoring the patient's bone health and fracture risk.
- The decision to resume therapy should be based on an individualized assessment of the patient's risk-benefit profile.
- High-risk patients may need to resume therapy sooner, while low-risk patients may be able to extend their holiday for a longer period.
- Q. In which situation we generally restart treatment for patient on a drug holiday ?
- Treatment with bisphosphonates is generally restarted for patients on a drug holiday in the following situations:
- If there is a significant decrease in bone mineral density (BMD) as indicated by a T-score that falls below -2.5 at the hip or spine.
- If the patient experiences a new osteoporotic fracture during the holiday period.
- If the patient had a very high risk of fracture before the start of the holiday, such as a history of multiple fractures, a T-score of <-2.5, or other significant risk factors.
- If there is a significant increase in bone turnover markers, suggesting accelerated bone loss.
- If the patient's overall health status or risk factors change in a way that increases their fracture risk.
- Treatment with bisphosphonates is generally restarted for patients on a drug holiday in the following situations:
- January 11th, 2024
- Q. True or false, Teriperatide is the only drug approved for the management of osteoporosis in men ?
- True
- All other agents have trials in post-menopausal women and not in men
- Q. When is Testosterone therapy considered for older men with osteoporosis ?
- Testosterone <200 ng/dl
- Organic cause of hypogonadism
23-Jan-2024
- Q. Give us some guidance regarding sequential therapy based on recent data
- According to a recent review published in the JCEM the following points are noted:
- For patients who discontinue denosumab, follow-on antiresorptive therapy is required to prevent the overshoot in bone remodeling and minimize subsequent bone loss.
- Transitioning from denosumab to teriparatide (and most likely abaloparatide) should be avoided as this leads to accelerated bone remodeling and rapid bone loss.
- Following bone-forming and dual-acting agents with an antiresorptive is required to maintain the achieved bone mineral density gains.
- In postmenopausal women who have not received any prior bone-targeted therapy, the greatest gains in bone mass are achieved with the initial use of a bone-forming/dual-acting drug followed by an antiresorptive.
- Initial therapy with a bisphosphonate may modestly diminish the bone effects of subsequent bone-forming or dual-acting drugs but prior antiresorptive use is not a contraindication to anabolic therapy.
- Ref: Ramchand SK, Leder BZ. Sequential Therapy for the Long-Term Treatment of Postmenopausal Osteoporosis. The Journal of Clinical Endocrinology & Metabolism. 2023 Aug 23:dgad496.
- According to a recent review published in the JCEM the following points are noted: