- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support us by purchasing our book - Click here for more details: Volume 1- THE BEST OF NOTES IN ENDOCRINOLOGY BOOK SERIES
- Support you by Becoming a YouTube member (Click here)
-
INTRODUCTION
-
Q. What is the definition of CKD – MBD?
- CKD-MBD is the metabolic bone disease typically seen at GFR <40
- It has three parts
- a) Abnormal biochemical parameters- Abnormal Calcium, Phosphate, PTH
- b) Abnormal bone metabolism - e.g., Adynamic bone disease
- c) Extraskeletal Calcium deposition
-
Q. Give the sequence of events in the pathogenesis of CKD-MBD?
-
-
Q. Summarize the points in pathogenesis of CKD-MBD?
- Pathogenesis factors for CKD-MBD
- a) Phosphate retention
- b) Reduced production of Active vitamin D (Calcitriol)
- c) Increased PTH
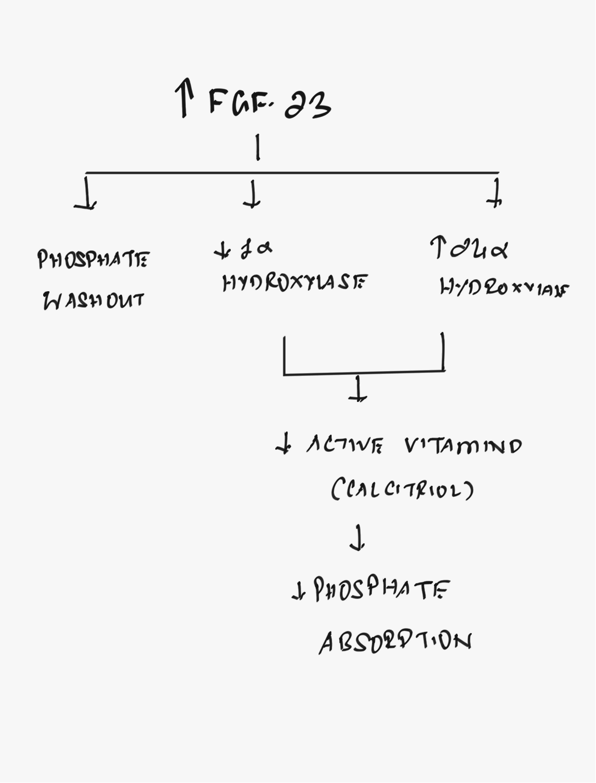
- d) Increased FGF-23
- e) Reduced FGFR1 and Klotho actions
-
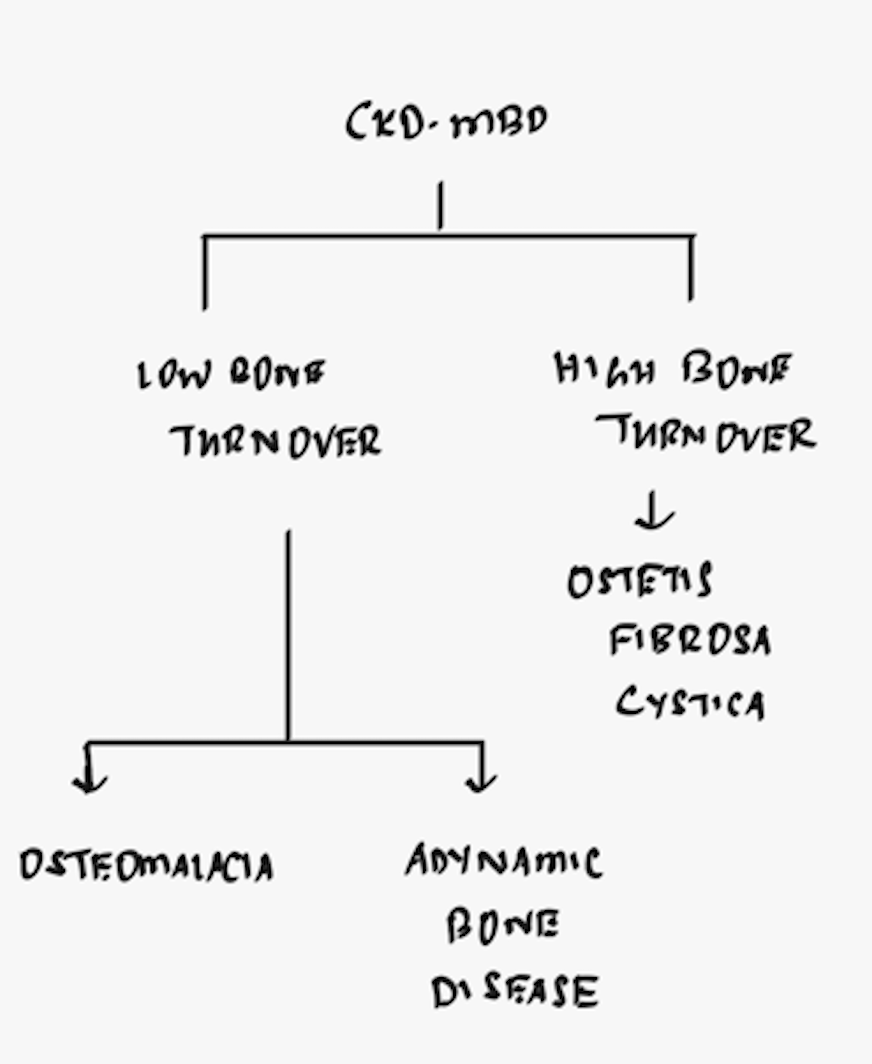
Q. What is the TMV system?
- Abnormalities of
- Turnover of bone
- Bone Mineralization
- Bone volume Volume
-
Q. What are the disorders of TMV seen in CKD-MBD?
- Osteitis fibrosa cystica- Increase turnover
- Osteomalacia- reduced mineralization
- Adynamic bone disease- reduced turnover
- Mixed disorder- a combination of above
-
MANAGEMENT OF CKD-MBD
-
Q. What tests are done for monitoring in patients with CKD-MBD, and how frequently?

- Ref: Morrone LF, Russo D, Di Iorio B. Diagnostic workup for disorders of bone and mineral metabolism in patients with chronic kidney disease in the era of KDIGO Guidelines. International journal of nephrology. 2011 Apr 7;2011.
-
Q. What should be the target phosphate levels in CKD-MBD?
- KDOQI guidelines
- Not on dialysis- <4.5 mg/dl
- On dialysis- 3.5-5.5 mg/dl
-
Q. Summarize the management options for management for phosphate for patients with CKD- MBD?
-

-
Q. What are the advantages of non calcium over calcium containing phosphate binders?
- Less adynamic bone disease
- Less vascular calcification
- Less mortality
-
**MANAGEMENT OF HYPERPARATHYROIDISM IN CKD **
-
Q. Describe the step wise management of hyperparathyroidism in CKD patient not on dialysis?
-
- Correct the hyperphosphatemia
-
- Add Cholecalciferol and keep it in target of 30 ng/ml
-
- Add Add Calcitriol if PTH above target and 25-Hydroxyvitamin D is >30 ng/ml
-
-
Q. What are the PTH targets for patient not on dialysis ?
- GFR:
- 30-60 – PTH 35-70 pg/ml
- 15-30 – PTH 70-110 pg/ml
- <15 - PTH 150-300 pg/ml
- GFR:
-
Q. Summarize the targets in patient with Stage 5 CKD?
- Calcium- 8.5-9.5 mg/dl
- Phosphate- 3.5-5.5 mg/dl
- PTH- 150-300 pg/ml
- Ca x P <55
-
Q. Describe the management of hyperparathyroidism in CKD patient on dialysis?
-
- Control the phosphate - get it in the target range with diet, drugs or dialysis
-
- Avoid hypocalcemia → Correct the calcium if required
-
- Recheck the PTH
- if <150-300 pg/ml → follow-up the patient
- If >300 pg/ml- move to step 4
-
- Additional drugs
- If S. Calcium >8.5 mg/dl → consider adding Cinacalcet (The use of Cinacalcet is considered controversial)
- If S. Calcium <8.5 mg/dl → consider adding Calcitriol
-
-
Q. Give the summary for targets of various parameter at various stages for patient with CKD?
-
GFR 30-60
- Calcium- 8.5-10.0 mg/dl
- Phosphate- <4.5 mg/dl
- PTH- 35-70 pg/ml
- Monitor:
- PTH every 6-12 months
- Calcium and phosphate- 6-12 months
- 25 hydroxy vitamin D – annually
-
GFR 15-30
- Calcium- 8.5-10.0 mg/dl
- Phosphate- <4.5 mg/dl
- PTH- 70-110 pg/ml
- Monitor:
- PTH every 6-12 months
- Calcium and phosphate- 3-6 months
- 25 hydroxy vitamin D – annually
-
GFR <15
- Calcium- 8.5-9.5 mg/dl
- Phosphate- 3.5-5.5 mg/dl
- PTH- 150-300 pg/ml
- Monitor:
- PTH every 3-6 months
- Calcium and phosphate- 1-3 months
- 25 hydroxy vitamin D – annually
-
-
CKD-MBD other points
-
Q. How do you diagnose adynamic bone disease in CKD-MBD?
- Bone biopsy- gold standard
- Low PTH - <100 pg/ml in presence of hypercalcemia
- Low ALP
- Low bone specific alkaline phosphatase (BSAP)
-
Q. Why do patient with CKD have increase CV risk?
- Increase vascular calcification- main point- lead pipe rigidity of the blood vessels
- Hypertension
- Increase Ca x P product, hypercalcemia, hyperphosphatemia
- Increase FGF23
- Reduced klotho
-
Q. What are the indications for parathyroidectomy in CKD patient?
- Severe Hypercalcemia
- Calciphylaxis
- Fractures
- Bone pain
- Intracable pruritis
- PTH unresponsive to vitamin D and its analogs
- Documented Hyperplasia / autonomous PTH gland or glands
-
Q. What are 2 important complications of parathyroidectomy in CKD patients?
- Hungry bone syndrome
- Adynamic bone disease
#Updates 12-Jul-2022 . Source: Ebeling PR et al [Ebeling PR , Nguyen HH, Aleksova J, Vincent AJ, Wong P, Milat F. Secondary osteoporosis. Endocrine Reviews. 2022 Apr;43(2):240-313]
-
Q. What exactly is "Renal osteodystrophy" ?
- This is part of CKD-MBD
- This mainly deals with Histomorphometric changes in CKD
-
Q. What is the earliest abnormality that occurs in CKD-MBD ?
- The earliest change that occurs is an increase in FGF23 and a decline in its coreceptor Alpha-Klotho
-
Q. What is the relationship between FGF23 and Alpha-Klotho?
- For the FGF23 to function it requires the presence of a co-receptor Alpha-Klotho
- Now, klotho is present only in Bones, kidneys and brain - hence other parts of the body are not affected by FGF23
- Also Klotho gives negative feedback to FGF23 production keeping it in check
-
Q. What happens as a consequence of FGF23 increase in Early CKD?
- The increase in FGF23 is an adaptive process to control the phosphate retention
- However because of the reduction of Klotho, though FGF23 increases, its effectiveness is reduced

-
Q. What happens later in CKD?
- Later on, the Klotho reduces so much, that FGF23 reduces its effect
- Because of reduced Calcitriol and phosphate retention the negative feedback on PTH is reduced and hence PTH increases
- Now the phosphate loss is dependent on PTH and not FGF23
- Later on, though PTH is high, the nephron loss is so much that the effect of both PTH and FGF23 on nephron is lost and phosphate retention multiplies
-
Q. What happens to the WNT/Beta-catenin pathway?
- CKD activates DKK1 and Sclerostin levels that inhibit the WNT/Beta-catenin pathway
- The above pathway is involved in bone formation
-
Q. What are the three major bone disorders seen in patients with CKD?
- Though there are three entities - they are NOT distinct and a combination of the following always exists in patients with CKD
-
Q. What happens to the cortical bones in CKD?
- There is "Trabecularization" of the cortical bones in patients with CKD with an increase in trabecular volume
-
Q. What type of fractures are predominant in CKD? (Important pearl)
- Patients with CKD have a loss of cortical bone
- Non-vertebral and peripheral fractures predominate in such patients- areas having more cortical bone have a loss of the same leading to more fracture risk
- Some people believe that perhaps the vertebral fractures are under-reported
-
Q. What are the other factors in patients with CKD that contribute to the bone disease?
-
- Use of unfractionated heparin in patients on dialysis
-
- Nutritional issues- anemia, sarcopenia, etc
-
- Gonadal dysfunction
-
- Associated Diabetes mellitus may contribute to the pathogenesis
-
-
Q. What is the gold standard for assessment of bone disease in patients with CKD-MBD?
- Tetracycline labeled bone biopsy
-
Q. Should a DEXA scan be done in patients with CKD?
- In stages 1-3 of CKD, DEXA scan is a must
- However, the use of DEXA in CKD 4-5, especially for dialysis patients is debatable
-
Q. What are the issues with using DEXA in CKD 4-5?
-
- The main problems here involve turnover issues and microarchitecture disturbances. Hence a DEXA may underestimate fracture risk
-
- Aortic vascular calcification may cause false high DEXA results in the vertebra
-
-
Q. How to interpret DEXA in CKD 4-5?
- Rely more on hip and radius compared to the vertebral BMD
- Low Hip and Radius scores correlate with the risk of fracture in CKD patients
-
Q. What are the roles of biochemical markers in this case?
- Both P1NP and CTX are falsely high due to lower clearance of these markers in CKD
- PTH and Bone specific alkaline phosphatase are useful, however a recent study has shown that it has a low predictive value for fractures
-
Q. What is the impact of increased phosphate on bone turnover?
- Phosphate reduces osteoclast reabsorption and osteoblast formation
- It inhibits bone turnover
- Hence overall, control of the phosphate levels should be a priority
-
Q. What should be the PTH targets in advanced CKD when using active vitamin D to suppress the PTH?
- PTH value should be 2-9 times the upper limit of normal
-
Q. Is there any role of calcimimetics at present?
- Though they control the PTH levels, the evidence for their benefits in fracture reduction is not seen
- Hence they are not recommended in Pre-dialysis patients
-
Q. In patients in whom parathyroidectomy is recommended, does it improve bone outcomes?
- Yes
- Parathyroidectomy reduces the risk of fractures in CKD patients
-
Q. If the patient is hypogonadal- should hormone replacement be suggested?
- Yes and no
- If there is a clearly defined cause for hypogonadism- hormone replacement must be done
- For example, if the patient has low testosterone due to a defined pituitary cause- testosterone replacement must be done
- For women SERMs may be preferred
-
Q. What about the use of anti-resorptive agents?
- Oral Alendronate has some data in CKD stages 3-4 and has shown fracture risk reduction
- The FREEDOM trial for Denosumab has evidence for CKD stages 3-4 as well and has shown good fracture reduction
- There are small trials in dialysis patients with these drugs, but fracture data is missing
- Also in the larger trials, patients were not on dialysis and patients did not have mineral disorders - hence difficult to generalize to a more routine CKD population
-
Q. What about anabolic agents?
- Small trials have shown benefits for these agents in CKD
- However, we need more data for the same
- Q. Give the algorithm for the management of osteoporosis in advanced CKD G4 and G5 as given by the European consensus statement
Video Lecture
References:
- Ebeling PR , Nguyen HH, Aleksova J, Vincent AJ, Wong P, Milat F. Secondary osteoporosis. Endocrine Reviews. 2022 Apr;43(2):240-313
- Evenepoel, P., Cunningham, J., Ferrari, S., Haarhaus, M., Javaid, M.K., Lafage-Proust, M.H., Prieto-Alhambra, D., Torres, P.U. and Cannata-Andia, J., 2021. European Consensus Statement on the diagnosis and management of osteoporosis in chronic kidney disease stages G4–G5D. Nephrology Dialysis Transplantation, 36(1), pp.42-59.
