-
- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
- Credits
-
Q. Give the Recommended daily allowance of vitamin D?
- infants- 400 IU
- Children- 600 IU
- Adults (<70 years)- 600 IU
- Elderly (>70)- 800 IU
- Pregnant and Lactating- 600 IU
-
Q. What is the tolerable upper limit of vitamin D?
- Infant 0-6 months- 1500 IU
- Infant 6-12 months- 2500 IU
- Child 1-5 years – 3000 IU
- Child >5 years and adults – 4000 IU
- However, short term ingestion of 10,000 IU / day poses no risk
- Dose >10,000 IU/day – toxicity can occur
-
Q. What are symptoms of vitamin D toxicity?
- Acute or Subacute toxicity
- Neurological symptoms- confusion, coma, muscle weakness
- Nephrogenic Diabetes insipidus
- polyuria
- polydipsia
- GI symptoms
- anorexia
- vomiting
- Chronic toxicity
- nephrocalcinosis
- nephrolithiasis
- bone demineralization
- Acute or Subacute toxicity
-
Q. Does excess vitamin D increase the risk of falls?
- Yes
- Some recent studies have shown that excess vitamin D increases the risk of falls.
-
Q. How is calcium reabsorbed in the thick ascending loop of Henle?
- The Na-K ATPase pump on the basolateral membrane drives 3 Na molecules out of the cell while two potassium molecules come in.
- Na-K-2Cl (furosemide sensitive Na channel) allows Na, K, and 2 Cl reabsorption – which is an electrically neutral process.
- Now cell has extra potassium, which is leaks out into the lumen
- Since Na is being pumped out and K is leaking out, there is a net negative charge inside the cell
- This allows Ca to enter the cell
-
Q. How does the Calcium sensing receptor receptor (CaSR) act in this area?
- Increase calcium → activation of CaSR → generation of arachidonic acid metabolite → suppress the Na-K ATPase pump → blocks the leaking potassium channel
- This disrupts the entire process, and hence calcium cannot be reabsorbed.
-
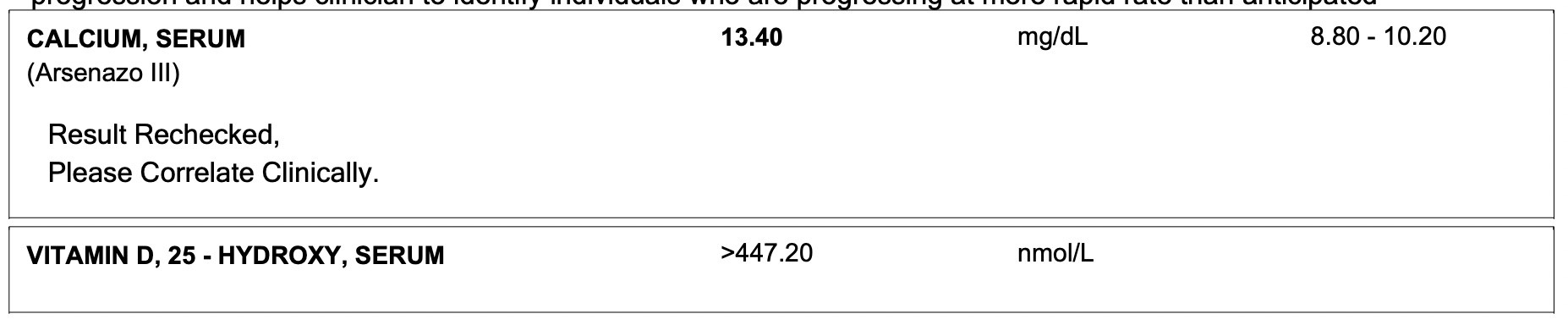
Q. What are the lab findings of vitamin D toxicity?
- Increase calcium
- Increase Phosphate
- Increase creatinine
- Dilute urine
- Hypercalciuria
- Reduce PTH
- Short QTc on ECG
-
Q. What level of 25-hydroxyvitamin D predisposes to toxicity?
-
Guidelines say >150 ng/ml leads to toxicity.
- However, current evidence says >80 ng/ml can predispose to toxicity
- However, toxicity depends on the amount of calcium intake, and hence all people with this level of vitamin D don’t develop toxicity
- This has to be kept in mind
-
Q. What produces hypercalcemia in hypervitaminosis of D ?
- Increase intestinal absorption
- Increased bone resorption
-
Q. Which vitamin D analogs can cause vitamin D toxicity?
- All of them can cause
- Calcitriol- highest risk
- Paracalcitol- lowest risk
- All of them can cause
-
Q. What is the difference in toxicity due to 25 hydroxyvitamin D and Calcitriol?
- The duration of toxicity
- Since calcitriol has a short half-life- the duration of toxicity is shorter but produces more acute symptoms
-
Q. What is the duration of toxicity of various vitamin D compounds?
- 25 hydroxyvitamin D- 15 days
- Alpha D3- 5 days
- Calcitriol- 2-5 days
-
Q. What is the management of patients with Vitamin D toxicity?
- Patients without renal failure
- Stop vitamin D and analogs
- Isotonic fluids +/- furosemide
- Glucocorticoids
- Patients with renal failure
- Stop offending drug
- Fluids +/- diuretics if required
- Glucocorticoids
- Hemodialysis with low calcium bath (if required)
- Patients without renal failure
-
Q. How does Glucocorticoid help?
- Reduces intestinal absorption of calcium
- Reduce 1 alpha-hydroxylase – reduce activation of vitamin D
-
- An elderly female had pain in her joints secondary to osteoarthitis
- She was prescribed a plethora of Vitamin D compounds in inappopriate doses including Calcitriol and calcium
- Presented to the emergency in coma with hypercalcemia and vitamin D toxicity
- The PTH value was 8 pg/ml suggesting PTH independent hypercalcemia
Please consider donating to "Notes in Endocrinology" to keep us going. Please visit our DONATION page to know more