Support us:
- Support you by Becoming a YouTube member (Click here).
- Premium Membership- Download PDF version of Notes, Get ad free video and more
- Consultant Membership- Above plus Download Powerpoint presentation of the notes and get access to EndoAI for Free
- Support us by purchasing our book - Click here for more details:
- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Also, see Non-Calciotropic actions of Vitamin D
-
Topic 1: Vitamin D and Diabetes
-
Q. Can vitamin D reverse Prediabetes ?
- Yes
- Benefit was found in nonobese subjects (RR 0.73 [95% CI 0.57–0.92]) but not in obese subjects (RR 0.95 [95% CI 0.84–1.08]) (__P__interaction = 0.048). [Ref: Zhang Y, Tan H, Tang J, Li J, Chong W, Hai Y, Feng Y, Lunsford LD, Xu P, Jia D, Fang F. Effects of vitamin D supplementation on prevention of type 2 diabetes in patients with prediabetes: a systematic review and meta-analysis. Diabetes Care. 2020 Jul 1;43(7):1650-8.]
- The reversion of prediabetes to normoglycemia occurred in 116 of 548 (21.2%) participants in the vitamin D group and 75 of 532 (14.1%) in the control group. Thus, vitamin D supplementation increased the reversion rate of prediabetes to normoglycemia (RR 1.48 [95% CI 1.14–1.92]; __I__2 = 0%.)
- In persons with prediabetes, vitamin D supplementation reduces the risk of T2DM and increases the reversion rate of prediabetes to normoglycemia.
- The benefit of the prevention of T2DM could be limited to non-obese subjects.

-
Q. But the D2D trial was negative! Shouldn't we go by this trial?
- Actually, No
- The subanalysis of the D2D trial looking at patients with vitamin D deficiency was POSITIVE

- In a post hoc analysis of data from participants with a baseline 25-hydroxyvitamin D level of less than 12 ng per milliliter (30 nmol per liter) (103 participants), the hazard ratio in the vitamin D group was 0.38 (95% CI, 0.18 to 0.80).
-
Q. Can Vitamin D help improve glycemic control in patients with established Type 2 Diabetes mellitus ?
- Yes.
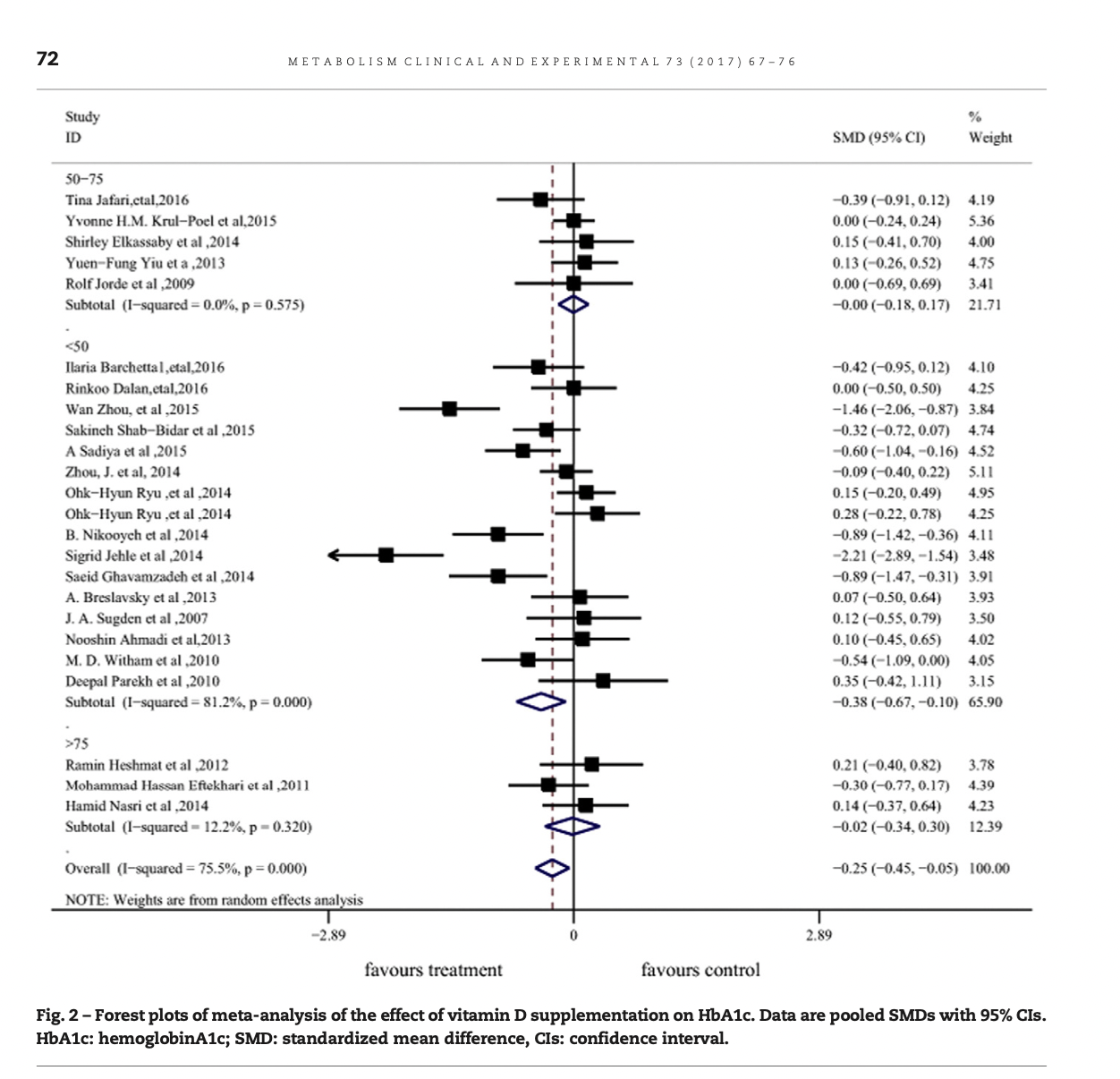
- Meta-analysis by Wu et al [1]
- Subgroup analyses suggested that vitamin D supplementation was associated with reduced HbA1c levels (SMD -0.39 [-0.67 to -0.10]) and FBG (SMD -0.27 [-0.46 to -0.07]) among patients with 25-hydroxyvitamin D (25(OH) D) deficiency at baseline.
- Significantly reduced HbA1c levels were also observed in association with vitamin D supplementation in the subgroup, including type 2 diabetes patients with a body mass index (BMI) <30kg m-2 (SMD -0.30 [-0.54 to -0.07]).
- Conclusion: Vitamin D supplementation could effectively improve glycemic control in vitamin D deficient or non-obese type 2 diabetes patients.
-
Q. Can Vitamin D reduce the incidence of Type 1 Diabetes in children?
- Yes
- Meta-analysis of the results of observational studies suggests that the risk of type 1 diabetes is significantly reduced in those who were supplemented in childhood with vitamin D compared to those who were not supplemented (odds ratio 0.71, 95% CI 0.60 to 0.84). [2]
- Conclusion: Vitamin D supplementation in early childhood may offer protection against the development of type 1 diabetes. The evidence for this is based on observational studies
- NOTE: The meta-analysis DID NOT include an RCT

-
Summary and Conclusion on Vitamin D and Diabetes
- Q. Can Vitamin D reverse diabetes?
- Can Vitamin D reverse diabetes - No.
- There is no evidence of Vitamin D "reversing" or producing remission in patients with established Type 1 and Type 2 Diabetes
- Q. Can Vitamin D reverse diabetes? No
- Q. Can Vitamin D reverse Prediabetes ? Yes
- Q. Can Vitamin D improve glycemic control in patients with established Type 2 diabetes? Yes
- Q. Can vitamin D prevent type 1 diabetes in children? Yes (*No RCT)
- Q. Can Vitamin D reverse diabetes?
-
Topic 2: Vitamin D and Hair
-
Q. Is Vitamin D deficiency more common in people who have alopecia areata?
- Yes
- Alopecia areata is an autoimmune disease
- A meta-analysis by Lee et al. - The subjects with alopecia areata had lower serum 25-hydroxyvitamin D level, and vitamin D deficiency was highly prevalent compared to non-AA controls. [3]
- Whether treatment with vitamin D has any benefit is debatable
-
Q. What are the potential mechanism by which Vitamin D deficiency is associated with Alopecia areata?
- Anagen stage hair follicles (HFs) exhibit “immune privilege (IP)” from the level of the bulge downwards to the bulb.
- Both passive and active IP mechanisms protect HFs from physiologically undesired immune responses and limit immune surveillance
- IP collapse is a key element in AA immunopathogenesis.
- IFN-γ is what leads to the collapse of IP
- Vitamin D may contribute to maintaining the IP of HF by decreasing the production of IFN-γ [4]

-
Q. Does treatment of vitamin D deficiency have any benefit on alopecia areata?
- This is not clear
- Calcipotriol, a vitamin D analog, has been reported to be topically used in treating alopecia areata, with promising results
- Topical Calcipotriol is more beneficial than oral vitamin D supplementation in AA (Ref: Abd-ElRaheem et al.)
- " Studies using topical vitamin D in alopecia are inconsistent and limited by small sample size or lack of appropriate controls. Preliminary results suggest a potential therapeutic benefit for topical vitamin D, with minor side effects." [5]
-
Q. What is the lesson to be learned from this pathogenesis?
- Vitamin D may have a role in other autoimmune diseases
-
Summary and Conclusion
-
Q. Can vitamin d deficiency cause hair loss?
- Patients having alopecia areata, a specific and important cause of hair loss, are more likely to have vitamin D deficiency.
- However, association does not always mean causation
- Correction of vitamin D deficiency may or may not have any impact on hair loss. There is little evidence to prove the same
- Topical Calcipotriol, a vitamin D analog, may have some role in managing alopecia areata.
- Most notably, Vitamin D deficiency indeed has a correlation with autoimmune diseases
-
Topic 3: Vitamin D and Obesity
-
Q. Do obese people have less vitamin D levels?
- Yes, and this is well known
- Meta-analysis by M Pereira-Santos et al. have suggested [6]
- The prevalence of vitamin D deficiency was 35% higher in obese subjects compared to the eutrophic group (PR: 1.35; 95% CI: 1.21-1.50) and 24% higher than in the overweight group (PR: 1.24; 95% CI: 1.14-1.34).
- These results indicate that the prevalence of vitamin D deficiency was more elevated in obese subjects.
- The vitamin D deficiency was associated with obesity irrespective of age, latitude, cut-offs to define vitamin D deficiency, and the Human Development Index of the study location.
-
Q. Why do obese people have lower vitamin D?
- There are several reasons for this, but the most likely being that obese people have large fat stores leading to lower 25 hydroxyvitamin D levels
- "High prevalence of vitamin D (VD) deficiency in obese subjects is a well-documented finding, most probably due to volumetric dilution into the greater volumes of fat, serum, liver, and muscle." [7]

-
Q. Does VItamin D deficiency cause obesity?
- Probably, not
- No data to suggest it
-
Q. Does Vitamin D deficiency CONTRIBUTE to obesity?
- Yes
- Vitamin D deficiency has a link with depression which in turn is linked with obesity
- Vitamin D deficiency is linked with increased muscle strength
-
Q. What is the link between Vitamin D deficiency and depression?
- Google Question: How much vitamin D should I take for depression?
- Spedding S et al. meta-analysis [8]
- A meta-analysis of all studies without flaws demonstrated a statistically significant improvement in depression with Vitamin D supplements (+0.78 CI +0.24, +1.27).
- Vitamin D supplementation (≥800 I.U. daily) was somewhat favorable in managing depression in studies that demonstrate a change in vitamin levels, and the effect size was comparable to that of anti-depressant medication.
-
Q. Does VItamin D supplementation improve muscle strength?
- Yes, it does
- Beaudet et al. meta-analysis [9]
- Results revealed a small but significant positive effect of vitamin D supplementation on global muscle strength with a standardized mean difference (SMD) of 0.17 (P = .02).
- Results on muscle strength were significantly more important with people who presented a 25-hydroxyvitamin D level <30 nmol/L.
- Supplementation seems also more effective on people aged 65 years or older compared to younger subjects (SMD 0.25; 95% CI 0.01 to 0.48 vs SMD 0.03; 95% CI -0.08 to 0.14)
-
Summary and Conclusion
-
Q. Can vitamin D deficiency cause weight gain? No
- Q. Do obese people have lower vitamin D ? Yes
- Q. Does Vitamin D supplementation help in depression? Yes
- Q. Does vitamin D supplementation help muscle strength? Yes
-
Topic 4: Other Topocs
-
Q. Are people with Vitamin D deficiency more likely to develop COVID-19 infection?
- Meta-analysis by Teshome et al
- "The pooled analysis showed that individuals with Vitamin-D deficiency were 80% more likely to acquire COVID-19 infection as compared to those who have sufficient Vitamin D levels (OR = 1.80; 95%CI: 1.72, 1.88). Begg's test also revealed that there was no significant publication bias between the studies (P = 0.764)." [10]
-
Q. Is there a link between VItamin D deficiency and increased risk of death due to COVID-19 infection?
-
Meta-analysis by Bassatne A et al [11]
-
"While the available evidence to date, from largely poor-quality observational studies, may be viewed as showing a trend for an association between low serum 25(OH)D levels and COVID-19 related health outcomes, this relationship was not found to be statistically significant.""
-
Recent trial published in the JCEM [12]
-
Case-control study done in 900 patients with calcifediol
-
"Out of 447 patients treated with calcifediol at admission, 20 (4.5%) required ICU, compared to 82 (21%) out of 391 non-treated (p-value<0.0001)"
-
In the Intention-to-Treat analysis, 21 (4.7%) out of 447 patients treated with calcifediol at admission died compared to 62 patients (15.9%) out of 391 non-treated (p=0.0001)
-
In patients hospitalized with COVID-19, calcifediol treatment significantly reduced ICU admission and mortality.
-
-
Q. Does Vitamin D deficiency lead to increased cardiovascular disease ?
-
Meta-analaysis by Barbarawi et al [13]
-
21 RCT were included- more than 80,000 patients
-
Vitamin D supplementation compared with placebo was not associated with reduced major adverse cardiovascular events (RR, 1.00 [95% CI, 0.95-1.06]; P = .85)
-
Nor the secondary end points of myocardial infarction (RR, 1.00 [95% CI, 0.93-1.08]; P = .92), stroke (RR, 1.06 [95% CI, 0.98-1.15]; P = .16), CVD mortality (RR, 0.98 [95% CI, 0.90-1.07]; P = .68), or all-cause mortality (RR, 0.97 [95% CI, 0.93-1.02]; P = .23
-
Vitamin D supplementation was not associated with reduced major adverse cardiovascular events, individual CVD endpoints (myocardial infarction, stroke, CVD mortality), or all-cause mortality. The findings suggest that vitamin D supplementation does not confer cardiovascular protection and is not indicated for this purpose.
-
Q. Does Vitamin D help in the prevention of cancer?
-
“Vitamin D was not associated with significant reduction of cancer incidence (RR: 0.96; 95% CI: 0.86–1.07; P = 0.46; I2 = 31%)" [14]
-
Colon cancer:
- Meta-analysis of the WHO working group
- Compared with 25(OH)D levels of 20 to <25 ng/mL (50 to <62.5 nmol/L), a 25(OH)D level of <12 ng/mL (30 nmol/L) was associated with a higher risk of colorectal cancer (RR 1.31, 95% CI 1.05-1.62), whereas 25(OH)D levels ≥30 ng/mL (75 nmol/L) were associated with a lower risk (RRs 0.81, 95% CI 0.67-0.99 and 0.73, 95% CI 0.59-0.91, for levels of 30 to <35 ng/mL [75 to <87.5 nmol/L] and 35 to <40 ng/mL [87.5 to <100 nmol/L], respectively).
-
Breast cancer
- A meta-analysis of prospective studies examining the relationship between serum 25(OH)D concentrations and breast cancer risk showed a significant inverse association in post- but not premenopausal women. The risk of postmenopausal breast cancer decreased with 25(OH)D levels between 27 and <35 ng/mL (67 to 87 nmol/L), with no further reduction for levels above 35 ng/mL.
-
Prostate cancer- there is no evidence from a meta-analysis
-
Q. Does Vitamin D reduce mortality in patients with cancer?
-
Vitamin D was associated with significant reduction of cancer-related mortality compared with placebo (RR 0.87; 95% CI: 0.79–0.96; P = 0.05: I2 = 0%) [15]
-

Video on the topic by Dr. Om J Lakhani
Ref: Wu C, Qiu S, Zhu X, Li L. Vitamin D supplementation and glycemic control in type 2 diabetes patients: a systematic review and meta-analysis. Metabolism. 2017 Aug 1;73:67-76. ↩︎
Ref: Zipitis CS, Akobeng AK. Vitamin D supplementation in early childhood and risk of type 1 diabetes: a systematic review and meta-analysis. Archives of disease in childhood. 2008 Jun 1;93(6):512-7. ↩︎
Ref: Lee S, Kim BJ, Lee CH, Lee WS. Increased prevalence of vitamin D deficiency in patients with alopecia areata: a systematic review and meta‐analysis. Journal of the European Academy of Dermatology and Venereology. 2018 Jul;32(7):1214-21 ↩︎
Lin X, Meng X, Song Z. Vitamin D and alopecia areata: possible roles in pathogenesis and potential implications for therapy. American journal of translational research. 2019;11(9):5285. ↩︎
Hosking AM, Juhasz M, Mesinkovska NA. Complementary and alternative treatments for alopecia: a comprehensive review. Skin appendage disorders. 2019;5(2):72-89. ↩︎
Pereira‐Santos M, Costa PD, Assis AD, Santos CD, Santos DD. Obesity and vitamin D deficiency: a systematic review and meta‐analysis. Obesity reviews. 2015 Apr;16(4):341-9. ↩︎
Ref: Vranić L, Mikolašević I, Milić S. Vitamin D deficiency: consequence or cause of obesity?. Medicine. 2019 Sep;55(9):541 ↩︎
Spedding S. Vitamin D and depression: a systematic review and meta-analysis comparing studies with and without biological flaws. Nutrients. 2014 Apr;6(4):1501-18. ↩︎
Beaudart C, Buckinx F, Rabenda V, Gillain S, Cavalier E, Sloman J, Petermans J, Reginster JY, Bruyère O. The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: a systematic review and meta-analysis of randomized controlled trials. The Journal of Clinical Endocrinology & Metabolism. 2014 Nov 1;99(11):4336-45. ↩︎
Teshome A, Adane A, Girma B, Mekonnen ZA. The Impact of Vitamin D Level on COVID-19 Infection: Systematic Review and Meta-Analysis. Front Public Health. 2021 Mar 5;9:624559. DOI: 10.3389/fpubh.2021.624559. PMID: 33748066; PMCID: PMC7973108 ↩︎
Bassatne A, Basbous M, Chakhtoura M, El-Zein O, Rahme M, El-Hajj Fuleihan G. The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis. Metabolism. 2021 Jun;119:154753. DOI: 10.1016/j.metabol.2021.154753. Epub 2021 Mar 24. PMID: 33774074; PMCID: PMC7989070. ↩︎
Rogues X, Ovejero D, Pineda-Moncusí M, Bouillon R, Arenas D, Pascual J, Ribes A, Guerri-Fernandez R, Villar-Garcia J, Rial A, Gimenez-Argente C, Cos ML, Rodriguez-Morera J, Campodarve I, Quesada-Gomez JM, Garcia-Giralt N. Calcifediol treatment and COVID-19-related outcomes. J Clin Endocrinol Metab. 2021 Jun 7:dgab405. doi: 10.1210/clinem/dgab405. Epub ahead of print. PMID: 34097036; PMCID: PMC8344647. ↩︎
Barbara M, Kheiri B, Zayed Y, Barbara O, Dhillon H, Swaid B, Yelangi A, Sundus S, Bachuwa G, Alkotob ML, Manson JE. Vitamin D Supplementation and Cardiovascular Disease Risks in More Than 83 000 Individuals in 21 Randomized Clinical Trials: A Meta-analysis. JAMA Cardiol. 2019 Aug 1;4(8):765-776. DOI: 10.1001/jamacardio.2019.1870. Erratum in: JAMA Cardiol. 2019 Nov 6;: PMID: 31215980; PMCID: PMC6584896 ↩︎
Haykal T, Samji V, Zayed Y, Gakhal I, Dhillon H, Kheiri B, Kerbage J, Veerapaneni V, Obeid M, Danish R, Bachuwa G. The role of vitamin D supplementation for primary prevention of cancer: a meta-analysis of randomized controlled trials. J Community Hosp Intern Med Perspect. 2019 Dec 14;9(6):480-488. DOI: 10.1080/20009666.2019.1701839. PMID: 32002154; PMCID: PMC6968692. ↩︎
Haykal T, Samji V, Zayed Y, Gakhal I, Dhillon H, Kheiri B, Kerbage J, Veerapaneni V, Obeid M, Danish R, Bachuwa G. The role of vitamin D supplementation for primary prevention of cancer: meta-analysis of randomized controlled trials. J Community Hosp Intern Med Perspect. 2019 Dec 14;9(6):480-488. DOI: 10.1080/20009666.2019.1701839. PMID: 32002154; PMCID: PMC6968692. ↩︎