Support us:
- Support you by Becoming a YouTube member (Click here).
- Premium Membership- Download PDF version of Notes, Get ad free video and more
- Consultant Membership- Above plus Download Powerpoint presentation of the notes and get access to EndoAI for Free
- Support us by purchasing our book - Click here for more details:
-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
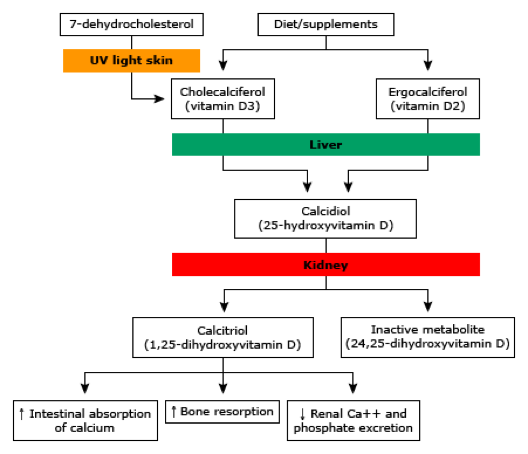
Q. Give the pathway for vitamin D synthesis?
-
Q. Which are the precursors of Vitamin D?
-
Q. What happens to the vitamin D precursors in the presence of light?
- In the presence of light, the vitamin D precursors undergo photoisomerization to Previtamin D
- Previtamin D is an unstable compound and within 48 hours undergoes temperature-dependent molecular rearrangement to form Vitamin D
-
Q. Why can't excess sunlight produce excess Vitamin D?
-
- Apart from the formation of Vitamin D, the Previtamin D also isomerizes to inert compounds called Lumisterol and Tachysterol. This prevents all the previtamin D from converting to vitamin D
-
- The melanin in the skin darkens with sunlight reducing the penetration of UV rays and hence putting a brake on the first step of vitamin D synthesis dependent on the light
-
-
Q. What timing of sunlight helps vitamin D formation?
- 10-11 am to 2-3 pm
-
Q. What is the impact of sunlight exposure on Vitamin D levels?
- Sunlight exposure improves vitamin D level to about 4 ng/ml In children in summer with 30 min sunlight exposure with 15-30% of body surface area
- However, there is little increase in vitamin D in Winters
-
Q. What skin melanin category do Indians belong to?
- Category I- European skin
- Category VII- African skin
- Indians- Category- IV or V
-
Q. What are the primary dietary sources of vitamin D?
- Fortified Cereals
- Fortified dairy products
- Egg yolk
- Fish oil
-
Q. Why do vitamin D levels decline with aging?
- It is mainly due to reducing skin synthesis of vitamin D
-
Q. How is vitamin D transported?
- Vitamin D binding protein
-
Q. What is the half-life of 25 hydroxyvitamin D?
- 15 days
-
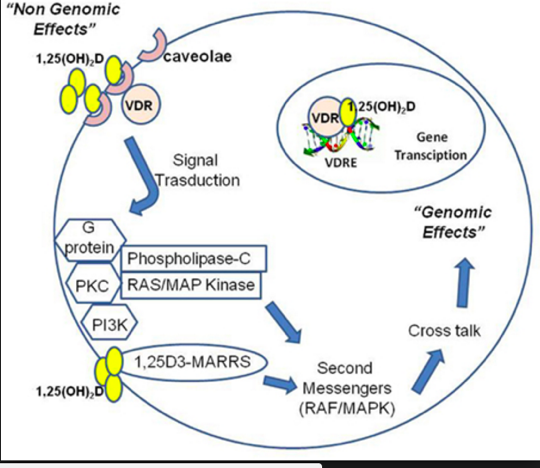
Q. What are the pathway for genomic and nongenomic actions of vitamin D?
-
Q. What are the names of plant and animal sources of vitamin D? Which is more potent?
- Plant- Ergocalciferol- vitamin D2
- Animal- Cholecalciferol- vitamin D3
- Both are equipotent
-
Q. Where does vitamin D after it is absorbed?
- Vitamin D is transported via a lymphatics
- it is bound to Vitamin D binding protein (VDBP)and Albumin while in circulation
- It goes to the liver, where it is converted to its storage form 25-Hydroxyvitamin D
-
Q. Apart from 25-Hydroxyvitamin D, what else binds to the Vitamin D binding protein (VDBP)?
- 1,25 Dihydroxyvitamin D also binds to the VDBP
-
Q. What happens to animal models having deficiency of Vitamin D binding protein (VDBP)?
- These mice have an increased tendency for toxicity due to 1,25 Dihydroxyvitamin D
- It also leads to Vitamin D Deficiency
-
Q. What does the polymorphism in the biding of Vitamin D binding protein (VDBP) produce?
- It leads to vitamin D deficiency in a specific subset of patients
-
Q. Which is the principal storage form of vitamin D, and what is its half-life?
- Storage form is 25-Hydroxyvitamin D
- Half-life is 15 days
-
Q. Give the definitions of vitamin D deficiency and insufficiency?
- Vitamin D levels
- Deficiency <20 ng/ml
- Insufficiency – 20-29 ng/ml
- Sufficiency – 30-100 ng/ml
- Toxicity – >150 ng/ml
- Vitamin D levels
-
Q. Give the cutoffs for vitamin D in nmol/l
- <30 nmol/l – inadequate
- 30-50- insufficiency
- 50-75- sufficiency
- 75-125- no benefit of replacement
- More than 125- toxicity
-
Q. Where do these levels for normality come from?
- They are based on when the PTH level rises
- Hence they are correlated with PTH level
-
Q. Which antitubercular drug reduces the 25 hydroxylations of vitamin D?
- Isoniazid
- This is because 25 hydroxylation of Vitamin D is a Cytochrome P450 like enzyme
-
Q. How does vitamin D reduce blood pressure?
- Vitamin D reduces renin and hence reduces the blood pressure
-
Q. What is megalin and what is its importance in vitamin D metabolism?
- Megalin is also called LRP2
- it is a type of receptor
- antibodies against megalin have been implicated in membranous nephropathy
- Vitamin D binding protein (VDBP) is filtered by glomeruli and reabsorbed by megalin
- Deficiency of megalin leads to loss of VDBP leading to severe Vitamin D Deficiency
- It is also thought to cause reuptake of 25-Hydroxyvitamin D from that filtered by the kidney
-
Q. Why is there Vitamin D Deficiency in nephrotic syndrome?
- In nephrotic syndrome also there is loss of Vitamin D binding protein (VDBP)
- This leads to deficiency of vitamin D
-
Q. Do 1,25 Dihydroxyvitamin D level impact 25-Hydroxyvitamin D levels?
- Yes
- Increased conversion to 1,25 Dihydroxyvitamin D leads to lower 25-Hydroxyvitamin D levels
#Updates : Notes from Williams Textbook of Endocrinology
-
-
Q. Which are the precursors of Vitamin D?
-
Q. What happens to the vitamin D precursors in the presence of light?
- In the presence of light, the vitamin D precursors undergo photoisomerization to Previtamin D
- Previtamin D is an unstable compound and within 48 hours undergoes temperature-dependent molecular rearrangement to form Vitamin D
-
Q. Why can't excess sunlight produce excess Vitamin D?
-
- Apart from the formation of Vitamin D, the Previtamin D also isomerizes to inert compounds called Lumisterol and Tachysterol. This prevents all the previtamin D from converting to vitamin D
-
- The melanin in the skin darkens with sunlight reducing the penetration of UV rays and hence putting a brake on the first step of vitamin D synthesis dependent on the light
-
-
Q. What is the half-life of active vitamin D, 1,25 Dihydroxyvitamin D ?
-
The half-life of this is 6-8 hours
-
-
Q. Where is the 1-alpha hydroxylase enzyme present?
- It is present in proximal convoluted tubule
- It is also a Cytochrome P450 enzyme
-
Ketoconazole can suppress this enzyme activity. Hence it can be used for the treatment of granulomatous disease-induced hypercalcemia #Clinicalpearl
-
Q. What is the critical difference between 25-hydroxylase and 1-alpha hydroxylase enzymes?
-
1-alpha is a more tightly regulated enzyme unline 25-hydroxylase #Clinicalpearl
-
-
Q. Which substances stimulate and which suppresses the enzyme?
-
Q. What is klotho ?
-
Q. Apart from the PCT of the kidney, where else is the 1-alpha hydroxylase enzyme expressed?
-
- Keratinocytes
-
- Placenta
-
- Granulomatous tissue
-
This is the reason why granulomatous disease like sarcoidosis and tuberculosis produce hypercalcemia #Clinicalpearl
-
-
Q. What produces this enzyme in granulomatous tissue?
- Macrophages produce this
- This is in response too Interferon gamma
- This is NOT regulated by routine regulators of 1-alpha hydroxylase like PTH etc
- Treatment with the following can suppress its production
-
Q. What is the benefit for the macrophage to produce this enzyme?
graph TD A[Macrophages from 1,25 Dihydroxyvitamin D] A --> B[Activate Vitamin D receptor] B --> C[Produce cathelicidin] C --> D[This has antimicrobial property] D --> E[Kills intracellular mycobacteria]
- Q. What is the role of the 24 hydroxylase enzyme?
- This converts 25 hydroxyvitamin D to 24,25 dihydroxyvitamin D
- This is an active form of hormone
- Deficiency of this enzyme can lead to hypercalcemia
-
Please consider donating to "Notes in Endocrinology" to keep us going. Please visit our DONATION page to know more