Support us:
- Support you by Becoming a YouTube member (Click here).
- Premium Membership- Download PDF version of Notes, Get ad free video and more
- Consultant Membership- Above plus Download Powerpoint presentation of the notes and get access to EndoAI for Free
- Support us by purchasing our book - Click here for more details:
-
Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
-
Associated notes:
-
Abbreviations:
- HPA axis = hypothalamic-pituitary–adrenal
-
Q. Which patients develop Exogenous Cushing syndrome?
- Patients taking Supraphysiological doses of Steroids for >3 weeks develop exogenous Cushing
-
Q. Apart from glucocorticoids which drugs can lead to Cushing's?
- Megestrol- a progesterone
- Medroxyprogesterone
- Fludrocortisone
-
- Cosmetic skin whiteners' may have glucocorticoids
-
Q. How is the diagnosis of Exogenous Cushing syndrome made?
- Low cortisol in the presence of Cushingoid symptoms
-
Q. What is the value of cortisol in exogenous Cushing's?
- 8 am cortisol < 3.6 ug/dl
-
Q. In which cases of exogenous Cushing can the 8:00 am cortisol be normal or high?
- Use of hydrocortisone- assay interference
- Use of ACTH
- Recovering from previous use of exogenous steroids
- Use of prednisone / prednisolone
-
Q. What are the causes of Normal or low 8:00 am cortisol despite endogenous Cushing's?
- Causes of normal or low baseline cortisol with endogenous Cushing syndrome
- Normocortisolemic Cushing's – Cortisol hyper-reactive syndrome
- Pituitary apoplexy
- bilateral macronodular adrenal hyperplasia (BMAH) with GIP responsive receptors
- Inactive phase of cyclical Cushing's
- Ketoconazole therapy inpatient with Cushing syndrome
- Causes of normal or low baseline cortisol with endogenous Cushing syndrome
-
Q. What will happen to ACTH in exogenous Cushing's?
- It will also be low
-
Q. Due to the use of exogenous glucocorticoids, what is the level at which suppression occurs?
- Suppression is mainly seen at the CRH level (Hypothalamus)
- Eventually, because of the lack of stimulation, the adrenal gland also undergo atrophy
-
Q. Why do patients on chronic Glucoritocid therapy fail ACTH stimulation even though the defect is at CRH level and at the level of adrenal cortex?
- Because of adrenal atrophy
-
Q. What are Factitious Cushing's and occult Cushing's?
- Factitious- patient secretly taking glucocorticoid without the knowledge of the physician
- Occult Cushing - a patient is taking Glucocorticoids without his/her knowledge
-
Q. Which agent used in AIDS cachexia is known to cause Cushing syndrome?
- Megesterol acetate (ENDACE, UNISTROL)
- Also medroxyprogesterone
-
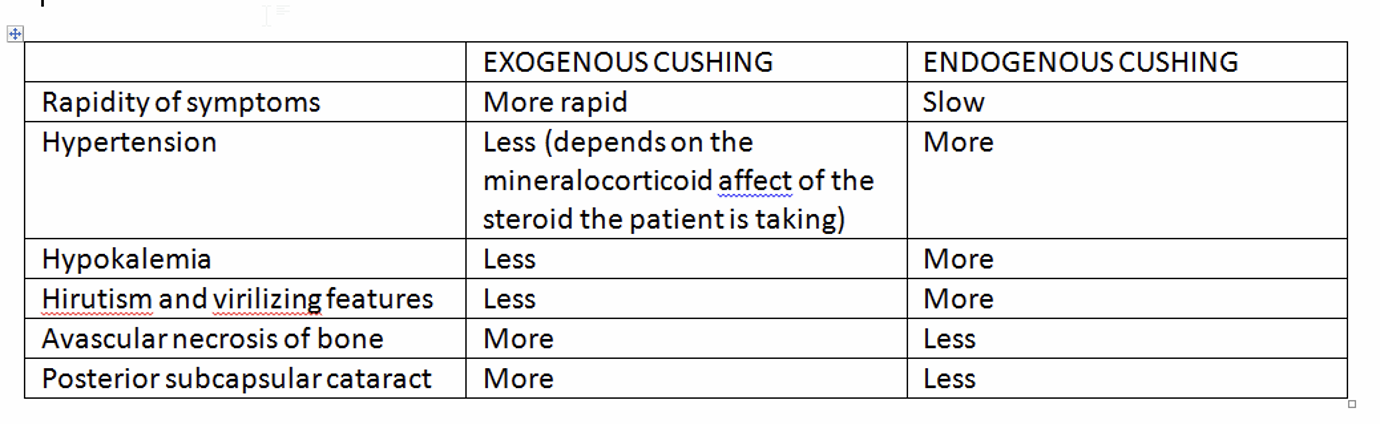
Q. What are the differences in clinical presentation between Exogenous and Endogenous Cushing's?
-
Q. Which clinical features are more common in Exogenous Cushing compared to endogenous Cushing's?
- Benign Raised ICT
- Osteonecrosis of femoral head
- Posterior subcapsular cataract
- Glaucoma
- Panniculitis
- Pancreatitis
- Spinal epidural lipomatosis
-
Q. Which clinical features as less common in exogenous Cushing's?
- Hypertension
- Hypokalemia
- Hirsustism and virilization
-
Q. What is the dreaded ocular complication with exogenous steroids?
- Glaucoma
-
Q. How is a diagnosis of Exogenous Cushing syndrome established?
- Presence of low morning serum cortisol and ACTH in the presence of Cushingoid symptoms
- Low DHEAS is also a practical test for looking at the health of the HPA axis in such patients. It is beneficial for the assessment of the recovery of the HPA axis
-
Q. Do exogenous Steroids interfere with endogenous assays?
- Yes
- Most do
- The exception is dexamethasone which does not interfere with the assay
- Prednisolone is more likely to interfere
- Glucocorticoid in question can directly be assayed but only in specialized labs
-
Q. What happens to ACTH stimulation test in Exogenous Cushing syndrome?
- There is atrophy of the adrenal cortex
- Hence there is less plasma cortisol response to ACTH
-
Q. What is Occult Cushing syndrome?
- Patient receives glucocorticoids without their knowledge leading to clinical features of Cushing syndrome
-
Q. Which mode of glucocorticoid therapy does not cause Cushing syndrome?
- There is no mode of therapy that does not cause Cushing
- All modes of glucocorticoids may cause Cushing syndrome
- However, it depends on the dose, duration, and many other factors
-
Q. Can hydrocortisone also cause Cushing's?
- Yes, If given in supraphysiological doses for a long time
-
Q. Which clinical features appear within hours of glucocorticoid administration?
- Insomnia
- Increased appetite and psychological manifestations
-
- Cushing syndrome has been described with Intra-articular, Inhaled, and Topical preparations also !!
-
Q. Which drugs used along with steroid increases the risk of Cushing's?
- Itraconazole and ritonavir
- They inhibit cytochrome p450 hence increasing the half-life of most steroids
-
Q. What is "steroid withdrawal syndrome"?
- Symptoms occurring because of steroids withdrawal even if the HPA axis is intact
-
- The dose and duration of steroids that can cause HPA axis suppression varies from individual to individual
-
Q. What is the typical duration of use of steroids that is known to cause HPA axis suppression?
- It is unknown
- Most people believe it is three weeks
- Some people believe that high doses can cause HPA axis suppression within five days
- Physiological doses can cause HPA axis suppression after one month
- HPA axis suppression may not in turn to adrenal insufficiency in all cases
- Patients receiving frequent short courses of steroids also have significant HPA axis suppression
-
Q. Which patients are more likely to have HPA axis suppression with glucocorticoids?
- Prednisolone > 20 mg for >3 weeks
- Prednisolone >5mg at night-time > 2 weeks
- Patient having clinical features of iatrogenic Cushing's
-
Q. What prednisolone dose cut-off is considered physiological as far as the HPA axis is concerned?
- It is believed Prednisolone dose of 7.5 mg of equivalent or less does not cause HPA suppression
- Dose equivalent to more than this can cause suppression
-
Q. What are the physiological doses of steroids described above?
- Hydrocortisone – 15-20 mg
- Prednisolone- 5-7.5 mg
-
Q. How long with tertiary adrenal insufficiency remain after steroid withdrawal in cases where the HPA axis is affected?
- They remain for a long time
- Often, for nine months after withdrawal of steroid
-
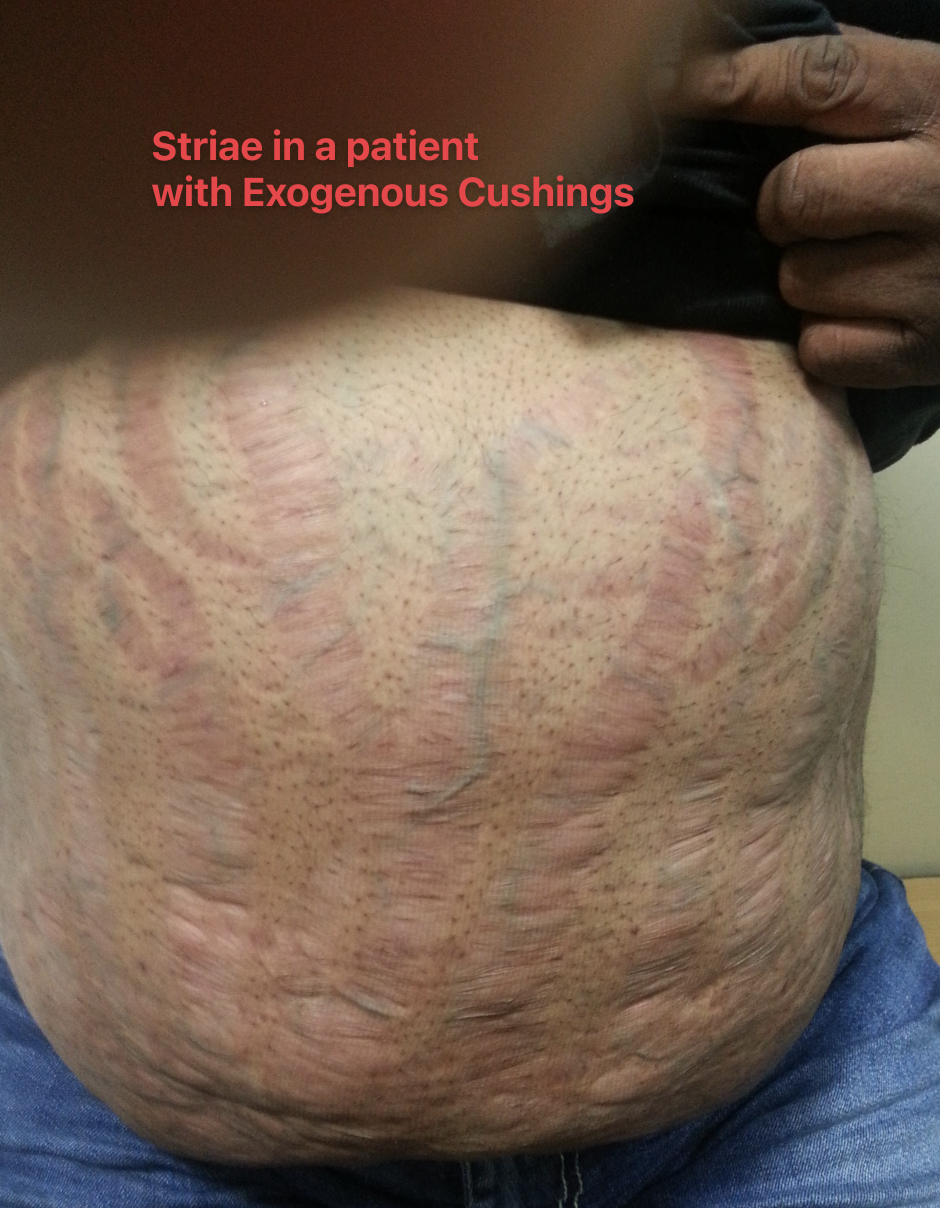
- This is a patient taking medications from a local quack for generalized weakness from a quack for a long time. When the patient came to us, he had features of Cushing syndrome. On evaluation, we found he was taking an injection of DEXAMETHASONE from a local quack (Patient permission taken for photographs)
-
Investigations:
- S. Cortisol - <1.0 mcg/dl
- DHEAS- 8.3 mcg/dl (lower limits of normal is 56 mcg/dl)
- ACTH <5.0 pg/ml
- Detailed video and discussion on Exogenous Cushing syndrome
Please consider donating to "Notes in Endocrinology" to keep us going. Please visit our DONATION page to know more