Support us:
- Support you by Becoming a YouTube member (Click here).
- Premium Membership- Download PDF version of Notes, Get ad free video and more
- Consultant Membership- Above plus Download Powerpoint presentation of the notes and get access to EndoAI for Free
- Support us by purchasing our book - Click here for more details:
- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Date: 09-Aug-2023
-
Source: Basics of Adrenal insufficiency - By Dr. Om J Lakhani
-
**Acute adrenal crisis **
-
Q. What is the volume status in primary vs secondary AI?
- Primary AI- volume deficit
- Secondary AI – Normal/ slightly increased volume status
- Hypotension occurs in both cases
- In primary AI it is Mineralocorticoid deficiency leading to volume depletion which is the cause
- In secondary AI → it is lack of pressor effect and lack of Epinephrine which is the cause
-
Q. Which is the preferred glucocorticoid in adrenal crisis?
- Hydrocortisone
-
Q. Is mineralocorticoid required during an acute adrenal crisis?
- Generally no
- This is because sodium retaining ability of fludrocortisone takes 2-3 days to appear
- Saline infusion solves the same purpose
- Hence Mineralocorticoid is unnecessary in acute adrenal crisis
-
Q. Describe the emergent treatment of adrenal crisis.
-
- Establish intravenous access with a large-gauge needle.
-
- Draw blood for immediate serum electrolytes and glucose and routine measurement of plasma cortisol and ACTH. Do not wait for lab results.
-
- Infuse 2 to 3 liters of isotonic saline or 5 percent dextrose in isotonic saline as quickly as possible. Frequent hemodynamic monitoring and measurement of serum electrolytes should be performed to avoid iatrogenic fluid overload.
-
- Give intravenous hydrocortisone, 100 mg immediately, and every six hours thereafter may be used.
-
- Use supportive measures as needed.
-
-
Q. What is the subsequent management?
-
- Continue intravenous isotonic saline at a slower rate for the next 24 to 48 hours.
-
- Search for and treat possible infectious precipitating causes of the adrenal crisis.
-
- Perform a short ACTH stimulation test to confirm the diagnosis of adrenal insufficiency, if the patient does not have known adrenal insufficiency.
-
- Determine the type of adrenal insufficiency and its cause if not already known.
-
- Taper parenteral glucocorticoid over one to three days, if precipitating or complicating illness permits, to an oral glucocorticoid maintenance dose.
-
- Begin mineralocorticoid replacement with fludrocortisone, 0.1 mg by mouth daily, when the saline infusion is stopped. (for Primary adrenal insufficiency)
-
-
Q. What type of fluid should be avoided during initial resuscitation of an acute adrenal crisis?
- Avoid hypotonic fluids as they can worsen the hyponatremia
-
CHRONIC ADRENAL INSUFFICIENCY
-
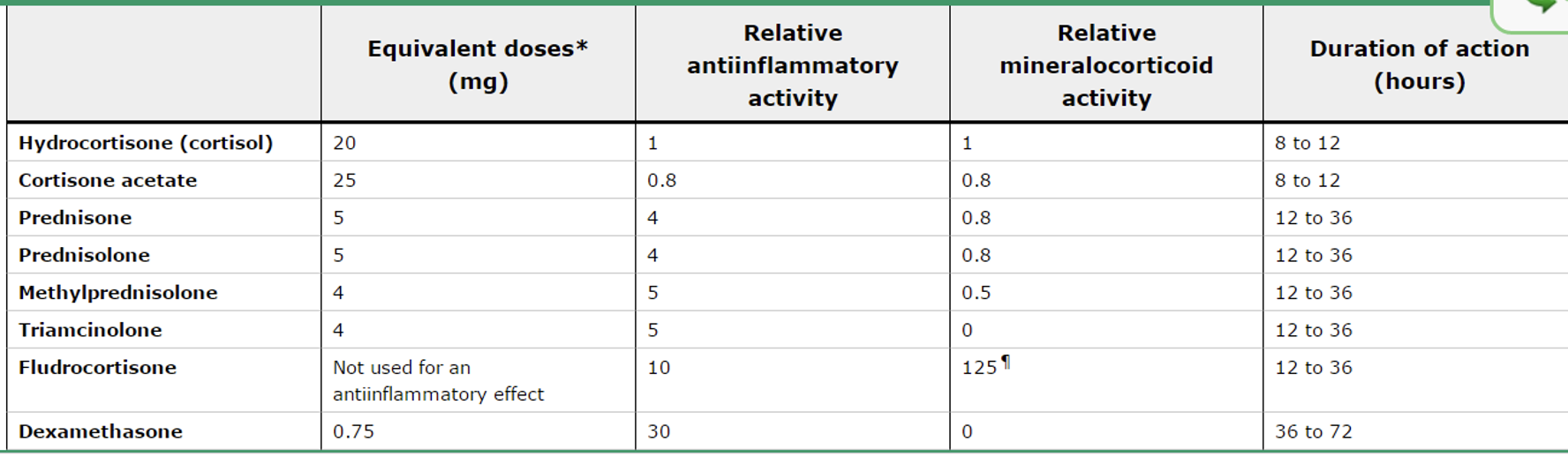
Q. Give the relative potency of various Glucocorticoid preparations.
-
Q. What should be the dose of Hydrocortisone per day based on /m2 (useful for children)?
- 10-12 mg/m2
-
Q. What are the doses used if longer-acting preparations are used?
- Dexamethasone – 0.5 mg
- Prednisolone – 5 mg
-
Q. What do endocrine society guidelines say about the choice of agent?
- Prefer- hydrocortisone or cortisone
- Prednisolone- alternate
- Avoid dexamethasone – cushingoid side effects are often seen
-
Q. What are the problems with long-acting agents?
- Tendency for overtreatment
- Also they tend to produce more BMD loss
-
Q. In which cases are longer-acting preps preferred?
- Patient noncompliant with treatment with multiple daily doses
- Patient has late evening or early morning symptoms
-
Q. Which drugs increase the requirement of Glucocorticoids?
- Drugs that increase the CYP3A4 enzyme activity
- These are
- Rifampicin
- Phenytoin
- Barbiturates
-
**MONITORING TREATMENT WITH HYDROCORTISONE **
-
Q. What is the best method to monitor treatment?
- Treatment should be monitored clinically
- Cortisol day curve may be useful
-
Q. When are samples taken to make a cortisol day curve?
- Blood sample on arrival – noting the time
- Before the lunchtime dose
- 1 hr after lunchtime dose
- Before the evening dose
- 1 hr after the evening dose or 6 pm
-
Q. What is the interpretation of the cortisol day curve?
- Peak and trough
- Peak <32 ug/dl and trough > 3.6 ug/dl
- Rough guide to normal values
- Morning peak – 18-28 ug/dl
- Lunchtime peak cortisol- 14 – 18 ug/dl
- Evening post-dose- 10-14 ug/dl
- Peak and trough
-
Q. Is there a simpler way to monitor apart from using a day curve?
- One paper suggests to measure Cortisol 4 hr after the morning hydrocortisone dose
- The value should be within 10-90th percentile of the nomogram that they have created
-
Q. What is Plenadren ?
- It is dual release hydrocortisone
- It has an immediate release outer cover and slowly extended release core
-
Q. How is it taken?
- It is taken as one tablet in the morning
-
Q. What are the advantages of Plenadren?
- In one study the patients had better metabolic parameters- Lower BMI, HbA1c, weight gain, and blood pressure
-
Q. What is the diavantage of Plenadren ?
- Provides a very long period of almost no cortisol
- Starting from evening time till morning there is negligible cortisol cover
-
Q. What is Chronocort?
- Chronocort is designed to have an early morning 4:00 am raise of cortisol which is what is physiologically seen
- The patient takes 20 mg at bedtime and 10 mg in the morning at 7:00 am
-
Q. Does the Dose of Fludrocortisone dependent on which steroid is taken?
- With Hydrocortisone- 0.05 mg is sufficient
- With Dexamethasone- 0.2 mg may be required
-
Q. How does the environment affect the Floudrocortisone dose?
- Dose must be increased in summer along with liberal salt intake
-
Q. How is monitoring done with the patient on Florinef?
- Supine and standing BP
- Serum potassium
- Plasma renin activity
-
Q. Which suggests a reduction of Fludrocortisone dose?
- Edema
- Hypertension
- Hypokalemia
-
Q. What are the criteria suggesting normal Fludrocortisone replacement?
- No Orthostatic hypotension or tachycardia
- Normal supine and standing BP
- Normal potassium
- Normal or slightly suppressed renin
-
Q. What PRA level should be targeted?
- PRA in the range of 1-4 ng/ml/hr (seated)
- Upper limit of the normal range
-
Q. PRA monitoring is useful in which patients?
- Annual PRA must be done in
- Patients with symptoms due to Mineralocorticoid deficiency
- Newly diagnosed AI with unstable doses of Fludrocortisone
-
Q. What are the symptoms of Mild Mineralocorticoid deficiency?
- Nausea – mild
- Salt craving
-
Q. A patient is asymptomatic on Fludrocortisone of 100 mcg and potassium is normal. PRA is done which is 5 ng/ml/hr. Should the dose of Fludrocortisone be increased?
- No
- Do not increase the dose of Fludrocortisone if patient is asymptomatic
- Clinical parameters should precede judgment based on PRA levels
-
Q. A patient on Fludrocortisone develops hypertension. What should be done?
- Reduce the dose of Fludrocortisone
- If the patient continues to remain hypertensive – then it could be essential hypertension- add antihypertensive- except Spironolactone
-
Q. What is the dose and benefit of the use of DHEA in Adrenal insufficiency?
- It is used in a dose of 50 mg /day
- It is thought to improve the quality of life in women
- In women who report reduced quality of life despite being on Glucocorticoid and Mineralocorticoid may be given DHEA trial for 6 months
- Endocrine Society also recommends this trial
-
Q. How is a dose of DHEA titrated?
- Based on the Morning DHEA-S level before the medications
- It should be targeted to mid normal range
-
Q. Why do patients with secondary Adrenal insufficiency develop Cortisol deficiency on starting GH?
- GH suppresses 11 beta HSD1 activity which converts cortisone to cortisol
-
Q. What is 3 x 3 rule ?
- In patients with AI, if they have a minor illness they can triple their dose of glucocorticoid for 3 days
- This is 3 x 3 rule
- If it fails to improve in 3 days then they need to consult a doctor
-
Q. What is the dose of glucocorticoids that must be used during surgery?
- Minor surgery – 25 mg of Hydrocortisone on the day of surgery
- Moderate surgical stress (eg: cholecystectomy) – 50-75 mg on the day of surgery and post-op day 1
- Major surgery – 100-150 mg on the day or surgery and ½ dose on the post of days 2 and 3- then return to baseline dose
-
Q. What emergency injectable Glucocorticoid must be prescribed to the patient?
- Hydrocortisone 100 mg or Dexamethasone 4 mg must be prescribed to the patient and the patient’s relatives must be taught how to inject it in case of emergency
-
Q. When should a family member inject hydrocortisone?
- Injury leading to blood loss of more than 1 cup
- Fracture
- Patient unresponsive
- Severe nausea and vomiting
- Symptoms of acute adrenal insufficiency
- In these cases- they must inject the drug and seek medical help immediately
-
Q. What is the dose of glucocorticoid required in women who are pregnant?
- Same dose as they were taking before pregnancy
- May increase the dose in 3rd Trimester
-
Q. What is the management during labor?
- 25 mg / 6 hrly during labor
- 100 mg /6hrly during delivery or infusion during delivery
- Taper to the previous dose in 2-3 days
-
Q. What is the effect of Progesterone on the RAAS axis?
- Progesterone competes with aldosterone for binding to Mineralocorticoid receptor
- Hence it causes a mild natriuretic effect
-
Q. Overall, what happens to aldosterone and renin in pregnancy?
- Aldosterone and renin increase during normal pregnancy
-
Q. How is fludrocortisone dose adjusted in pregnancy?
- PRA may guide therapy
- However do not try to suppress to pre-pregnancy range
-
Q. What do quality of life studies and prognosis says for patients with Adrenal insufficiency?
- They say the quality of life is worse with PAI despite optimal therapy
- Mortality may be increased but data is uncertain
-
- Fludrocortisone has a long half-life and can even be given on alternate days
-
Q. Which form of Hydrocortisone is preferred for an emergency?
- Hydrocortisone hemisuccinate
-
Q. What dose of hydrocortisone eliminates the need for Fludrocortisone?
- Hydrocortisone >40 mg has enough Mineralocorticoid activity
- Eliminates the need for fludrocortisone
-
- Low normal or subnormal ACTH may suggest overtreatment in primary adrenal insufficiency!
-
**Sick Day rules **
-
Q. What is the first sick day rule for Adrenal insufficiency
- Double the dose of steroids in following cases:
-
- Fever with Temp >37.5 C
-
- Any illness requiring bed rest
-
- Any infection requiring antibiotics
-
- Vomiting or diarrhea but able to tolerate food and liquids
-
- Double the dose of steroids in following cases:
-
Q. Till how long to continue double the dose?
- Till the patient is better from the underlying disease
-
Q. In which cases is parenteral hydrocortisone required?
-
- The patient is having very severe illness requiring hospitalization
-
- The patient is NPO for surgery or some other reasons
-
- Loss of consciousness/collapse of the patient
-
- Persistent vomiting and diarrhea which cause oral medication cannot be taken
-
-
Q. What is done for minor surgical procedures?
- Double the dose of steroid on the day prior or the morning or the procedure
- Taking 100 mg Hydrocortisone IM/IV 30 minutes before the procedure