Diagnosis Of Adrenal Insufficiency
Author: Dr. Om J Lakhani
If you find this useful, please use the link to see the various ways in which you can Support us →
ESTABLISHING THE DIAGNOSIS
-
Q. What morning cortisol value should be used for the diagnosis of Primary adrenal insufficiency [PAI]?
- < 5 mcg/dl – 100% specificity but less sensitivity
- This is the cutoff recommended by the Endocrine society
- However, a value of <3 ug/dl is suggested by other experts
-
Q. What upper limit of cortisol value rules out adrenal insufficiency?
- This is debatable
- Some say 10.8 ug/dl and some say 17 ug/dl
- However, the upper limit should not be used for diagnostic consideration
-
Q. Can morning salivary cortisol be used for diagnosis?
- Yes, but it has not been validated
- Value <1.8 ng/ml - most likely adrenal insufficiency is present
- Value >5.8 ng/ml – rules out
-
Q. Does 4 pm cortisol have any value?
- No
-
Q. Is Cosyntropin a complete ACTH molecule?
- No
- It is ACTH – 1-24 amino acids
- Normal ACTH is 1-39 amino acids
- However, it has full biological potency
-
Q. Is it necessary to perform ACTH stimulation in the morning?
- No
- However, normal people have the highest cortisol response in the morning
- Hence, doing the test in the morning would improve specificity and avoid false positives
-
Q. How is the low dose ACTH stimulation test performed?
- Get baseline cortisol first – no further testing required in the following conditions
- S. Cortisol <3.6 ug/dl - Definitely low (NEW ENDOCRINE SOCIETY GUIDELINES)
- S. cortisol >15 ug/dl - Definitely normal
- For Baseline cortisol 3 - 15 ug/dl perform Low dose ACTH stimulation test
- Give 1 ug of Cosyntropin IV – 1 unit in 100 IU insulin syringe
- Insulin syringe can be used for this purpose
- 250 ug (2ml) of Cosyntropin is diluted in 250 ml of normal saline, giving a ratio of 1 ug/ml
- Take 1 ml of this in an insulin syringe (alternatively, dilute in 500 ml of normal saline and take 2 ml in a normal 5 cc syringe)
- 1 ml (1ug/ml dilution) is injected IV
- Repeat Cortisol after 20 and 30 min
- If peak cortisol >21.7 ug/dl – then suggestive of normal response (18 ug/dl according to Endocrine society guidelines)
- Give 1 ug of Cosyntropin IV – 1 unit in 100 IU insulin syringe
- Get baseline cortisol first – no further testing required in the following conditions
-
Q. Why is cortisol collected at 20 min also in low dose ACTH stimulation?
- Because the peak may be achieved earlier
-
Q. In which conditions is the low dose ACTH stimulation test useful?
- Recent secondary Adrenal insufficiency - e.g., after pituitary surgery - within 1-2 weeks (< 4 months of Pituitary surgery)
- Chronic partial pituitary AI
-
Q. When should the 250 ug dose ACTH stimulation be performed after pituitary surgery?
- It is reliable 4 months after pituitary surgery
- Or 9 months after radiation therapy
ESTABLISHING THE LEVEL OF DEFECT
-
Q. What is the lab method for testing of ACTH?
- 2 site chemiluminescent assay
-
Q. What is the normal value of ACTH using the 2 site chemiluminescent assay?
- It is 20-52 pg/ml
-
Q. What ACTH value favors primary and what favors secondary adrenal insufficiency?
- More than 100 pg/ml - primary
- <20 pg/ml - Secondary adrenal insufficiency
- 20-100 pg/ml - gray zone
-
Q. When should the ACTH sample be drawn?
- Ideally, before the treatment is started
- However, if treatment is already started, then 24 hours after the last dose of hydrocortisone and a longer duration after the last dose of dexamethasone
- Alternatively, switch to hydrocortisone from dexamethasone for several days before measuring ACTH if dexamethasone is used
-
Q. What is the principle of a prolonged ACTH stimulation test?
- Atrophic adrenal glands in secondary and tertiary AI may not respond to a single ACTH stimulation but may respond to a prolonged ACTH stimulation test
- While in primary AI – they don't respond to prolonged ACTH stimulation
- Hence, it helps distinguish primary from secondary/tertiary AI
-
Q. What is the principle of the Metyrapone test?
- Metyrapone blocks 11 beta hydroxylase, reducing Cortisol further → stimulates ACTH → increase of 11 deoxycortisol
-
Q. What is the use of the metyrapone stimulation test?
- It is used for the diagnosis of partial ACTH deficiency, which may be missed with ACTH stimulation or even ITT
-
Q. Why does the metyrapone stimulation detect partial ACTH deficiency, which is missed by ITT?
- Hypoglycemia is a more potent stimulant for ACTH release than hypocortisolemia
- Hence, ITT may lead to a normal response in patients with partial ACTH defect
-
Q. What is the use of the CRH Stimulation test?
- It is used to differentiate secondary from tertiary AI
- ACTH increases in response to CRH in tertiary AI, while it does not in secondary AI
-
Q. Is the insulin tolerance test really required to make the diagnosis of AI?
- Generally no, unless it is also done to test for GH deficiency or in a very recent ACTH defect
-
Q. So which test to use in secondary AI?
- Chronic secondary AI - high dose ACTH stimulation test (4 months after pituitary surgery)
- Acute secondary AI - Low dose ACTH stimulation test / ITT
- Partial ACTH deficiency – Metyrapone stimulation test
USE OF ACTH STIMULATION TESTS FOR DIAGNOSIS OF ADRENAL INSUFFICIENCY
-
Q. Can Cosyntropin for a low dose be given IM?
- No
- For the full dose, both IM and IV are possible
- For a low dose, IM has not been evaluated
-
Q. Is 1mg the standard dose for Low dose ACTH stimulation, or can a lower dose be used?
- 0.5 mg/1.73 m2 has also been tested
-
Q. How is the solution for 1 ug/ml made?
- a. Take 0.2 ml of Cosyntropin 250 ug/ml with a Tuberculin/insulin syringe (0.2 ml will be 20 units in an insulin syringe of 100 IU)
- b. This is injected into 25 ml of normal saline – this makes it a solution of 2 ug/ml
- c. 0.5ml of this solution is taken and shaken thoroughly and injected IV using the same syringe
-
Q. What cut off must be used if the IM injection of Cosyntropin is used instead of IV?
- One paper suggests a lower cut off of 16 ug/dl instead of 18 ug/dl for the high dose ACTH stimulation test used IM instead of IV
-
Q. Summarize the role of various tests in the diagnosis of Adrenal insufficiency?
- 250 mcg ACTH stimulation test-
- Diagnosis of Primary AI
- Diagnosis of Secondary AI > 4 months after pituitary surgery
- 1 mcg ACTH stimulation test
- Diagnosis of PAI (same sensitivity as 250 mcg)
- Diagnosis of Acute ACTH deficiency (SAI) <4 months after surgery
- Prolonged ACTH stimulation test - Differentiate Primary from Secondary AI
- Metyrapone stimulation test - Diagnosis of partial ACTH deficiency
- CRH stimulation test - distinguish secondary and tertiary AI
- Insulin tolerance test - gold standard - used to evaluate the entire HPA axis
- 250 mcg ACTH stimulation test-
-
Q. What are the precautions taken before using the metyrapone stimulation test?
- Must be done in an indoor setup as it leads to further reduction of cortisol
- Leads to nausea and vomiting - avoid in patients with severe AI
-
Q. How is the metyrapone stimulation test performed?
- Earlier it was performed over 3 days
- Now it is done overnight
- Metyrapone 30 mg/kg (750 mg) is given at midnight
- ACTH, Cortisol, and 11 deoxycortisol are measured at 8:00 am in the morning
-
Q. What is the normal response?
- Normal values
- ACTH >100 pg/ml
- 11 deoxycortisol - > 7 ug/dl
- Cortisol < 5 ug/dl
- Normal values
-
Q. What suggests adrenal insufficiency?
- 11 Deoxycortisol < 7 ug/dl
- Cortisol < 5 ug/dl
- This is diagnostic of PAI
-
Q. What is the importance of the ACTH value in the metyrapone stimulation test?
- It can help differentiate primary from secondary AI
- However, the values overlap with normal individuals, hence it cannot be used if the patient is not established to have AI
- In Partial Secondary AI – ACTH value is 10-200 pg/ml
- In PAI - >200 pg/ml
-
Q. Can a conventional Immunoassay be used in this test?
- No, it cannot be used because cortisol and 11 Deoxycortisol may cross-react
- Hence, it is better to use LC-MS/MS
-
Q. Can this test be used in Cushing's syndrome?
- Yes
- It can be used to distinguish Pituitary from Ectopic Cushing's
-
Q. How does it help in ACTH-dependent Cushing's?
- In Ectopic Cushing's – the natural HPA Axis is suppressed - hence there is a negative response (failure of 11 Deoxycortisol to raise) to Metyrapone
- In Pituitary Cushing's - ACTH increases, hence it responds
-
Q. Can DHEAS be used to make a diagnosis of adrenal insufficiency?
- Yes
- DHEAS <60 ug/dl goes in favor of adrenal insufficiency
- Also, in patients with secondary adrenal insufficiency early - the DHEAS response to low dose ACTH is lost first before the cortisol response
- Hence, stimulated DHEAS can be used for early diagnosis of secondary AI
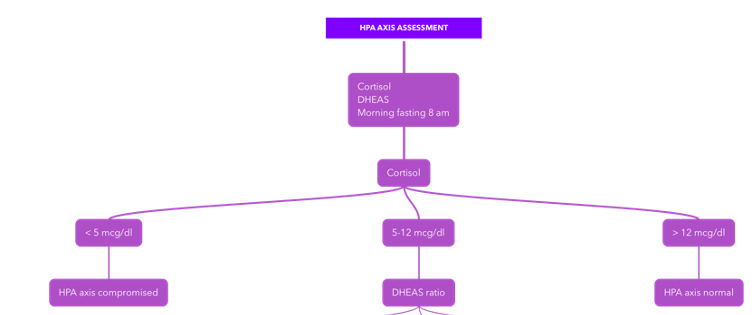
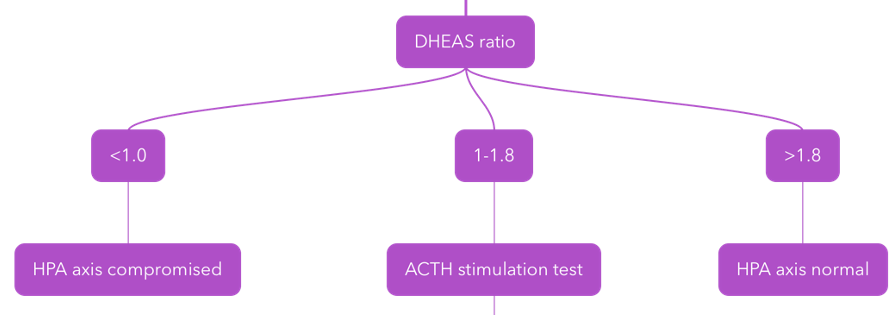
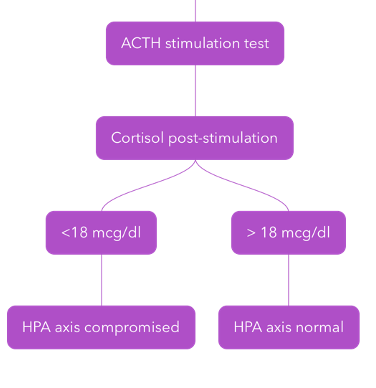
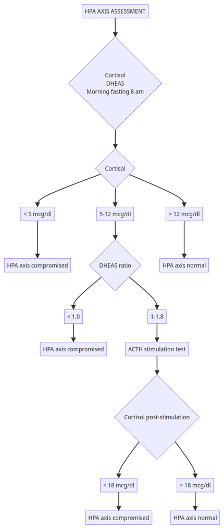
Updates, 03-Aug-2023
- Q. What is Dr. Om J Lakhani's protocol for the diagnosis of Adrenal insufficiency?
- Step 1:
- Step 2:
- Step 3:
- All Steps in one:
- Step 1:
UPDATES - 06-Jan-2024
-
Q. What is the role of the low dose ACTH stimulation test done using ACTON Prolongatum (Porcine sequence corticotropin)?
- A study conducted by Appaiah et al found that the use of a low dose of ACTON prolongatum in the dose of 6 units achieves the same objective as a higher dose (24 units) of the same
-
Q. What is the new protocol for the ACTH stimulation test as suggested in the paper?
- Take a baseline cortisol sample
- Administer 6 units of ACTON Prolongatum (Porcine sequence corticotropin) intramuscularly
- Take samples for the Cortisol at 30 and 60 minutes
- Use the same cut-off >18 mcg/dl as suggested earlier
UPDATES - 31-December-25
DHEAS for Diagnosis of Adrenal Insufficiency
Adrenal Insufficiency Diagnostic Calculator using DHEAS based on Han Suresh et al
References:
- Appaiah, Sonali; Shivanappanavar, Vishwanath; George, Belinda; Bantwal, Ganapathi; Ayyar, Vageesh. A Comparison of Lower Doses of Porcine Sequence Corticotropin with Standard Dose in Testing the Hypothalamic Pituitary Adrenal Axis in Healthy Individuals. Indian Journal of Endocrinology and Metabolism 27(5):p 421-425, Sep–Oct 2023. | DOI: 10.4103/ijem.ijem_56_23
- Han AJ, Suresh M, Gruber LM, Algeciras-Schimnich A, Achenbach SJ, Atkinson EJ, et al. Performance of Dehydroepiandrosterone Sulfate and Baseline Cortisol in Assessing Adrenal Insufficiency. J Clin Endocrinol Metab. 2024;00:1–8. doi:10.1210/clinem/dgae855.