- Credits
- Section Writer: Dr. Om J Lakhani
- Section Editor: Dr. Om J Lakhani
Support us:
- Support you by Becoming a YouTube member (Click here).
- Premium Membership- Download PDF version of Notes, Get ad free video and more
- Consultant Membership- Above plus Download Powerpoint presentation of the notes and get access to EndoAI for Free
- Support us by purchasing our book - Click here for more details:
- Q. What are the different non-systemic way of glucocorticoid administration ?
- Topical Application: This involves applying glucocorticoid creams or ointments directly to the skin to treat conditions like eczema, psoriasis, and dermatitis. The medication acts locally on the skin without significant absorption into the bloodstream.
- Inhalation: Inhaled glucocorticoids are commonly used in the management of asthma and chronic obstructive pulmonary disease (COPD). Medications are delivered directly to the lungs through an inhaler or nebulizer, minimizing systemic exposure.
- Intra-Articular Injection: For conditions like arthritis, glucocorticoids can be injected directly into a joint. This localizes the effect to the joint, reducing inflammation and pain with minimal systemic impact.
- Intranasal Spray: Glucocorticoids in the form of a nasal spray are used for treating allergic rhinitis and nasal polyps. The medication acts on the nasal mucosa to reduce inflammation.
- Ophthalmic Application: Glucocorticoid eye drops or ointments are used to treat various inflammatory conditions of the eye, such as uveitis or conjunctivitis.
- Q. What is the other name for non-systemic glucorticoid use ?
- It is called compartmental glucorticoid administration
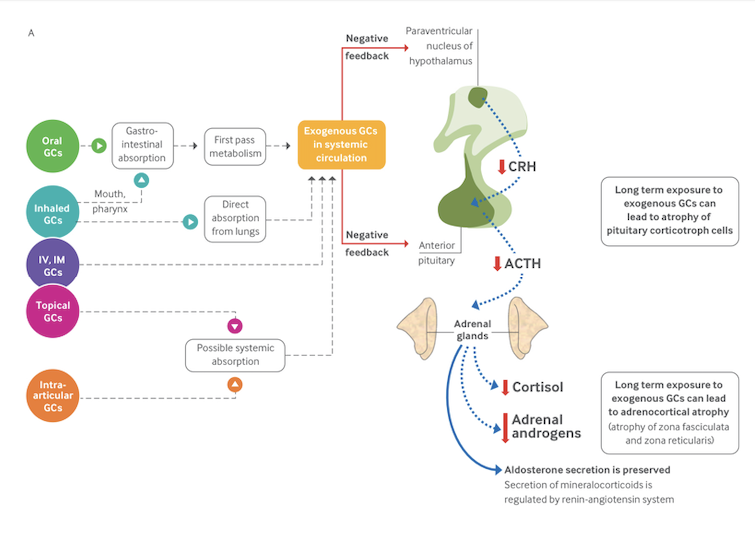
- Q. With a diagram, show a summary of how various glucorticoids can lead to HPA axis suppression ?
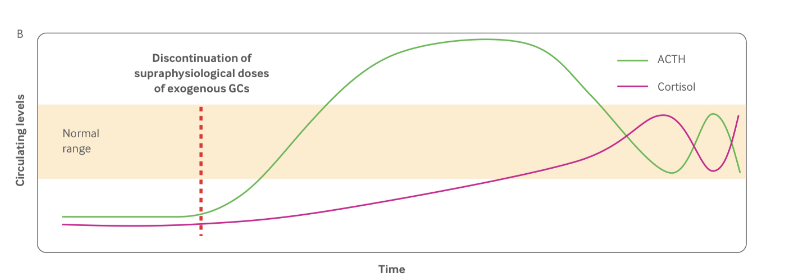
- Q. After withdrawal of glucorticoids- which hormone recovers first ?
- ACTH and CRH recover first
- The adrenal cortex often atrophies and takes time for the cortisol production to recover
- Q. Which are the flourinated and nonflourinated glucorticoids and what are the difference between them ?
-
Fluorinated Glucocorticoids
- Examples:
- Dexamethasone
- Betamethasone
- Triamcinolone
- Fludrocortisone
- Characteristics:
- Contain fluorine atoms in their molecular structure.
- Tend to have a longer duration of action.
- Generally more potent compared to non-fluorinated glucocorticoids.
- Have a higher risk of causing certain side effects, such as fluid retention and increased blood pressure.
- Examples:
-
Non-Fluorinated Glucocorticoids
- Examples:
- Hydrocortisone (Cortisol)
- Prednisone
- Methylprednisolone
- Cortisone
- Characteristics:
- Lack fluorine atoms in their molecular structure.
- Usually have a shorter duration of action compared to fluorinated glucocorticoids.
- Generally less potent, requiring higher doses to achieve the same effect as fluorinated glucocorticoids.
- Tend to have a lower risk of certain side effects like fluid retention and hypertension, but this can vary depending on the specific drug and dosage.
- Examples:
-
- Q. What are the factors that increase or reduce the risk of Adrenal insufficiency with systemic glucorticoid use (Oral, Intravenous, intramuscular) ?
- Factors increasing the risk of GI-Al:
- Dailv administration for ›2-4 weeks
- Multiple daily split doses
- Bedtime administration
- Factors reducing the risk of GI-Al:
- Alternate day administration
- Pulse systemic therapy (intermittent intravenous administration of very high doses of glucocorticoids over a few days orweeks)
- Factors increasing the risk of GI-Al:
- Q. Use of what concomitant drugs increase or reduce the risk of adrenal insufficiency due to systemic glucorticoid use ?
- CYP3A4 inhibitors
- CYP3A4 is the major pathway for the inactivation of most prescribed glucocorticoids. CYP3A4 inhibitors are expected to increase the systemic exposure to synthetic glucocorticoids
- Strong inhibitors: ceritinib, clarithromycin, cobicistat, darunavir, idelalisib, indinavir, itraconazole, ketoconazole, lopinavir, posaconazole, ritonavir, saquinavir, telaprevir, telithromycin, and voriconazole
- Moderate inhitors include amrodarone, aprepitant, cimetidine, convaptan, cazountd, cictosporn, antiazem, dronedarone, erythromycin, Fluconazole, rosamprenavir, rosaprepitant, grapetruit juice, imatinib, isavuconazole, netupitant, nilotinib, ribocicib, schisandra, and verapamil
- CYP3A4 inducers
- CYP3A4 inducers are expected to decrease the systemic exposure to synthetic glucocorticoids.
- Strong inducers include apalutamide, carbamazepine, enzalutamide, fosphenytoin, lumacaftor, lumacaftor-ivacaftor, mitotane, phenobarbital, phenytoin, primidone, and rifampicin
- Moderate inducers include bexarotene, bosentan, cenobamate, dabrafenib, efavirenz, elagolix/ estradiol/no rethindrone acetate combination, eslicarbazepine, etravirine, lorlatinib, modafinil, nafcillin, pexidartinib, rifabutin, rifapentine, and StJohn' wort (Hypericum pertoratum)
- CYP3A4 inhibitors
- Q. Which non-glucorticoid drugs can also lead to adrenal insufficiency ?
- Megesterol acetate
- High dose of Medroxyprogsterone acetate
- Q. Which glucocorticoids are not metabolised via CYP3A4 ?
- Beclometasone
- Flunisolide
- Q. Do children also have risk of adrenal suppression:
- Yes
- They very much do especially those with age <5 years
- However the recovery of the adrenal function is also faster
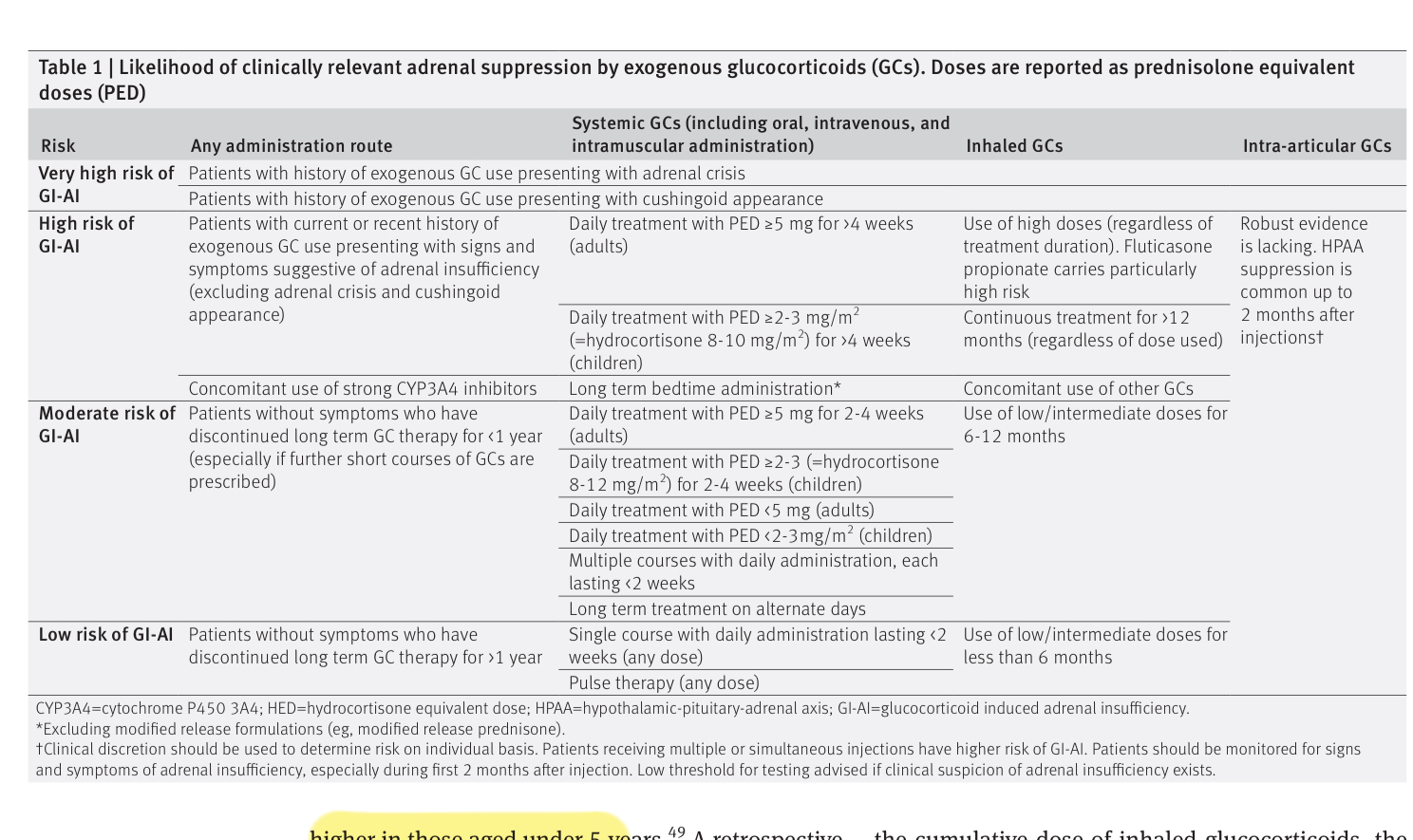
- Q. Enlist the conditions associated with very high, high , moderate and low risk of adrenal insufficiency with glucocorticoid use in systemic situations
- Very High Risk of GI-AI (Glucocorticoid-induced Adrenal Insufficiency)
- Patients with a history of exogenous GC use presenting with adrenal crisis.
- Patients with a history of exogenous GC use presenting with cushingoid appearance.
- High Risk of GI-AI
- Patients with current or recent history of exogenous GC use presenting with signs and symptoms suggestive of adrenal insufficiency (excluding adrenal crisis and cushingoid appearance).
- This risk category mentions a daily treatment with a prednisolone equivalent dose (PED) ≥ 5 mg for ≥4 weeks for adults.
- Daily treatment with PED ≥ 2-3 mg/m² for >4 weeks for children.
- Concomitant use of strong CYP3A4 inhibitors.
- Long term bedtime administration
- Moderate Risk of GI-AI
- Patients without symptoms who have discontinued long-term GC therapy for < 1 year, especially if further short courses of GCs are prescribed.
- Daily treatment with PED ≥ 5 mg for 2-4 weeks for adult
- Daily treatment with PED ≥ 2-3 mg/m² for 2-4 weeks for children
- Daily treatment with PED <5 mg (adults)
- Daily treatment with PED <2-3 mg/m2 (children)
- multiple courses with dailv administration. each lasting <2 weeks
- Long term treatment on alternate days
- Low Risk of GI-AI
- Patients without symptoms who have discontinued long-term GC therapy for >1 year.
- The low-risk category includes long-term treatment on alternate days, a single course with daily administration lasting < 2 weeks (any dose), and pulse therapy (any dose).
- Very High Risk of GI-AI (Glucocorticoid-induced Adrenal Insufficiency)
- Q. According to pediatric endocrine society, at what doses of oral corticosteroid use, should be consider possibility of a child having Adrenal insufficiency ?
- Children who have received supraphysiological doses of corticosteroids >8-12 mg/m2/day of hydrocortisone or greater for 2 weeks or more should be considered to have possibility of Adrenal insufficiency
- Q. What is total steroid load ?
- Patients with asthma often receive corticosteroids in different forms- inhaled, IV and oral and all aspects should be considered for evaluating adrenal insufficiency
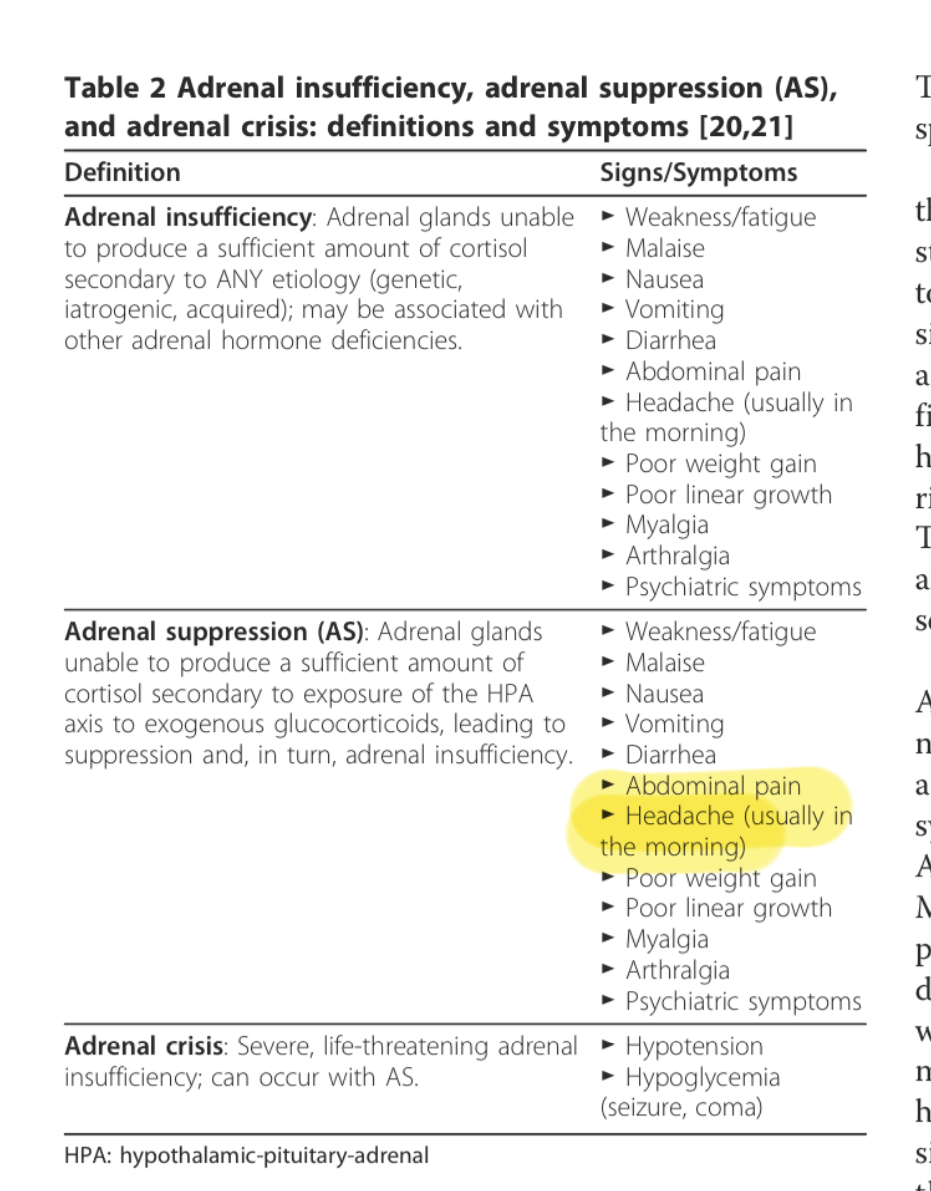
- Q. What are the symptoms of Adrenal insufficiency in children ?
- Q. True or false- standard High dose 250 mcg ACTH stimulation test is the the diagnosis of adrenal insufficiency due to exogenous glucocorticoids in children ?
- This is true
- It lack's sensitivity
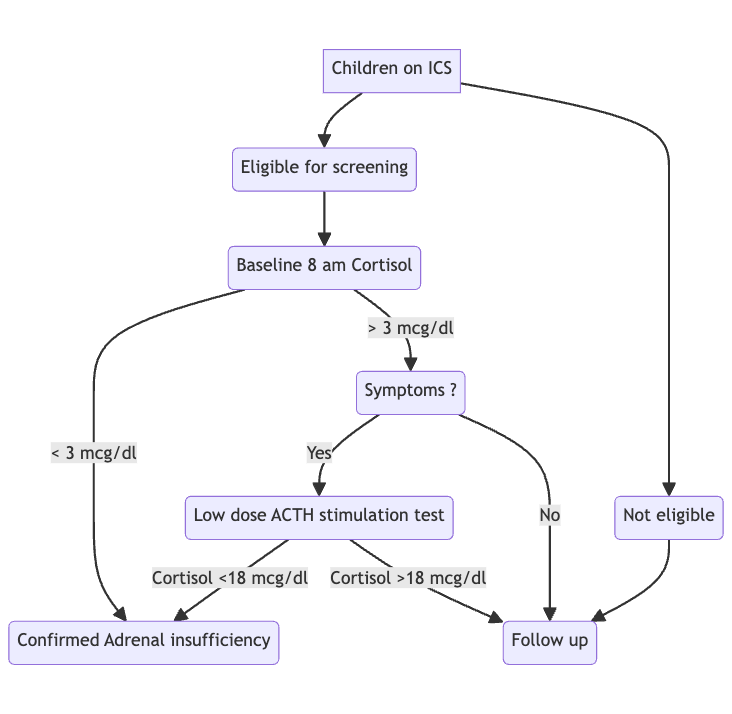
- Hence low dose ACTH stimulation test may be a better choice because of higher sensitivity
- Q. Is weight loss a sign of glucocorticoid deficiency or mineralocorticoid deficency ?
- Though it can be because of both , weight loss is definitely an important sign of mineralocorticoid defect in children
- Q. Can inhaled steroids produce growth retardardation in children ?
- Yes
- But poor asthma control can also lead to growth retardation
- Q. Give the brief about low dose ACTH stimulation test in children ?
- Ideally performed in morning fasting (unlike High dose ACTH stimulation which is done at anytime)
- 1 mcg of cosyntropin is given IV
- Serum cortisol is measured at
- 0
- 20 min
- 30 min
- Cortisol level <18 mcg/dl is considered abnormal
- This cut-off has sensitivity and specificity of 90%
- Q. Is baseline cortisol useful ?
- Yes
- Baseline 8 am cortisol is useful
- The cut-off of <5 mcg/dl is useful
- Inhaled corticosteroids
- Q. How common is adrenal insufficiency with the use of Inhaled corticosteroids overall ?
- The risk is 6.8% in patients on inhaled corticosteroids alone
- Q. Summarize the factors that increase the risk of adrenal suppression with inhaled corticosteroids
- High daily doses given for ›6-12 months
- Treatment with fluticasone propionate
- Concomitant use of oral glucocorticoids (including intermittent use-eg, in chronic obstructive pulmonary disease)
- Lower body mass index (children)
- Higher compliance with treatment (children)
- Q. Summarize the high, moderate and low risk of adrenal insufficiency with inhaled corticosteroid use ?
- Very High Risk of GI-AI (Glucocorticoid-induced Adrenal Insufficiency)
- Patients with a history of exogenous GC use presenting with adrenal crisis.
- Patients with a history of exogenous GC use presenting with cushingoid appearance.'
- High risk
- Use of high doses (regardless of treatment duration). Specifically, fluticasone propionate carries a particularly high risk.
- Continuous treatment for more than 1 year (regardless of the dose used).
- Concomitant use of strong CYP3A4 inhibitors.
- Concomitant use of other glucoroticoids
- Patients with current or recent history of exogenous GC use presenting with signs and symptoms suggestive of adrenal insufficiency (excluding adrenal crisis and cushingoid appearance).
- Moderate risk
- Low or intermediate doses for 6-12 months
- Low risk
- Low or intermediate doses for < 6 months
- Very High Risk of GI-AI (Glucocorticoid-induced Adrenal Insufficiency)
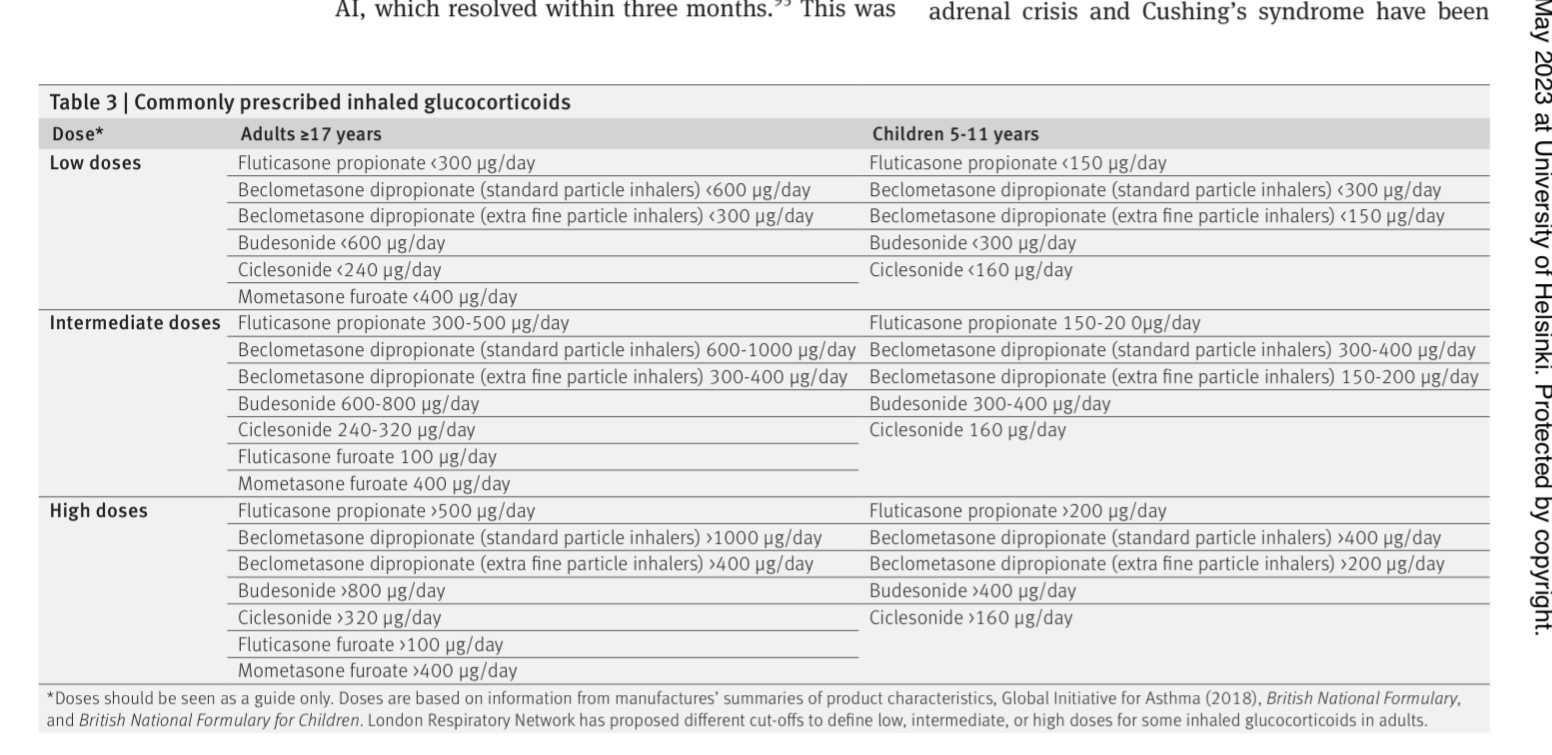
- Q. True or false, dose of Inhaled corticosteroids (ICS) in children with asthma is lower than that in adults ?
- Surprisingly no
- The dose of ICS for asthma in children is the same as that in adults
- Q. Summarize the doses and commonly prescribed inhaled corticosteroids ?
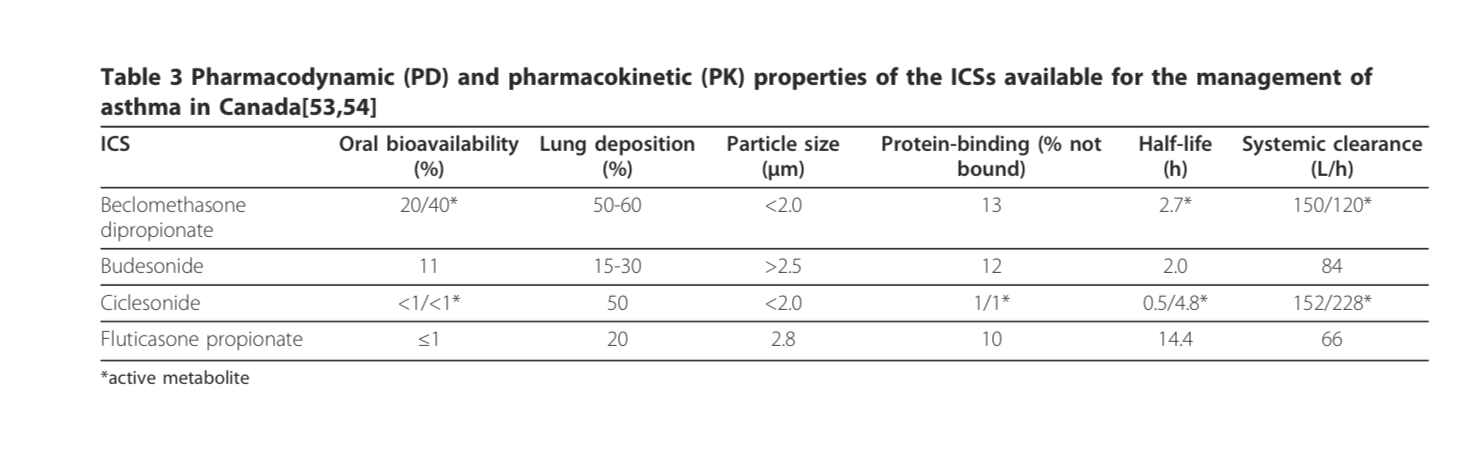
- Q. Describe the PK/PD of various inhaled corticosteroids
- Q. Describe the fate of inhaled corticosteroids when taken by the patient
- Approximately 10-60% of the administered ICS is deposited into the lungs upon inhalation.
- The ICS exerts its effect on inflamed tissue as soon as it dissolves into the pulmonary lining and binds to intracellular corticosteroid receptors.
- The remainder of the drug that does not get absorbed into the lung (40-90%) is deposited into the mouth and pharynx, where it has the potential to exert local side effects, such as oropharyngeal candidiasis and dysphonia.
- If not rinsed out of the mouth, this portion of the ICS dose may be swallowed and subsequently absorbed into the gastrointestinal (GI) tract.
- Drug that is absorbed from the GI tract and that escapes inactivation by first-pass metabolism in the liver enters the systemic circulation unchanged, potentially causing serious systemic side effects.
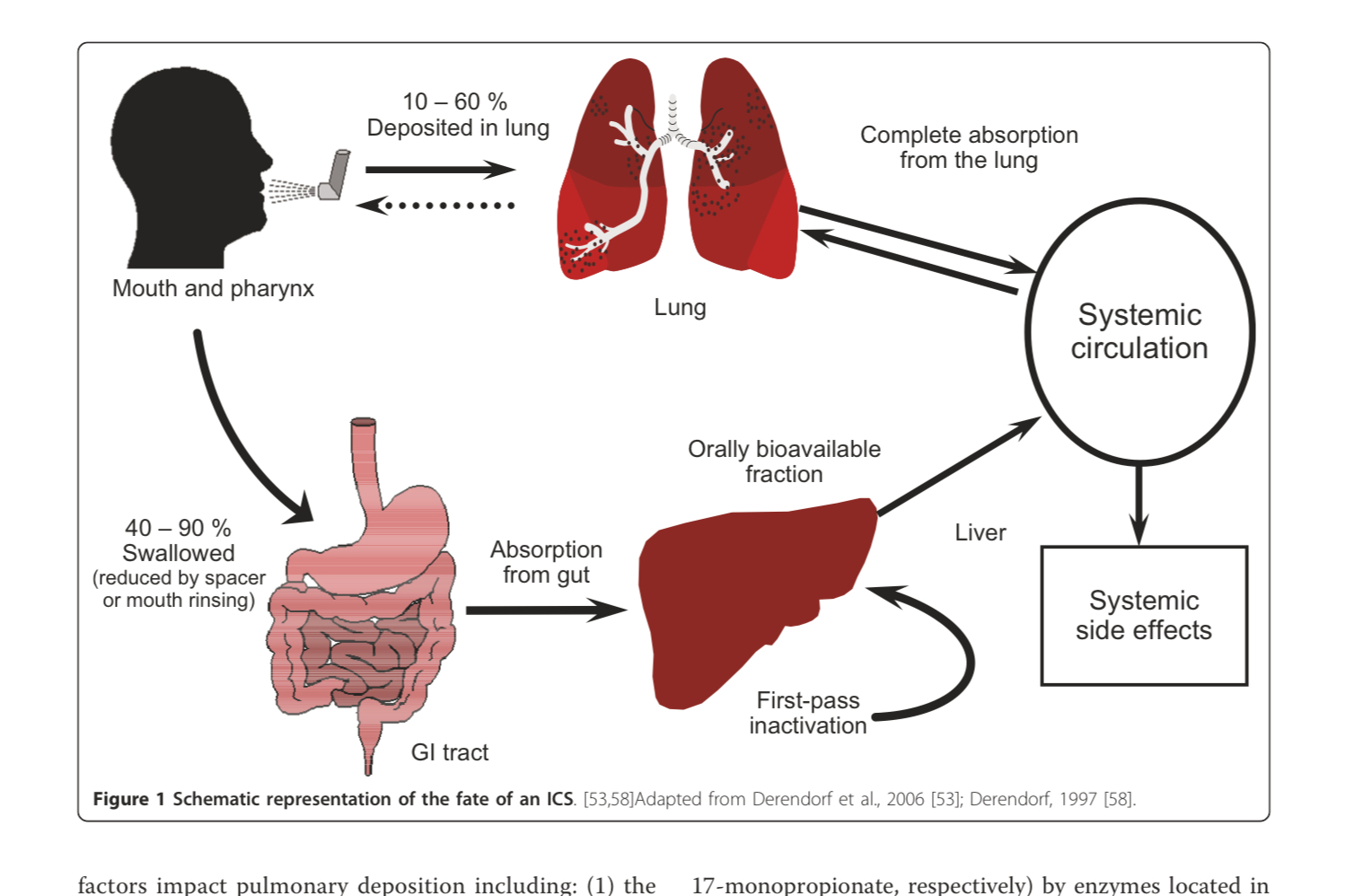
- Q. What percentage of inhaled corticosteroids reaches the lung ?
- 10-60%
- Q.Is it orally absorbed into the GIT ?
- Yes
- A lot of this gets deposited into the oropharynx
- If not rinsed- it may be absorbed into the oral tract
- Q. Does the user of spacer help ?
- Yes
- The spacer reduces the oropharyngeal deposition
- Q. inhaled corticosteroids has low oral bioavailiblity- is this good or bad ?
- This is good
- Since we don't want it to be orally absorbed and have systemic effects
- Q. Which inhaled corticosteroids has highest lung deposition ?]
- Beclomethasone
- Q. And which has highest oral bioavailiblity ?
- Also Beclomethasone
- Q. What is the impact of the particular size ?
- Smaller particles (<1 μm) are likely to be deposited into the oropharynx, while very small particles (<1 μm) will either be deposited in the upper airways or, if drawn into the lower airways, will be exhaled.
- Larger particles (>5 μm) are likely to be deposited into the oropharynx.
- Beclomethasone and ciclesonide delivered by metered-dose inhaler (MDI) have the smallest particle sizes among the available ICS medications.
- Q. Does it have plasma protein binding ?
- Yes
- inhaled corticosteroids has good albumin binding which makes it inactive
- This is useful to reduce it's systemic side effects
- Q. Which type of drug interaction is particularly common with the use of inhaled corticosteroids ?
- Increase half life due to CYP3A4 inhibitors like itraconazole
- Concomitant administration of itraconazole and budesonide, for example, has been associated with a more than 4-fold increase in plasma concentrations of budesonide given by inhalation.
- The concomitant use of ritonavir and fluticasone has also been shown to greatly increase plasma fluticasone concentrations, leading to cases of Cushing's syndrome and AS.
- Q. Enlist all the potential drug interactions ?
- Ketoconazole: An antifungal medication often used to treat fungal infections.
- Itraconazole: Another antifungal agent.
- Clarithromycin: An antibiotic used to treat various bacterial infections.
- Erythromycin: A widely used antibiotic.
- Ritonavir: An antiretroviral drug often used in HIV/AIDS treatment.
- Indinavir: Also an antiretroviral medication.
- Nelfinavir: Another drug used for HIV/AIDS.
- Grapefruit Juice: Known to inhibit CYP3A4 enzymes, affecting the metabolism of various drugs.
- Diltiazem: A calcium channel blocker used for heart conditions and high blood pressure.
- Verapamil: Similar to Diltiazem, used for heart rhythm disorders, angina, and high blood pressure.
- Cimetidine: A medication used to treat heartburn and peptic ulcers.
- Fluconazole: An antifungal medication, less potent as a CYP3A4 inhibitor compared to Ketoconazole and Itraconazole.
- Q.Which inhaled corticosteroids produces the highest adrenal suppression ?
- Fluticasone
- Especially doses >500 mcg/day (>800 mcg in one meta-analysis)
- In a study using insulin tolerance test- 50% of the children had evidence of adrenal insufficiency upto 16 weeks after starting therapy
- Similar study using low dose ACTH stimulation test also found 40% children having adrenal suppression
- Also proven in meta-analysis
- Q. What makes fluticasone particularly nasty in terms of HPA axis suppression ?
- Long half life- 14 hours
- Strong binding affinity for glucocorticoid receptors (18 times binding)
- Q. Is there a difference between fluticasone furoate and fluticasone propionate ?
- Fluticasone furoate has a longer retention time in respiratory tissues compared to fluticasone propionate, which likely leads to lower levels of systemic absorption and less impact on the hypothalamic-pituitary-adrenal axis.
- Studies show that fluticasone furoate has lower risk of adrenal suppression and lower systemic exposure compared to fluticasone propionate, resulting in a lower effect on adrenal function.
- However, one study showed that systemic exposure and risk of adrenal suppression to fluticasone furoate may be higher in people of East Asian descent.
- Overall, while not completely risk-free, studies suggest fluticasone furoate likely poses a lower risk of adrenal suppression and systemic side effects than fluticasone propionate, especially at equivalent doses. Careful monitoring is still required.
- Q. What doses of budesonide produces adrenal supression ?
- Doses >1000 mcg/day produces adrenal suppression
- Doses <400 mcg/day generally does not produce any adrenal issues
- Q. Which agent produces almost no adrenal suppression ?
- Ciclesonide
- Q. Why does Ciclesonide produce less HPA axis suppression ?
- Ciclesonide itself has low glucocorticoid receptor binding activity, but is converted by esterases in the lung to its active metabolite desisobutyryl-ciclesonide.
- Desisobutyryl-ciclesonide undergoes high rates of serum protein binding, reducing its biological availability.
- The active metabolite also undergoes extensive clearance from the circulation by the liver, lowering systemic exposure.
- These pharmacokinetic properties limit ciclesonide's systemic availability and reduce its systemic bioactivity, resulting in less HPA axis suppression.
- Studies demonstrate lower rates of HPA axis suppression, as measured by things like early morning cortisol, ACTH levels, and ACTH stimulation tests compared to other inhaled corticosteroids.
- However, while less suppressive than many other options, cases of adrenal insufficiency have still been associated with ciclesonide use indicating it is not risk-free and monitoring is still required.
- Q. Which two groups of patients with respiratory diseases are particularly venerable to HPA axis involvement ?
- Those with cystic fibrosis
- ABPA - allergic bronchopulmonary aspergillosis particularly due to antifungal use
- Q. According to UK guidelines which children should be screened for HPA axis ?
- Children receiving fluticasone >400 mcg/day should be screen for their HPA axis involvement
- Q. Based on the review article by Ahmet et akl which patients are recommended screening for the HPA axis ?
- Patient has persistent symptoms of AS: Weakness/fatigue, malaise, nausea, vomiting, diarrhea, abdominal pain, headache (usually in the morning), poor weight gain, myalgia, arthralgia, psychiatric symptom, poor growth, hypotension hypoglycemia
- Patient has >1000 g/day of budesonide/beclomethasone;
- Patient has received oral corticosteroids for: >2 consecutive weeks or >3 cumulative weeks in the last 6 months
- Patient using concomitant ICS therapy and potent CYP3A4 inhibitors, particularly antiretroviral and antifungal agents
- Q. According to the paper, what should be the protocol for screening such children ?
- Q. While screening should inhaled corticosteroids be stopped ?
- No. inhaled corticosteroids may be continued
- But oral corticoidsteroids need to be stopped 24 hours prior to testing
- Q. How frequent should be the follow-up ?
- Atleast once every 6 months
- Topical corticosteroids and adrenal suppression
- Q. What are the indications for topical corticosteroids in adults and children ?
-
For Adults:
- Eczema: Including atopic dermatitis and contact dermatitis.
- Psoriasis: To reduce inflammation and suppress the rapid skin cell growth.
- Lichen Planus: To relieve itching and reduce lesions.
- Discoid Lupus Erythematosus: For reducing inflammation and skin lesions.
- Seborrheic Dermatitis: To reduce flakiness and inflammation.
-
For Children:
- Eczema: Especially atopic dermatitis, commonly in children.
- Psoriasis: In mild to moderate cases.
- Diaper Rash: If associated with significant inflammation.
- Insect Bites: To reduce itching and swelling.
-
Common for Both Adults and Children:
- Allergic Reactions: Including those to poison ivy or other allergens.
- Inflammatory Skin Conditions: Such as dermatitis.
- Pruritus: Generalized itching, which may be due to various underlying conditions.
-
- Q. What are low, high and medium potency corticosteroids ?
-
Low Potency Corticosteroids:
- Examples: Hydrocortisone 1%, Desonide 0.05%.
- Uses: Typically used for sensitive areas like the face, skin folds, and in children.
- Indications: Treat mild to moderate non-facial dermatoses, diaper rash, and other sensitive skin conditions.
-
Medium Potency Corticosteroids:
- Examples: Triamcinolone acetonide 0.1%, Mometasone furoate 0.1%.
- Uses: Suitable for moderate dermatoses on the trunk and extremities.
- Indications: Used for more severe dermatitis, eczema, and non-facial psoriasis.
-
High Potency Corticosteroids:
- Examples: Clobetasol propionate 0.05%, Betamethasone dipropionate 0.05%.
- Uses: Reserved for severe dermatoses, particularly those unresponsive to medium potency steroids.
- Indications: Severe psoriasis, severe atopic dermatitis, discoid lupus, and other resistant conditions.
-
- Q. Does the use of Topical corticosteroids in atopic dermatititis in children lead to adrenal suppression ?
- A meta-analysis was conducted by Heickman et al:
- Meta-analysis of pediatric clinical trials on topical corticosteroid (TCS) use for atopic dermatitis found a low rate of hypothalamic-pituitary-adrenal (HPA) axis suppression, with 3.8% of participants experiencing HPA axis suppression.
- The prevalence of HPA axis suppression varied based on the potency of the TCS used, with low-potency TCS having a 2% suppression rate, medium-potency TCS having a 3.1% suppression rate, and high-potency TCS having a 6.6% suppression rate.
- The study concluded that mid- to low-potency TCS use is rarely associated with clinically significant adrenal insufficiency or adrenal crisis in pediatric patients.
- Severe systemic effects, such as adrenal insufficiency, Cushing syndrome, and adrenal crisis, have been reported in young children following prolonged or inappropriate use of very-high-potency TCS.
- The analysis included studies with a duration of 2 to 4 weeks and participants aged between 3 months and 18 years. All studies were prospective, open-label cohort studies
- A meta-analysis was conducted by Heickman et al:
- Q. Which situations lead to increase risk of HPA axis suppression with topical glucocorticoid use ?
- Situations that can lead to an increased risk of HPA axis suppression with topical glucocorticoid use include:
-
- Skin inflammation: Inflamed skin can have an impaired barrier function, which can increase the rate of systemic absorption of the glucocorticoid.
-
- Damage to the skin barrier: Any damage to the skin, such as cuts or wounds, can increase the absorption of the glucocorticoid into the bloodstream.
-
- Use of occlusive dressings: Occlusive dressings, such as bandages or plastic wrap, can enhance the absorption of the glucocorticoid through the skin.
-
- Site of application: The rate of systemic absorption can vary depending on the site of application. For example, percutaneous absorption is higher through mucous membranes, eyelids, and scrotum. It is important to note that short-term administration of topical glucocorticoids at recommended dosages is generally considered safe.
- Q. What is the difference in flourinated vs non florinated glucorticoids for topical preprations ?
-
Fluorinated Topical Glucocorticoids
- Examples: Dexamethasone, Triamcinolone Acetonide, Betamethasone, Beclomethasone.
- Skin Penetration: Better skin penetration compared to non-fluorinated steroids.
- Local Complications: More likely to produce local complications.
- Systemic Absorption and Side Effects: Associated with a greater risk of systemic absorption and side effects.
- Adverse Effects (AEs): Frequent local adverse effects include atrophy, striae, rosacea, perioral dermatitis, acne, and purpura. Less common effects include hypertrichosis, pigmentation alterations, delayed wound healing, and exacerbation of skin infections. Systemic reactions like hyperglycemia, glaucoma, and adrenal insufficiency are less frequent.
-
Non-Fluorinated Topical Glucocorticoids
- Example: Hydrocortisone.
- Skin Penetration: Less skin penetration compared to fluorinated steroids.
- Local Complications: Generally, fewer local complications.
- Systemic Absorption and Side Effects: Lower risk of systemic absorption and side effects compared to fluorinated steroids.
-
- Q. What are the local adverse effects of topical corticosteroids ?
- Atrophy: Thinning of the skin.
- Striae: Stretch marks.
- Rosacea: A condition characterized by redness and visible blood vessels in the face.
- Perioral Dermatitis: A rash around the mouth.
- Acne: Skin condition causing pimples.
- Purpura: Purple-colored spots and patches on the skin.
- Less Common Effects:
- Hypertrichosis: Excessive hair growth.
- Pigmentation Alterations: Changes in skin color.
- Delayed Wound Healing: Slower recovery of skin integrity after injury.
- Exacerbation of Skin Infections: Increased risk or severity of skin infections.
- Q. Can the use of topical steroids lead to fatal consequences ?
- There has been a reported case of an infant's death due to a generalized CMV (Cytomegalovirus) infection following the administration of topical GCs.
- Q. What are the dosage guidelines for the use of topical corticosteroids in children ?
- It is suggested that infants require about one-fifth of the adult dose of topical GCs,
- children require two-fifths
- adolescents two-thirds of the adult dose, based on their body surface area
- Ophthalmic preparation and corticosteroids
- Q. Does the use of opthalmic corticosteroids lead to HPA axis suppression ?
- A study by Sukhpal et al found no evidence that patients using continuous long-term corticosteroid eye drops after Post keratoplasty experienced inadequate adrenal response, and did not find any evidence of a negative correlation between length of treatment and SST or LDSST measurements at baseline
- Intra-articular glucocorticoid use
- Q. Give me some pointers towards HPA axis suppression with intra-articular glucorticoid use ?
- There is no doubt that there is systemic absorption that happens with intra-articular glucorticoid use
- However, the exact evidence for the same is lacking
- This may last for 2-3 months after the injection
- It is more in cases of inflammatory arthropathies especially in children since the area is highly vascular
- Q. How common is adrenal suppression seen with these agents ?
- In patients with osteoarthritis of the knee, the HPA axis suppression was seen after 4 weeks with
- methylprednisolone 25% of the cases
- betamethasone 5% of cases
- In another study 60% of cases had asymptomatic HPA axis involvement with bilateral intra-articular glucorticoid injection
- In patients with osteoarthritis of the knee, the HPA axis suppression was seen after 4 weeks with
- Q. Do epidural glucorticoid injection also produce the same ?
- Yes
- Q. Which intra-articular glucocorticoid has less systemic absorption ?
- Triamcinolone hexacetonide has less systemic absorption compared to other intra-articular steroid injections
- It is available in India as Kencort Hexa injection

- Other forms of non-systemic glucocorticoid use
- Q. What are the uses of intranasal corticosteroids ?
- Intranasal corticosteroids, used primarily for treating allergic rhinitis and nasal polyposis in both adults and children.
- Q. Which are the various generations of intranasal corticosteroids ?
- First Generation:
- These include older corticosteroids such as beclomethasone dipropionate and flunisolide. They were effective but had a higher potential for systemic side effects due to less favorable pharmacokinetics.
- Second Generation:
- This generation includes drugs like fluticasone propionate, mometasone furoate, and budesonide. These corticosteroids have a lower bioavailability and higher topical potency, reducing the risk of systemic side effects. They are often preferred due to their improved safety profile.
- Third Generation:
- This category, although sometimes debated, can include newer formulations or derivatives of second-generation drugs, such as fluticasone furoate. These newer formulations may offer advantages such as an improved side effect profile, more effective relief of symptoms, or more convenient dosing schedules.
- First Generation:
- Q. Does intranasal use of corticosteroid lead to adrenal suppression ?
- According to review by Boner et al (see reference below) "There is o effects on the HPA axis were detected in either children or adults with intranasal corticosteroid use"
- According to a meta-analysis by Samperi et al "The use of intranasal corticosteroids (INCS) carries a low risk for hypothalamic-pituitary-adrenal axis dysfunction and adrenal insufficiency (AI). The pooled percentage of AI for routinely utilized first- and second-generation INCS was 0.70% (95% CI, 0.29-1.12%)"
- Q. Which generation produces less HPA axis supression ?
- The newer generation intranasal steroid produces less HPA Axis suppression compared to older generation
- Q. Does the use of oral budesonide use in inflammatory bowel disease lead to HPA axis suppression ?
- oral budesonide, which is frequently used to treat inflammatory bowel disease, can be absorbed systemically and has been associated with cases of adrenal crisis and Cushing's syndrome.
- Clinical aspects of Glucocorticoid induced adrenal insufficiency
- Q. Do all patients with biochemically positive for adrenal insufficiency due to glucocorticoids also have symptoms of adrenal insufficiniency ?
- No
- In a study conducted- only 2 % patients had symptoms of adrenal insufficiency while 19% tested positive for Adrenal insufficiency biochemically
- Q. Can adrenal insufficiency due to inhaled corticosteroids use lead to death ?
- Yes
- several cases of death also have been reported
- Q. What are the usual doses of fluticasone propionate ?
- For Asthma:
- Adults and Adolescents (12 years and older):
- The typical dose ranges from 88 to 880 micrograms (mcg) per day, usually divided into two doses.
- Children (4-11 years old):
- Commonly, the dose is 88 mcg twice a day.
- Adults and Adolescents (12 years and older):
- For Chronic Obstructive Pulmonary Disease (COPD):
- The typical dose for adults is 250 to 500 mcg twice a day.
- For Asthma:
- Q. Of these what doses are associated with adrenal insufficiency ?
- Doses >500 mcg/day as suggested earlier
- Q. What are the usual symptoms of iatrogenic adrenal insufficiency ?
- General malaise
- Fatigue
- Weakness
- Dizziness (including postural dizziness)
- Gastrointestinal symptoms (nausea, vomiting, diarrhea, cramps, loss of appetite)
- Weight loss
- Hypotension (including postural hypotension)
- Headaches (usually in the morning)
- Arthralgias (especially in hand joints)
- Myalgias
- Recurrent respiratory infections with slow recovery
- Alabaster-like, pale skin
- Poor linear growth (children)
- Poor weight gain (children)
- Hypoglycemia (more frequent in children)
- Hyponatremia
- Lymphocytosis and eosinophilia
- Q. What are the clinical features of iatrogenic cushing's syndrome ?
- • Proximal muscle weakness
- • Weight gain and central obesity
- • Disproportionate supraclavicular and dorsocervical fat pads
- • Facial and upper neck plethora
- Facial rounding
- • Skin atrophy, easy bruising, red stretch marks
- • Acne
- • Poor wound healing
- • Insomnia
- • Increased appetite
- • Irritability, impaired memory, depression
- • Hypertension
- • Abnormal glucose metabolism
- • Menstrual irregularities (women)
- • Poor linear growth (children)
- Q. What are the symptoms of adrenergic crisis ?
- Cushing's syndrome can develop adrenal crisis. Patients present with at least two of the following:
- Hypotension or hypovolemic shock
- • Nausea or vomiting
- Severe fatigue
- Fever with Impaired consciousness (including lethargy, confusion, somnolence, collapse, delirium, coma, seizures)
- Patients can also present with laboratory abnormalities (hypoglycemia, hyponatremia, lymphocytosis, eosinophilia).
- Q. What are the conditions that can precipitate adrenergic crisis ?
- • Infections (including gastrointestinal infections, respiratory infections, sepsis)
- • Surgery
- • Acute illness
- • Fever
- • Severe stress and pain (including severe anxiety, bereavement)
- • Physical trauma
- • Strenuous exercise
- • Dental procedures
- Labor and delivery
- • Abrupt glucocorticoid withdrawal
- • Glucocorticoid tapering below replacement doses
- • Switch between different types and doses of inhaled glucocorticoids
- • Initiation of a cytochrome P450 3A4 inducer
- Q. Glucorticoids given during what period does not need taper ?
- Glucorticoid given <2 weeks does not need tapering
- Q. What is glucocorticoid withdrawal syndrome ?
- GWS is a withdrawal reaction that may occur during the glucocorticoid taper owing to developed dependence on supraphysiological glucocorticoid concentrations
- The pathophysiology of GWS is multifactorial and is likely mediated by suppressed corticotropin releasing hormone, central noradrenergic and dopaminergic system, decrease in pro-opiomelanocortin related peptides due to chronic suppression of HPAA, and the increase in cytokines (interleukin 6, tumor necrosis factor α) and prostaglandins.
- Symptoms of GWS may include anorexia, nausea, emesis, lethargy, somnolence, arthralgia, myalgia, low-grade fever, postural hypotension, and psychiatric symptoms (mainly depression, anxiety, and panic attacks)
- GWS may last months, and patients report poor quality of life and wellbeing. GWS is under-recognized as a separate entity, partly because of overlap of GWS symptoms with those of adrenal insufficiency and possibly the underlying disorder glucocorticoids were initially prescribed to treat.
- Assessment of the severity of GWS during glucocorticoid taper is important for proper management.
- Q. What is the biggest advantage of using hydrocortisone while tapering glucocorticoids compared to prednisolone ?
- the recovery of HPA axis occurs faster with hydrocortisone
- However this is based on low quality evidence
- Q. When should you start assessing for HPA axis recovery while tapering glucorticoids ?
- Only when the predinolone doses are 5 mg or lower
- It is unlikely to occur for patient on dexamethasone so we should not bother
- Q. Summarize the approach to glucorticoid taper as addressed in the article by Prete et al ?
- Patient Education
- Symptoms and Management of GWS:
- Education on identifying and managing symptoms related to Glucocorticoid Withdrawal Syndrome (GWS).
- Symptoms and Management of GI-AI:
- Information on the symptoms and management of Glucocorticoid-Induced Adrenal Insufficiency (GI-AI).
- Symptoms and Management of GWS:
- Provider Education
- Recommendations for Medical Record:
- Documenting written recommendations in the patient’s medical record.
- Providing a letter on the management of glucocorticoid and adrenal insufficiency.
- Recommendations for Medical Record:
- Considerations for Glucocorticoid Taper
- Factors to Consider:
- Duration of glucocorticoid use and average dose
- Previous experiences with glucocorticoid tapering.
- Patient's functional status.
- Risk of relapse of the underlying disorder requiring glucocorticoid therapy.
- Avoidance of glucocorticoid administration in the afternoon/evening.
- Initial Rapid Glucocorticoid Taper:
- For patients on an average daily dose Prednisolone (PED) >40 mg: Decrease by 5-10 mg weekly until PED reaches 20 mg.
- For PED 20-40 mg: Decrease by 5 mg weekly until PED reaches 20 mg.
- For PED 10-20 mg: Proceed to slow taper recommendations.
- Switching twice-a-day or evening doses of predniso(lo)ne to once a day in the morning.
- For dexamethasone users, switch to an equivalent dose of predniso(lo)ne.
- Subsequent Slow Glucocorticoid Taper:
- For PED 10-20 mg: Decrease by 1-2.5 mg weekly until 10 mg. Consider bi-monthly decrements for severe GWS.
- For PED 5-10 mg: Decrease by 1 mg weekly until 5 mg. Consider bi-monthly or monthly decrements for severe GWS.
- For PED 5 mg: Do not decrease until HPAA recovery is documented. Consider switching to hydrocortisone (20 mg) if recovery is delayed.
- Factors to Consider:
- Assessment of HPAA Recovery
- Timing: After reaching PED 5 mg or a replacement dose of hydrocortisone for 1-4 weeks.
- Frequency: Every 2-3 months; if not recovered in 1-2 years, then every 3-6 months.
- Testing: Morning serum cortisol and additional tests if needed (e.g., Synthetic ACTH stimulation test, overnight metyrapone test, insulin tolerance test).
- Management of Patients with Established GC-AI (Refer to Fig 2)
- Physician Responsibilities:
- Periodic clinical and biochemical assessment.
- Ensuring adequate supply of oral and injectable glucocorticoids.
- Counseling on therapy, special situations (e.g., shift work, pregnancy), and sick day rules.
- Patient Responsibilities:
- Adhering to chronic glucocorticoid replacement therapy (e.g., hydrocortisone or predniso(lo)ne).
- Following sick day rules (e.g., doubling/tripling oral dose during illness, self-injecting in severe cases).
- Wearing medical alert identification.
- Carrying a steroid card/letter outlining management.
- Becoming comfortable with GC-AI management and practicing glucocorticoid injections.
- Communicating with the medical team regarding GC-AI.
- Physician Responsibilities:
- Patient Education
- Q. What single cortisol level is a good assuring sign of recover of the HPA axis ?
- Cortisol >10 mcg/dl as per a recent study
- Q. Is it possible that patients never have recovery of the HPA axis ?
- Yes
- This has been reported in about 5% of cases
- In some cases it has the it may remain for >3 years
- Q. Does the use of the commonly used inhaled corticosteroids cross react with cortisol immunoassay ?
- According to a study by Stokes et al:
- "The cross-reactivity of the inhaled steroids; betamethasone, fluticasone and beclomethasone in the Roche cortisol immunoassay are unlikely to be clinically significant at the concentrations found in patients on therapeutic doses. This will enable confident assessment of adrenal status in patients at risk of adrenal suppression."
- According to a study by Stokes et al:
References:
- Ahmet A, Kim H, Spier S. Adrenal suppression: A practical guide to the screening and management of this under-recognized complication of inhaled corticosteroid therapy. Allergy Asthma Clin Immunol. 2011 Aug 25;7(1):13. doi: 10.1186/1710-1492-7-13. PMID: 21867553; PMCID: PMC3177893.
- Boner AL. Effects of intranasal corticosteroids on the hypothalamic-pituitary-adrenal axis in children. Journal of allergy and clinical immunology. 2001 Jul 1;108(1):S32-9.
- Sampieri G, Namavarian A, Lee JJ, Hamour AF, Lee JM. Hypothalamic‐pituitary‐adrenal axis suppression and intranasal corticosteroid use: a systematic review and meta‐analysis. InInternational Forum of Allergy & Rhinology 2022 Jan (Vol. 12, No. 1, pp. 11-27).
- Lauren, K., Wood, Heickman., Ladan, Davallow, Ghajar., Mark, R., Conaway., Alan, D., Rogol. (2018). Evaluation of Hypothalamic-Pituitary-Adrenal Axis Suppression following Cutaneous Use of Topical Corticosteroids in Children: A Meta-Analysis.. Hormone Research in Paediatrics, 89(6):389-396. doi: 10.1159/000489125
- Sukhpal, S., Sandhu., J, M, Smith., M, Doherty., Andy, James., Francisco, C, Figueiredo. (2012). Do topical ophthalmic corticosteroids suppress the hypothalmic-pituitary-adrenal axis in post-penetrating keratoplasty patients?. Eye, 26(5):699-702. doi: 10.1038/EYE.2012.12
- Prete A, Bancos I. Glucocorticoid induced adrenal insufficiency. Bmj. 2021 Jul 12;374.
- Stokes F, Bailey L, Ganguli A, Davison A. Assessment of endogenous, oral and inhaled steroid cross-reactivity in the Roche cortisol immunoassay. Annals of Clinical Biochemistry: International Journal of Laboratory Medicine. 2013; 51(4):503-506. DOI: 10.1177/0004563213509793.