What is the role of MRI in Thyroid-Associated Orbitopathy (TAO) ?
Created/Updated: #jan2025
Research by : Perplexity
Edited by: Dr. Om J Lakhani
Q. What is the role of MRI in diagnosing thyroid-associated orbitopathy (TAO)?
- MRI provides high soft-tissue contrast and multiplanar imaging, making it ideal for TAO diagnosis.
- It helps differentiate TAO from other orbital pathologies.
Q. What are the characteristic MRI findings in TAO?
- Thyroid-associated orbitopathy (TAO) presents several characteristic features on magnetic resonance imaging (MRI) that are crucial for diagnosis, assessment of disease activity, and management. These features can be observed in various orbital structures and are best appreciated using specific MRI sequences.
-
Extraocular Muscle Changes
- The most prominent and consistent finding in TAO is the involvement of extraocular muscles:
- Muscle Enlargement:
- Typically symmetrical and bilateral, though asymmetry can occur.
- The inferior and medial rectus muscles are most commonly affected, followed by the superior and lateral rectus.
- Characteristic "tendon-sparing" pattern: the muscle belly enlarges while the tendinous insertion remains normal in size.
- Signal Intensity Changes:
- On T2-weighted images, active inflammation is characterized by increased signal intensity within the muscles.
- T1-weighted images show isointense or slightly hyperintense signal in the affected muscles.
-
Orbital Fat Changes
- Volume Increase:
- Expansion of the orbital fat compartment is a common finding.
- This contributes to increased orbital volume and can lead to proptosis.
- Signal Characteristics:
- Orbital fat typically shows high signal intensity on both T1 and T2-weighted images.
- Volume Increase:
-
Lacrimal Gland Involvement
- Enlargement of the lacrimal gland is observed in some cases.
- Signal intensity changes similar to those in extraocular muscles may be present.
-
Optic Nerve Changes
- Optic Nerve Compression:
- In severe cases, crowding at the orbital apex can lead to optic nerve compression.
- This is best visualized on coronal images.
- Optic Nerve Stretching:
- Increased orbital content can cause straightening and stretching of the optic nerve.
- Optic Nerve Compression:
-
Orbital Apex Crowding
- Enlargement of extraocular muscles at the orbital apex can lead to crowding.
- This is a critical finding as it may precede the development of dysthyroid optic neuropathy.
-
Proptosis
- Forward displacement of the globe relative to the interzygomatic line.
- Quantifiable on MRI, providing an objective measure of exophthalmos.
-
Specific MRI Sequences and Their Utility
- T2-weighted Imaging:
- Crucial for assessing disease activity.
- Active inflammation appears as high signal intensity within the muscles.
- T1-weighted Imaging:
- Useful for anatomical delineation and fat visualization.
- STIR (Short TI Inversion Recovery):
- Enhances the visibility of edema and inflammation in muscles.
- Diffusion-Weighted Imaging (DWI):
- Can provide additional information on disease activity through apparent diffusion coefficient (ADC) values.
- Dynamic Contrast-Enhanced MRI:
- May be used to assess orbital blood flow and inflammation.
- In conclusion, MRI provides a comprehensive evaluation of orbital changes in TAO, allowing for accurate diagnosis, assessment of disease activity, and monitoring of treatment response. The combination of muscle enlargement, signal intensity changes, and associated orbital findings forms a characteristic pattern that is highly suggestive of TAO when interpreted in the clinical context
- T2-weighted Imaging:
Q. How does MRI help assess disease activity in TAO?
- T2-weighted imaging:
- Increased signal intensity suggests active inflammation.
- Quantitative Techniques:
- T2 relaxometry and T2 mapping reflect inflammatory edema.
- Diffusion-weighted imaging (DWI) and ADC values help measure disease activity.
Q. What is the role of MRI STIR sequence in assessing disease activity in TAO ?
- According to a study done by Ge , Zhang et al: "the signal intensity of extraocular muscles on STIR sequence was a good predictor for TAO activity. A cut-off SIR value of > 2.9 in the inferior rectus could be applied to evaluate the active stage of TAO."
- Read more about the study here: MRI STIR sequence for Disease activity in TAO
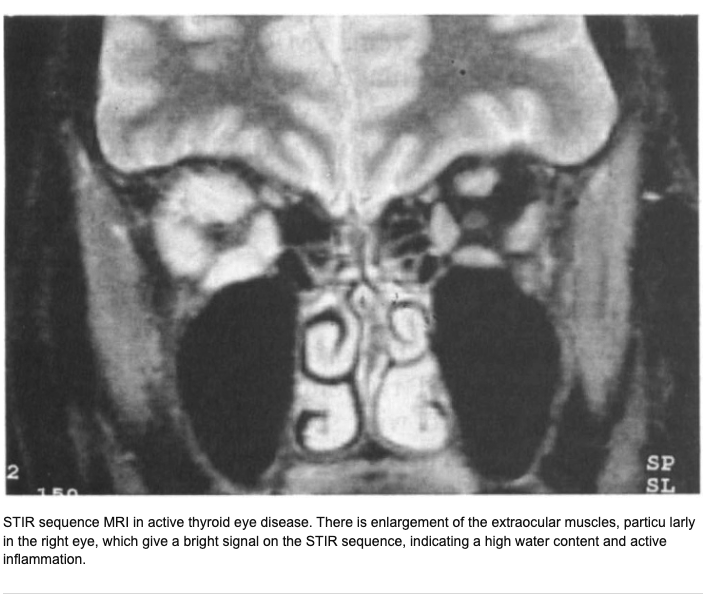
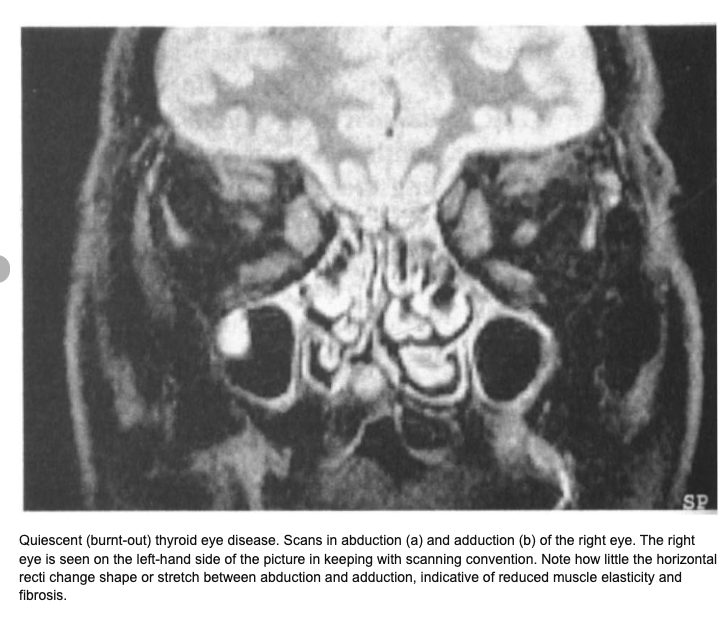
(Image source: Bailey CC, Kabala J, Laitt R, Goddard P, Hoh HB, Potts MJ, Harrad RA. Magnetic resonance imaging in thyroid eye disease. Eye (Lond). 1996;10 ( Pt 5):617-9. doi: 10.1038/eye.1996.140. PMID: 8977792.)
Q. Can MRI help to predict which patients are likely to respond to Glucorticoids in TAO ?
- According to a study published in 2024: "Serum cholesterol levels and orbital MRI parameters can serve as simple, effective predictors of glucocorticoid response in TED. Patients with lower total cholesterol and high EOM-SIRmin may benefit from glucocorticoid therapy"
- Read about the article here : Can you use MRI to predict response to steroid in TAO ?
Q. How does MRI assist in monitoring treatment response for TAO?
- Changes in muscle signal intensity and volume can be tracked.
- Reduction in T2 signal or ADC values indicates positive treatment response.
Q. Can MRI detect complications in TAO?
- Yes. Key complications detected include:
- Optic neuropathy: Apical crowding and optic nerve compression.
- Muscle fibrosis: Chronic cases may show fibrotic changes in extraocular muscles.
Q. Is MRI useful for surgical planning in TAO?
- Yes. MRI provides detailed anatomical visualization critical for orbital decompression surgery planning.
Q. How does MRI compare to CT in TAO evaluation?
- MRI Advantages:
- No ionizing radiation (safe for repeated use).
- Superior soft-tissue contrast.
- Better for detecting subtle inflammation.
- CT Advantages:
- Better for bony structures evaluation.
Conclusion:
- MRI is a powerful tool for diagnosing, monitoring, and managing TAO.
- It provides detailed, objective data to guide diagnosis, track disease activity, assess treatment response, and aid surgical planning.